Nursing diagnosis is a critical skill for every nurse. It’s the foundation upon which effective patient care plans are built. This guide will walk you through the essential concepts of nursing diagnosis, providing you with a clear understanding of what it is, its purpose, and, most importantly, how to formulate accurate and helpful nursing diagnoses.
Understanding Nursing Diagnosis
A nursing diagnosis is defined as a clinical judgment about a patient’s response to actual or potential health conditions or life processes. This response can be experienced by an individual, a family, a group, or a community. It’s not just about identifying a disease; it’s about understanding how that disease or health issue affects the patient’s life and well-being. This judgment provides the crucial basis for nurses to select specific nursing interventions that will lead to desired patient outcomes. Nurses are accountable for these outcomes, making accurate nursing diagnoses paramount.
Nursing diagnoses are derived from the comprehensive data gathered during the nursing assessment. This assessment process involves collecting subjective and objective data about the patient’s physical, psychological, social, and spiritual health. By analyzing this data, nurses can identify patterns and draw conclusions that form the basis of their nursing diagnoses, ultimately guiding the development of a tailored nursing care plan.
Why is Nursing Diagnosis Important?
Nursing diagnosis serves several vital purposes in healthcare:
- Enhances Critical Thinking and Problem-Solving: For nursing students, learning how to formulate nursing diagnoses is an excellent way to sharpen problem-solving and critical thinking skills. It encourages a systematic approach to patient care.
- Prioritizes Nursing Care: Nursing diagnoses help nurses identify the most pressing patient needs, allowing for the prioritization of nursing interventions. This ensures that the most critical issues are addressed promptly and effectively.
- Supports Quality Assurance and Reimbursement: Well-defined nursing diagnoses contribute to the formulation of measurable expected outcomes. These outcomes are essential for quality assurance requirements and are often necessary for third-party payers to justify reimbursement.
- Focuses on Patient Response: Nursing diagnoses emphasize understanding how a patient or group is responding to health challenges, whether actual or potential. This patient-centered approach also considers the patient’s strengths and resources that can be utilized in resolving or preventing problems.
- Facilitates Communication and Collaboration: By providing a common language, nursing diagnoses create a foundation for clear and effective communication among nursing professionals and the entire healthcare team. This shared understanding is crucial for coordinated patient care.
- Enables Evaluation of Nursing Care Effectiveness: Nursing diagnoses provide a benchmark for evaluation. By assessing patient outcomes related to the diagnosed problems, nurses can determine if the nursing care provided was beneficial and cost-effective.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems: Key Differences
It’s important to distinguish nursing diagnoses from medical diagnoses and collaborative problems. While all are crucial to patient care, they represent different aspects of healthcare.
- Nursing Diagnosis: Focuses on the patient’s response to a health condition. It’s about how the illness impacts the patient’s physical, emotional, and lifestyle aspects. Nurses are autonomous in addressing nursing diagnoses through independent nursing interventions. For instance, a patient with pneumonia (medical diagnosis) might have a nursing diagnosis of “Ineffective Airway Clearance” related to increased mucus production.
- Medical Diagnosis: Identifies the disease or pathological condition. This is made by a physician or advanced practitioner and deals with what only medical professionals can treat, often focusing on pathology and cure. Examples include Diabetes Mellitus, Tuberculosis, or Hepatitis. Medical diagnoses guide medical treatment, including medication and surgical interventions.
- Collaborative Problems: These are potential or actual health complications that nurses monitor and manage in collaboration with physicians. They require both physician-prescribed and independent nursing interventions. The nursing focus is on monitoring for changes in patient status and preventing potential complications. For example, a patient post-surgery is at risk for a collaborative problem like “Potential Complication: Hemorrhage,” where nurses monitor for bleeding and implement physician-ordered interventions if it occurs.
In essence, nursing diagnoses are patient-centered and focus on care, medical diagnoses are disease-centered and focus on cure, and collaborative problems are complication-focused and require interdisciplinary management.
Understanding Nursing Diagnosis Classifications: Taxonomy II
To standardize and organize nursing diagnoses, classification systems like Taxonomy II are used. Adopted in 2002 and based on Dr. Mary Joy Gordon’s Functional Health Patterns, Taxonomy II provides a hierarchical structure.
