Hi. I’m Dr. Leslie Thomas, a nephrologist at Mayo Clinic, and I’m here to shed light on the crucial process of diagnosing hypertension, often referred to as HTN. Understanding how hypertension is diagnosed is the first step towards managing this condition effectively and safeguarding your long-term health.
Hypertension, or high blood pressure, is a common condition where the force of blood against your artery walls is consistently too high. But how exactly is this diagnosis made? It’s not always as simple as a single high reading at the doctor’s office. Let’s delve into the methods and considerations involved in accurately diagnosing hypertension.
One of the foundational aspects of HTN diagnosis is measuring blood pressure accurately. This might seem straightforward, but several factors can influence blood pressure readings. To get a reliable picture of your blood pressure, healthcare professionals often recommend both in-office and home blood pressure monitoring.
When you visit your doctor, your blood pressure will be measured using a sphygmomanometer, typically on your upper arm. It’s important to ensure accuracy during this process. For the most reliable readings in a clinical setting, certain precautions are taken. You should be seated comfortably for at least five minutes before the measurement, with your feet flat on the floor and your arm supported at heart level. Avoid caffeine, smoking, and exercise for at least 30 minutes prior to the measurement as these can temporarily elevate blood pressure.
Accurate blood pressure measurement is crucial for diagnosing hypertension; a doctor uses a manual sphygmomanometer to ensure precision.
Interestingly, blood pressure can vary slightly between arms. If there’s a known difference, subsequent measurements should be taken on the arm with the higher readings to ensure consistency in monitoring.
Beyond the doctor’s office, home blood pressure monitoring plays an increasingly vital role in HTN diagnosis. It provides a broader picture of your blood pressure levels over time, minimizing the influence of “white coat hypertension,” where blood pressure is elevated in a medical setting but normal elsewhere.
For effective home monitoring, it’s essential to use a validated and properly calibrated blood pressure monitor. Calibration should be checked annually to maintain accuracy. Similar to in-office measurements, preparation is key at home. Rest for at least five minutes in a relaxed state, feet flat on the floor, legs uncrossed, and back supported. Support your arm on a flat surface at heart level. It’s recommended to take at least two readings, one minute apart, both in the morning before taking any medications and in the evening before your evening meal. Record these readings and share them with your doctor.
Home blood pressure monitoring allows for regular checks and helps in identifying trends over time, crucial for managing hypertension.
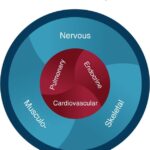
Sometimes, individuals experience erratic blood pressure, also known as labile blood pressure, characterized by sudden and significant fluctuations. Diagnosing the cause of labile blood pressure is crucial as it could indicate underlying health issues. Conditions such as heart problems, hormonal imbalances, neurological disorders, or even psychological factors can contribute to these fluctuations. If you experience such erratic readings, it’s important to discuss this pattern with your doctor to investigate potential underlying causes. Identifying and addressing the root cause can significantly stabilize blood pressure.
While blood pressure measurement is the cornerstone of diagnosis, it’s also important to understand that diagnosis is not solely based on a single high reading. Typically, hypertension diagnosis requires multiple elevated blood pressure readings taken on different occasions. This helps to rule out temporary elevations due to stress or other transient factors.
Furthermore, your doctor will consider your medical history and conduct a physical examination as part of the diagnostic process. They will inquire about family history of hypertension, lifestyle factors, and any existing medical conditions that might contribute to or be affected by high blood pressure. This comprehensive approach ensures an accurate diagnosis and helps tailor a management plan that’s right for you.
In conclusion, diagnosing hypertension is a multi-faceted process that involves accurate blood pressure measurement, often both in clinical and home settings. Understanding the proper techniques for blood pressure measurement, recognizing patterns like labile blood pressure, and consulting with your healthcare provider are all vital steps in getting an accurate diagnosis and taking proactive steps towards managing your health. Remember, early diagnosis and management are key to preventing the long-term complications of hypertension. If you have concerns about your blood pressure, don’t hesitate to reach out to your medical team for guidance and support.