Nursing diagnosis is a cornerstone of effective patient care. It’s the critical step where nurses analyze patient data to identify health problems and guide the development of personalized care plans. Understanding How To Write A Nanda Nursing Diagnosis is essential for nursing students and practicing nurses alike. This guide will delve into the intricacies of nursing diagnoses, focusing on the NANDA-I (North American Nursing Diagnosis Association International) system, the globally recognized standard for nursing terminology.
Understanding Nursing Diagnosis: The Foundation of Patient Care
A nursing diagnosis is defined as a clinical judgment about individual, family, group, or community responses to actual or potential health problems or life processes. It’s a statement that describes a patient’s health condition that nurses are licensed and competent to treat. This diagnosis forms the basis for selecting nursing interventions and achieving specific patient outcomes for which nurses are accountable. Nursing diagnoses are derived from a thorough nursing assessment, the first step of the nursing process, and are crucial for developing effective nursing care plans.
Why is Nursing Diagnosis Important? Key Purposes
Nursing diagnoses serve several vital purposes in healthcare:
- Enhancing Critical Thinking: For nursing students, formulating diagnoses is an invaluable exercise in problem-solving and sharpening critical thinking skills.
- Prioritizing Care: Nursing diagnoses help nurses identify the most pressing patient needs, guiding the prioritization of nursing interventions.
- Outcome-Based Care: They facilitate the establishment of measurable expected outcomes, essential for quality assurance and accountability to healthcare payers.
- Holistic Patient Understanding: Nursing diagnoses illuminate how patients respond to health issues and life events, considering their strengths and resources to address problems.
- Professional Communication: They provide a standardized language, fostering clear and effective communication among nurses and the interdisciplinary healthcare team.
- Evaluating Care Effectiveness: Nursing diagnoses offer a framework for evaluation, determining the effectiveness and cost-efficiency of nursing care provided.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems: Key Differences
It’s crucial to differentiate nursing diagnoses from medical diagnoses and collaborative problems:
- Nursing Diagnosis: Focuses on the patient’s response to a health condition. It describes a patient’s health state that nurses can independently address within their scope of practice. For instance, a patient with pneumonia might have the nursing diagnosis “Ineffective Airway Clearance related to excessive mucus production.”
- Medical Diagnosis: Identifies a disease or pathological condition that only a physician or advanced practitioner can treat. Examples include Pneumonia, Diabetes Mellitus, or Appendicitis. Medical diagnoses guide medical treatment, while nursing diagnoses guide nursing care.