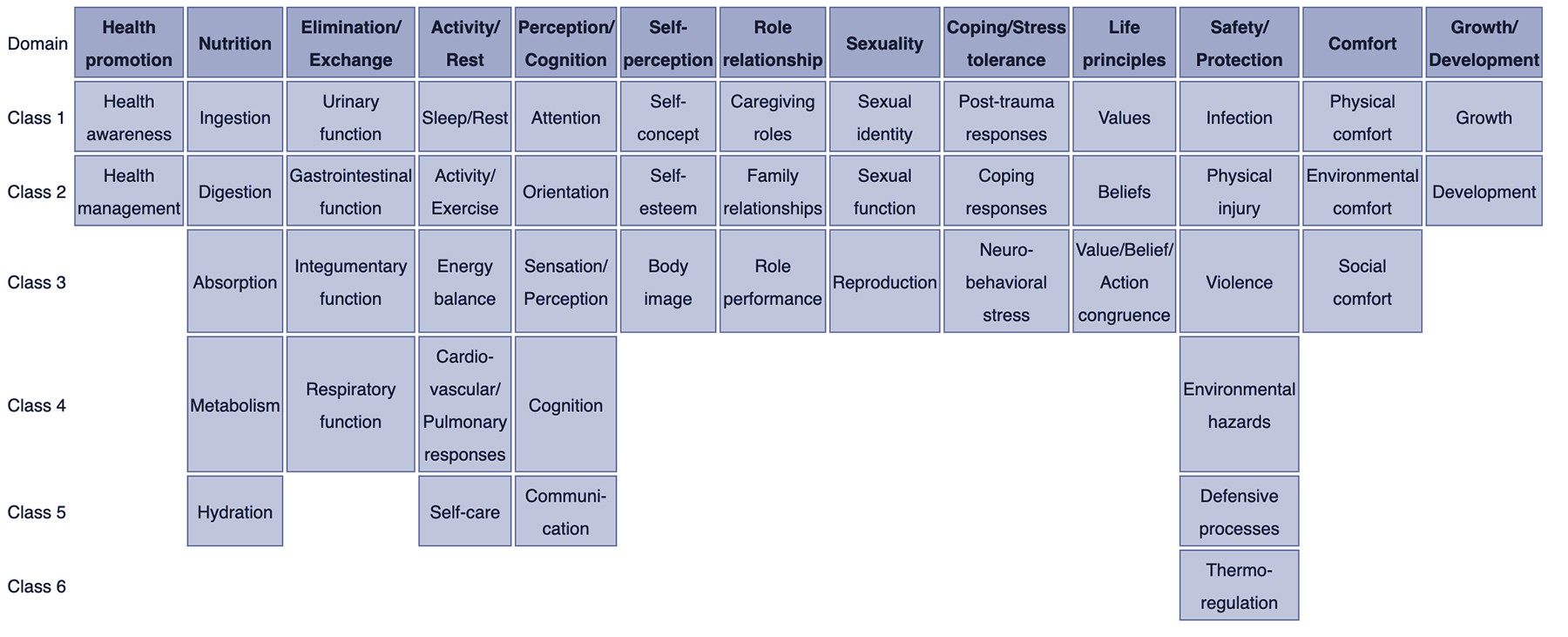
NURSING DIAGNOSIS TAXONOMY II. Taxonomy II for nursing diagnosis contains 13 domains and 47 classes. Image via: Wikipedia.com
Taxonomy II is organized into three levels:
- Domains (13): Broad categories of human health. Examples include Health Promotion, Nutrition, Elimination and Exchange, Activity/Rest, Perception/Cognition, Self-Perception, Role Relationship, Sexuality, Coping/Stress Tolerance, Life Principles, Safety/Protection, Comfort, and Growth/Development.
- Classes (47): Subcategories within each domain, providing more specific groupings. For example, within the domain “Nutrition,” classes include Ingestion, Digestion, Absorption, Metabolism, and Hydration.
- Nursing Diagnoses: Specific diagnostic labels are listed within each class. These are the standardized terms nurses use to identify patient problems.
Diagnoses in Taxonomy II are coded according to seven axes, including diagnostic concept, time, unit of care, age, health status, descriptor, and topology. Importantly, diagnoses are listed alphabetically by concept, not the first word, making them easier to locate within the taxonomy.
Examples of Domains and Classes:
- Domain 1. Health Promotion:
- Class 1. Health Awareness
- Class 2. Health Management
- Domain 2. Nutrition:
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Domain 3. Elimination and Exchange:
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Domain 4. Activity/Rest:
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Domain 5. Perception/Cognition:
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Domain 6. Self-Perception:
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Domain 7. Role relationship:
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Domain 8. Sexuality:
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Domain 9. Coping/stress tolerance:
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Domain 10. Life principles:
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Domain 11. Safety/Protection:
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Domain 12. Comfort:
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Domain 13. Growth/Development:
- Class 1. Growth
- Class 2. Development
The Nursing Process and Nursing Diagnosis
Nursing diagnosis is the second step in the nursing process, a systematic approach to patient care. The five stages of the nursing process are:
- Assessment: Gathering subjective and objective data about the patient.
- Diagnosis: Analyzing assessment data to identify nursing diagnoses.
- Planning: Developing a care plan with specific goals and nursing interventions to address the diagnoses.
- Implementation: Putting the care plan into action.
- Evaluation: Assessing the effectiveness of the interventions and the patient’s progress toward goals.
Each step of the nursing process requires critical thinking. For nursing diagnosis specifically, nurses need to understand definitions, recognize defining characteristics and related factors, and link diagnoses to appropriate interventions.
For a deeper understanding of the nursing process, refer to: “The Nursing Process: A Comprehensive Guide“
Types of Nursing Diagnoses: Which One to Use?
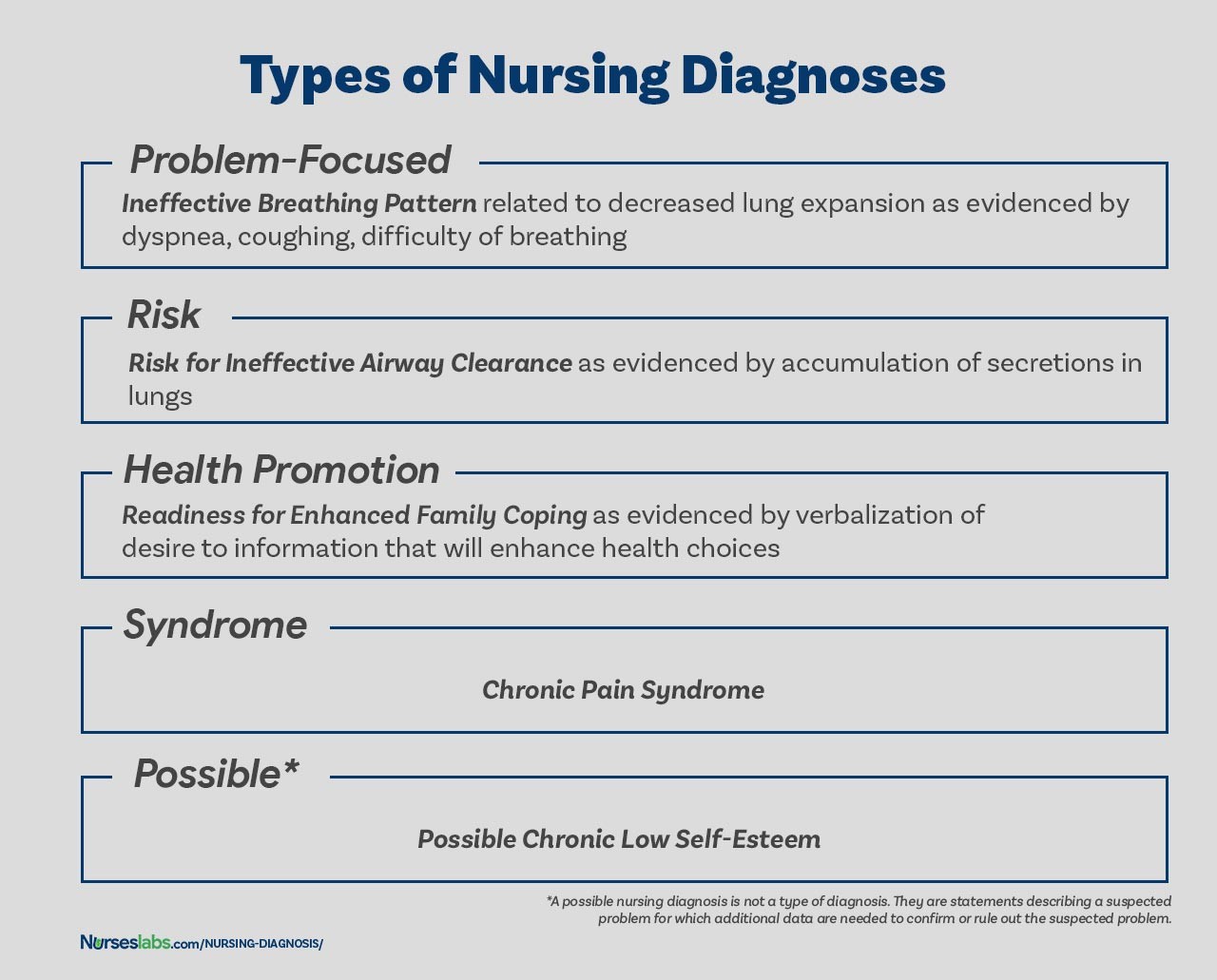
There are four main types of nursing diagnoses, each serving a distinct purpose:
TYPES OF NURSING DIAGNOSES. The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion, and Syndrome.
1. Problem-Focused (Actual) Nursing Diagnosis
A problem-focused diagnosis, also known as an actual diagnosis, describes a problem that is currently present at the time of the nursing assessment. These diagnoses are supported by defining characteristics – the signs and symptoms the patient is exhibiting. It’s crucial to remember that actual diagnoses are not inherently more important than risk diagnoses; in many cases, a risk diagnosis might be a higher priority for preventative care.