- Collaborative Problems: Are potential or actual health complications that require both medical and nursing interventions. Nurses monitor for and manage these problems using physician-prescribed and nurse-initiated actions. For example, a patient post-surgery is at risk for a collaborative problem like “Risk for Postoperative Infection,” requiring both medical interventions (antibiotics) and nursing interventions (wound care, monitoring).
The key distinction is that nursing diagnoses address patient responses to health conditions, guiding independent nursing actions, while medical diagnoses identify diseases requiring medical treatment. Collaborative problems bridge both domains, requiring coordinated care.
NANDA-I: The Standardized Language of Nursing Diagnosis
To ensure consistent and universal communication, nursing diagnoses are standardized through systems like NANDA-I. NANDA-I (North American Nursing Diagnosis Association International) provides a standardized taxonomy and terminology for nursing diagnoses, facilitating clear communication, research, and evidence-based practice in nursing.
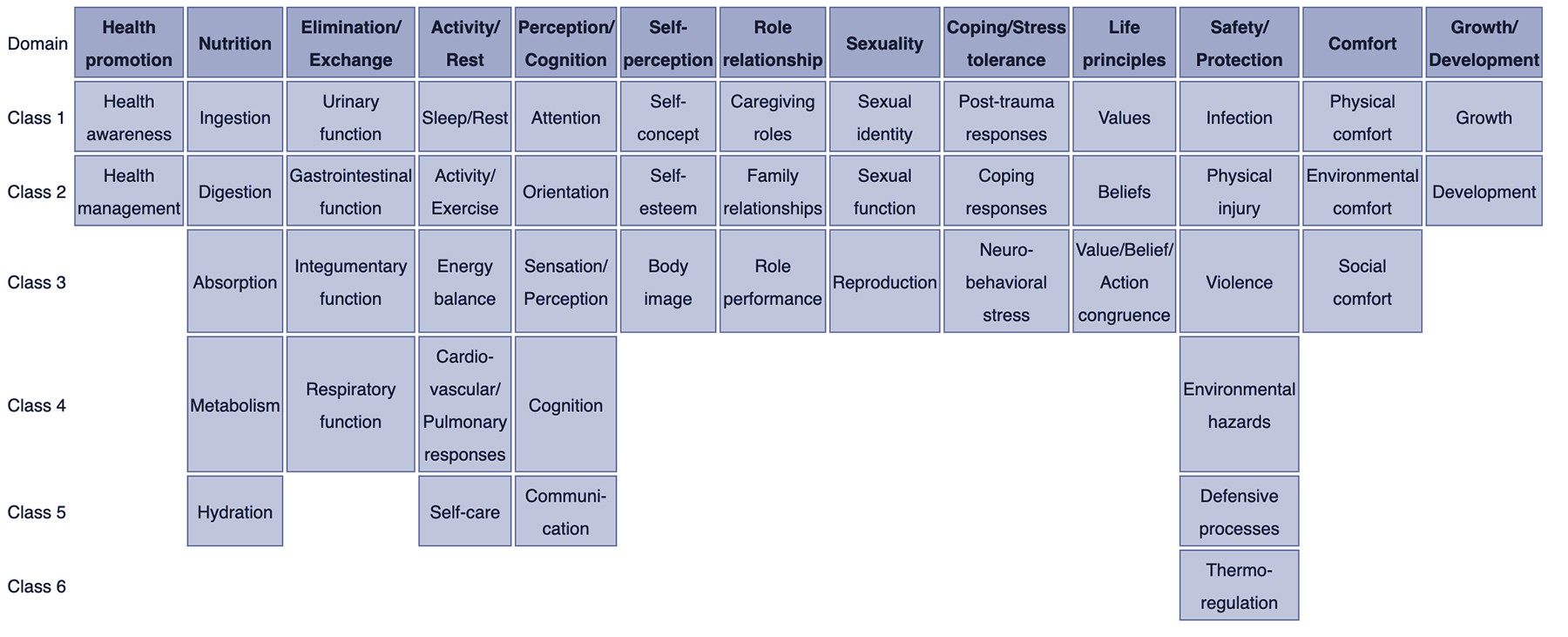
The NANDA-I taxonomy is organized into a multi-axial system, currently using 13 domains:
NANDA-I Domains:
- Domain 1: Health Promotion – Focuses on the awareness of well-being and health management.
- Domain 2: Nutrition – Addresses activities related to intake, digestion, absorption, metabolism, and hydration.
- Domain 3: Elimination and Exchange – Concerns bodily waste elimination and fluid and electrolyte balance.
- Domain 4: Activity/Rest – Covers sleep, rest, activity, exercise, energy balance, and cardiovascular and respiratory responses.
- Domain 5: Perception/Cognition – Deals with sensory and cognitive processes, including attention, orientation, and communication.
- Domain 6: Self-Perception – Focuses on self-concept, self-esteem, and body image.
- Domain 7: Role Relationship – Addresses roles and relationships, including caregiving and family dynamics.
- Domain 8: Sexuality – Concerns sexual identity, function, and reproduction.
- Domain 9: Coping/Stress Tolerance – Relates to coping mechanisms, stress responses, and post-trauma responses.
- Domain 10: Life Principles – Covers values, beliefs, and spiritual well-being.
- Domain 11: Safety/Protection – Addresses safety, security, infection, injury, and environmental hazards.
- Domain 12: Comfort – Concerns physical, environmental, and social comfort.
- Domain 13: Growth/Development – Focuses on growth and developmental milestones across the lifespan.
Within these domains are classes and then specific nursing diagnoses. Using NANDA-I ensures that nurses worldwide are speaking the same language when describing patient health problems.
The Nursing Process and Nursing Diagnosis
Nursing diagnosis is the second step in the nursing process, a systematic, five-step approach to patient care:
- Assessment: Gathering patient data (subjective and objective).
- Diagnosis: Analyzing data to identify nursing diagnoses.
- Planning: Setting goals and outcomes, and planning nursing interventions.
- Implementation: Carrying out the planned interventions.
- Evaluation: Assessing the effectiveness of interventions and progress toward outcomes.
Nursing diagnosis is the crucial link between assessment and planning. Accurate diagnoses ensure that care plans are tailored to address the patient’s specific needs identified during assessment.