Problem-focused diagnoses have three key components:
- Nursing Diagnosis Label: A standardized term for the problem (e.g., “Pain”).
- Related Factors: The “related to” factors that are causing or contributing to the problem (e.g., “related to surgical incision”).
- Defining Characteristics: The “as evidenced by” signs and symptoms that confirm the presence of the problem (e.g., “as evidenced by patient report of pain at incision site, guarding behavior, and elevated heart rate”).
Example: Acute Pain related to surgical incision as evidenced by patient report of pain at incision site, guarding behavior, and elevated heart rate.
2. Risk Nursing Diagnosis
Risk nursing diagnoses identify potential problems. They are clinical judgments that a problem does not currently exist, but risk factors indicate a problem is likely to develop without nursing intervention. Risk diagnoses are based on a patient’s current health status, medical history, and identified risk factors. They are vital for preventative care, allowing nurses to proactively address potential issues before they become actual problems.
Risk diagnoses have two components:
- Risk Diagnostic Label: A standardized term indicating a potential problem, starting with “Risk for” (e.g., “Risk for Infection”).
- Risk Factors: The “as evidenced by” factors that increase the patient’s vulnerability to the problem (e.g., “as evidenced by surgical wound, compromised immune system, and prolonged hospitalization”).
Example: Risk for Infection as evidenced by surgical wound, compromised immune system, and prolonged hospitalization.
It’s important to note that risk diagnoses do not include defining characteristics (signs and symptoms) because the problem is not yet present. Instead, “as evidenced by” links the diagnostic label to the risk factors.
3. Health Promotion Nursing Diagnosis
Health promotion diagnoses, sometimes called wellness diagnoses, focus on a patient’s desire and motivation to improve their well-being and health. They identify a patient’s readiness to engage in health-enhancing behaviors. For instance, a new mother eager to learn about breastfeeding might receive a health promotion diagnosis of “Readiness for Enhanced Breastfeeding.” These diagnoses guide interventions aimed at supporting the patient’s health goals and enhancing their current wellness level.
Health promotion diagnoses typically have one component:
- Diagnostic Label: A standardized term indicating a readiness to improve health (e.g., “Readiness for Enhanced Knowledge”).
Related factors can be added for clarity but are not always necessary, as the underlying factor is usually the patient’s motivation.
Example: Readiness for Enhanced Breastfeeding.
4. Syndrome Nursing Diagnosis
Syndrome diagnoses represent a cluster of actual or risk nursing diagnoses that are predicted to occur together due to a specific event or situation. They are also written as one-part statements, using only the diagnostic label. Syndrome diagnoses recognize patterns of problems that frequently co-occur.
Examples:
- Rape Trauma Syndrome
- Disuse Syndrome
- Relocation Stress Syndrome
5. Possible Nursing Diagnosis (Not a Type, but a Placeholder)
Possible nursing diagnoses are not a formal type like the other four. Instead, they are used to indicate a suspected problem where more data is needed to confirm or rule out the diagnosis. They are essentially placeholders, signaling to other nurses that a potential issue exists and further assessment is required.
Example: Possible Bowel Obstruction (needs further assessment to confirm or rule out).
Key Components of a Nursing Diagnosis Statement
A well-written nursing diagnosis statement typically includes three essential components:
- Problem (Diagnostic Label): A concise term describing the patient’s health problem or response.
- Etiology (Related Factors): The factors contributing to or causing the problem (for actual diagnoses).
- Defining Characteristics (Signs and Symptoms) or Risk Factors (for risk diagnoses): The evidence that supports the diagnosis.
1. Problem and Definition (Diagnostic Label)
The problem statement, or diagnostic label, is a standardized term from a nursing diagnosis taxonomy (like NANDA-I) that concisely describes the identified patient problem. It usually has two parts:
- Qualifier (Modifier): Words that add specific meaning or detail to the diagnosis (e.g., “Deficient,” “Impaired,” “Ineffective”).
- Focus of the Diagnosis: The area of health concern (e.g., “Fluid Volume,” “Gas Exchange,” “Tissue Perfusion”).
Some one-word diagnoses (e.g., Anxiety, Constipation) inherently combine the qualifier and focus.
| Qualifier | Focus of the Diagnosis | Example Nursing Diagnosis |
|---|---|---|
| Deficient | Fluid volume | Deficient Fluid Volume |
| Imbalanced | Nutrition: Less Than Body Requirements | Imbalanced Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange | Impaired Gas Exchange |
| Ineffective | Tissue Perfusion | Ineffective Tissue Perfusion |
| Risk for | Injury | Risk for Injury |
2. Etiology (Related Factors)
The etiology, or related factors, identifies the probable causes of the health problem for actual diagnoses. These factors are linked to the problem statement using the phrase “related to.” Identifying the etiology is crucial because nursing interventions should be directed at addressing these underlying causes to resolve the nursing diagnosis.
Example: Impaired Physical Mobility related to pain and stiffness. (Interventions would focus on pain management and improving joint mobility).
3. Risk Factors (For Risk Diagnoses)
For risk nursing diagnoses, risk factors replace etiology. Risk factors are conditions or vulnerabilities that increase an individual’s or group’s susceptibility to a health problem. They are linked to the risk diagnosis label using “as evidenced by.”
Examples:
- Risk for Falls as evidenced by muscle weakness and history of falls.
- Risk for Infection as evidenced by break in skin integrity and invasive procedures.
4. Defining Characteristics (Signs and Symptoms)
Defining characteristics are the observable signs and symptoms that cluster together to indicate the presence of an actual nursing diagnosis. They are the patient’s subjective and objective data that validate the diagnosis. Defining characteristics are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by.”
Example: Deficient Fluid Volume related to excessive vomiting and diarrhea as evidenced by dry mucous membranes, decreased urine output, and poor skin turgor.
The Diagnostic Process: Step-by-Step
The diagnostic process involves three key phases to arrive at accurate nursing diagnoses:
- Data Analysis: Examining the collected assessment data.
- Identification of Health Problems, Risks, and Strengths: Interpreting the analyzed data to pinpoint patient issues and resources.
- Formulation of Diagnostic Statements: Writing clear and concise nursing diagnosis statements.
1. Analyzing Data
Data analysis involves several steps:
- Comparing Data to Standards: Comparing the patient’s data to established norms and health standards to identify deviations.
- Clustering Cues: Grouping related cues (signs and symptoms) together to identify patterns.
- Identifying Gaps and Inconsistencies: Looking for missing information or contradictory data that needs further investigation.
2. Identifying Health Problems, Risks, and Strengths
After data analysis, nurses, in collaboration with the patient, identify:
- Health Problems: Actual or potential issues that can be addressed by nursing interventions.
- Health Risks: Factors that increase the patient’s vulnerability to developing problems.
- Strengths: Patient resources, coping mechanisms, and abilities that can be leveraged in the care plan.
This step also includes differentiating between nursing diagnoses, medical diagnoses, and collaborative problems to ensure the focus remains on nursing’s scope of practice.
3. Formulating Diagnostic Statements
The final step is to formulate the nursing diagnosis statements. This involves selecting the appropriate diagnostic label, identifying related factors or risk factors, and listing defining characteristics (for actual diagnoses). The next section details how to write these statements effectively.
How to Write a Nursing Diagnosis Statement: Step-by-Step Guide
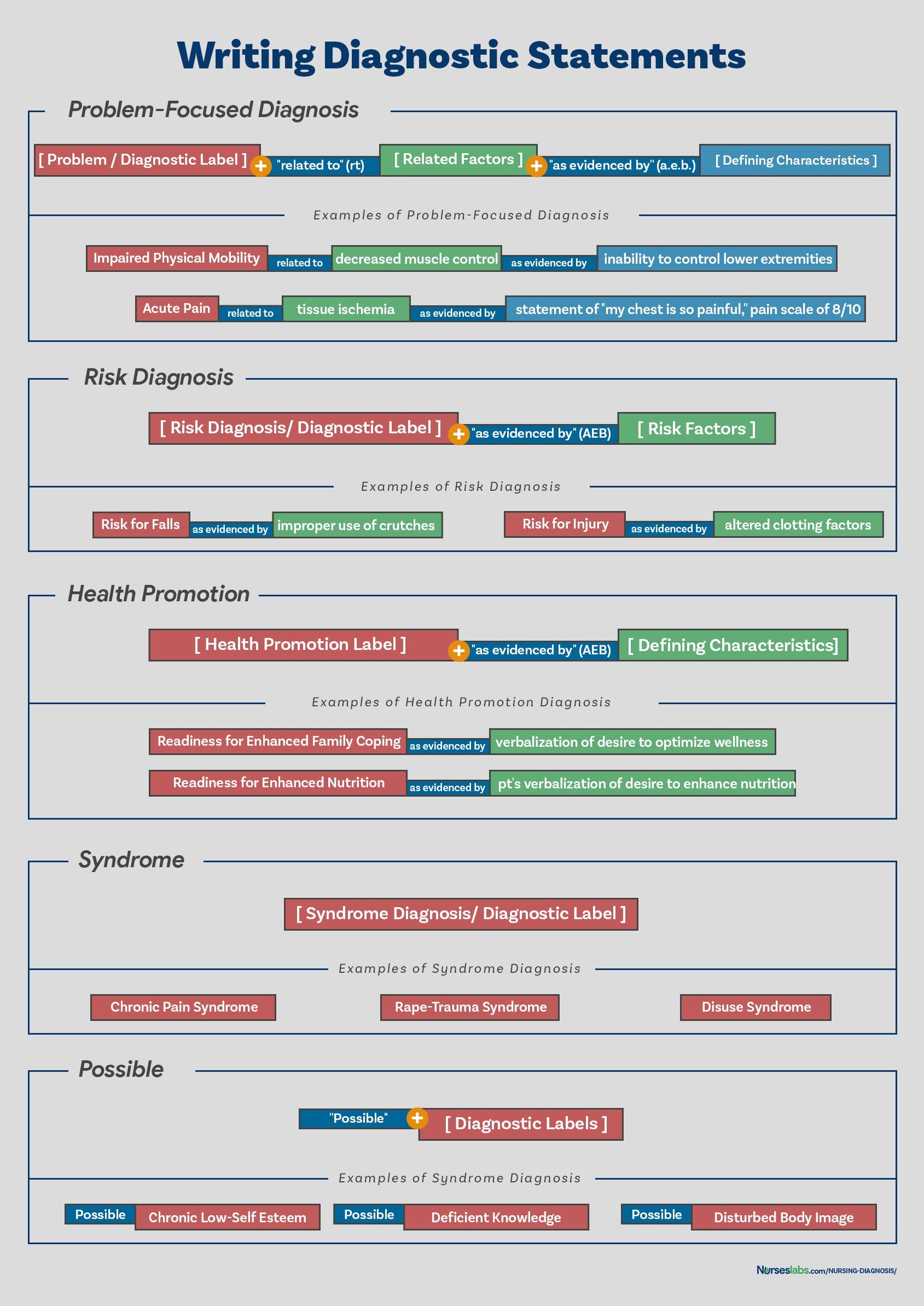
Writing clear and accurate nursing diagnosis statements is crucial for effective communication and care planning. The format varies slightly depending on the type of diagnosis.
WRITING DIAGNOSTIC STATEMENTS. Your guide on how to write different nursing diagnostic statements.
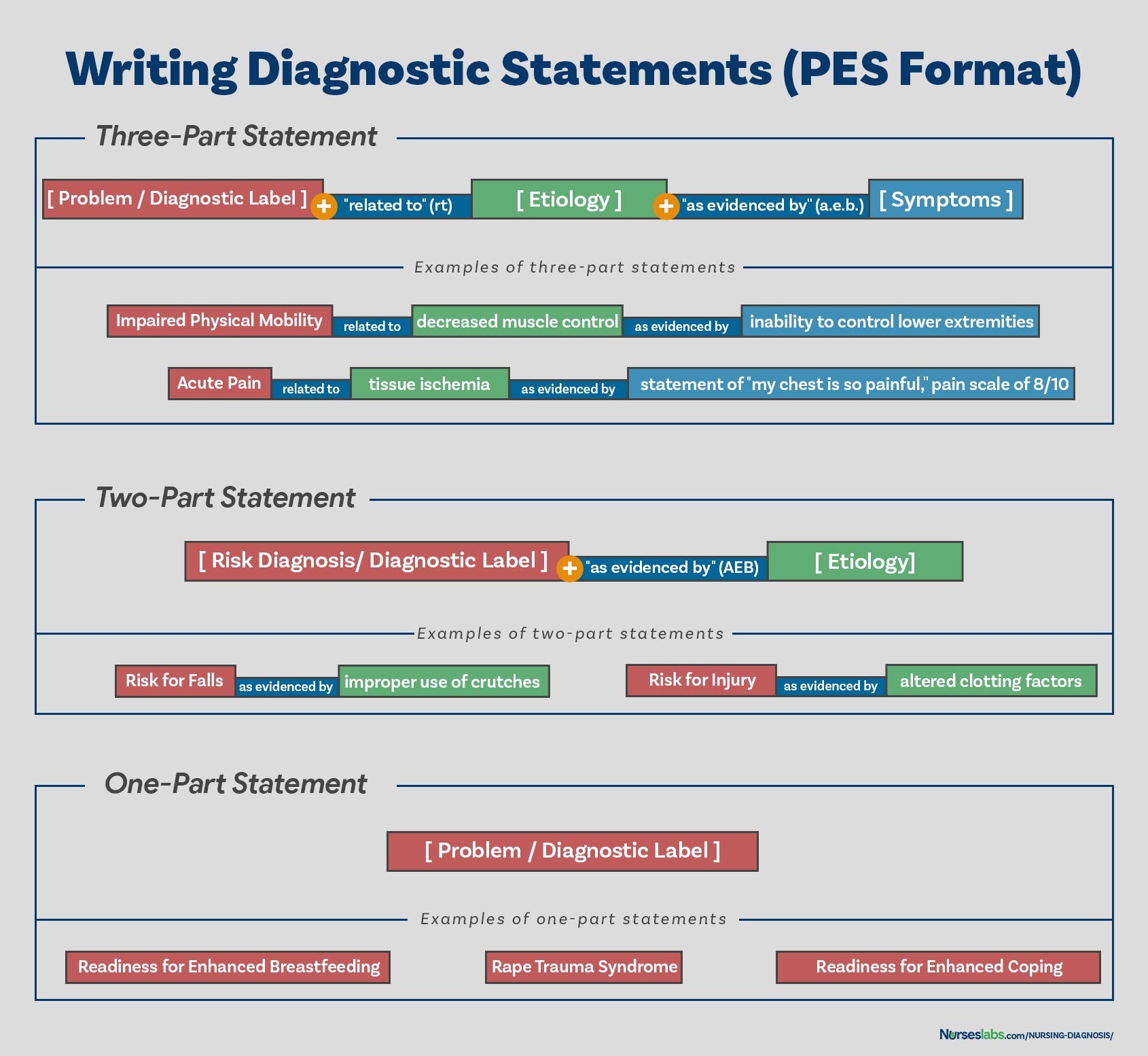
Using the PES Format
The PES format is a common and helpful structure for writing nursing diagnoses, particularly for problem-focused (actual) diagnoses. PES stands for:
- Problem (Diagnostic Label)
- Etiology (Related Factors)
- Signs/Symptoms (Defining Characteristics)
Diagnostic statements can be one-part, two-part, or three-part using the PES format, depending on the type of diagnosis.
PES FORMAT. Writing nursing diagnoses using the PES format.
One-Part Nursing Diagnosis Statement
- Used for: Health promotion and syndrome diagnoses.
- Format: Diagnostic Label only.
- Reason: Related factors are either always the same (health promotion) or inherent in the syndrome definition.
Examples:
- Readiness for Enhanced Coping
- Rape Trauma Syndrome
Two-Part Nursing Diagnosis Statement
- Used for: Risk and possible nursing diagnoses.
- Format: Diagnostic Label + “as evidenced by” + Risk Factors (for risk) or “Possible” + Diagnostic Label (for possible).
- Reason: Risk and possible diagnoses do not have defining characteristics (signs and symptoms) as the problem is not yet present or confirmed.
Examples:
- Risk for Infection as evidenced by weakened immune system response
- Risk for Injury as evidenced by unstable hemodynamic profile
- Possible Deficient Fluid Volume
Three-part Nursing Diagnosis Statement
- Used for: Actual (problem-focused) nursing diagnoses.
- Format (PES): Diagnostic Label + “related to” + Related Factors + “as evidenced by” + Defining Characteristics.
- Reason: Provides a complete picture of the problem, its causes, and the supporting evidence.
Example: Ineffective Airway Clearance related to excessive mucus production as evidenced by adventitious breath sounds, ineffective cough, and changes in respiratory rate.
Variations on Basic Statement Formats:
While PES is a standard format, there might be slight variations depending on specific contexts or institutional guidelines. However, the core components of problem, cause, and evidence should be clearly communicated.
Nursing Diagnosis Examples for Care Plans
Here are some common nursing diagnosis examples that you can use as a starting point for developing your nursing care plans:
(Note: This section in the original article leads to other articles with lists of nursing diagnoses. For this rewritten article, we will not replicate those lists but emphasize that nurses should consult resources like NANDA-I and nursing diagnosis handbooks for comprehensive lists.)
For comprehensive lists and examples of nursing diagnoses, consult resources such as the NANDA-I nursing diagnosis list and specialized nursing diagnosis handbooks.
Recommended Resources for Nursing Diagnosis
To further enhance your understanding and skills in nursing diagnosis, consider these recommended resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: Valuable for its evidence-based approach and step-by-step guidance on assessment, diagnosis, and care planning.
- Nursing Care Plans – Nursing Diagnosis & Intervention: A comprehensive resource with numerous care plans reflecting current evidence-based guidelines.
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick-reference tool for identifying correct diagnoses and planning efficient patient care.
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: Detailed resource for planning, individualizing, and documenting care for a wide range of diseases and disorders.
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: Provides a broad range of care plans across various specialties.
(Note: Affiliate links to Amazon were present in the original article. In this rewritten version, we maintain the resource recommendations but remove the affiliate links as per instructions.)
Conclusion: Mastering Nursing Diagnosis for Optimal Patient Care
Mastering how to formulate accurate nursing diagnoses is fundamental to providing high-quality, patient-centered care. By understanding the definition, purposes, types, components, and diagnostic process, and by utilizing resources like standardized taxonomies and handbooks, nurses can effectively identify patient needs and develop individualized care plans. Nursing diagnosis is not just a step in the nursing process; it is the intellectual foundation for effective nursing practice and improved patient outcomes.
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.