Types of Nursing Diagnoses: A Closer Look
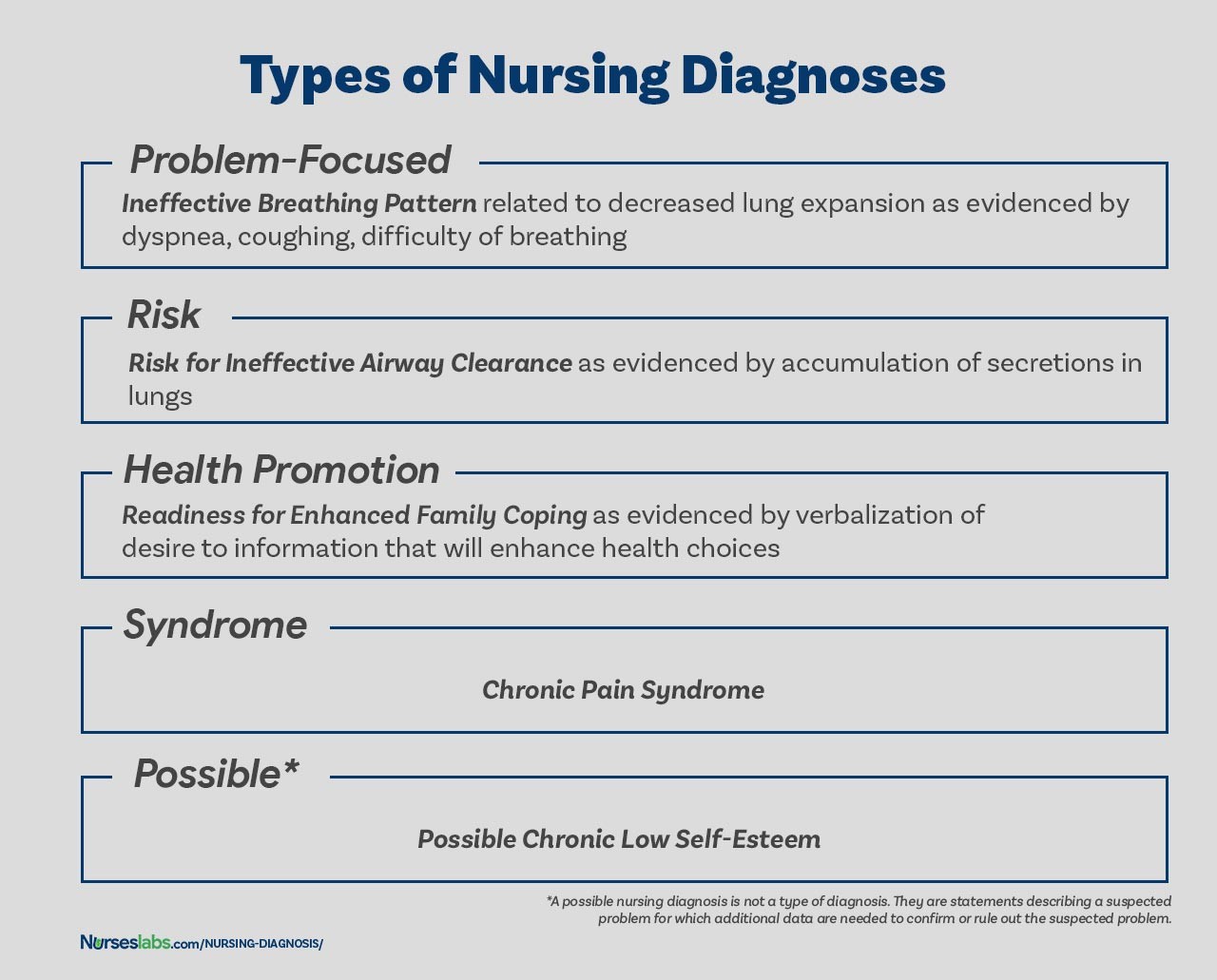
NANDA-I recognizes several types of nursing diagnoses, each serving a distinct purpose:
1. Problem-Focused (Actual) Nursing Diagnosis
A problem-focused nursing diagnosis, also known as an actual diagnosis, describes a current problem that the patient is experiencing at the time of assessment. It’s supported by defining characteristics – observable signs and symptoms. These diagnoses are written using a three-part statement (PES format, discussed later).
- Example: Impaired Physical Mobility related to pain as evidenced by reluctance to move, limited range of motion, and verbal report of pain.
2. Risk Nursing Diagnosis
A risk nursing diagnosis identifies potential problems that a patient is vulnerable to developing. It indicates that risk factors are present, increasing the patient’s susceptibility to a particular problem. Risk diagnoses are crucial for preventative care. They are written as two-part statements, linking the risk diagnosis to risk factors.
- Example: Risk for Infection as evidenced by surgical incision, compromised immune system, and presence of invasive lines.
3. Health Promotion Nursing Diagnosis
A health promotion nursing diagnosis focuses on a patient’s desire and motivation to improve their health and well-being. It highlights strengths and readiness to enhance wellness. These diagnoses are often one-part statements, focusing on the patient’s readiness for improvement.
- Example: Readiness for Enhanced Nutrition as evidenced by expressed interest in learning about healthy eating and choosing healthier food options.
4. Syndrome Nursing Diagnosis
A syndrome nursing diagnosis represents a cluster of actual or risk nursing diagnoses that frequently occur together due to a specific event or situation. These are also typically one-part statements, naming the syndrome.
- Example: Rape-Trauma Syndrome (encompasses a cluster of diagnoses like anxiety, fear, disturbed sleep pattern, etc., in response to sexual assault).
5. Possible Nursing Diagnosis
While not officially a type, possible nursing diagnoses are used when more data is needed to confirm or rule out a suspected problem. They indicate a potential issue requiring further assessment.
- Example: Possible Fluid Volume Deficit related to unknown etiology. (Further assessment needed to confirm fluid deficit and its cause).
Components of a NANDA Nursing Diagnosis Statement
A well-written NANDA nursing diagnosis statement typically includes three key components, especially for problem-focused diagnoses:
1. Problem (Diagnostic Label) and Definition
This is a concise statement of the patient’s health problem, drawn from the NANDA-I list of diagnoses. It has two parts:
- Qualifier (Modifier): Words that add specific meaning to the diagnosis, like “deficient,” “impaired,” “ineffective,” or “risk for.”
- Focus of the Diagnosis: The area of health concern, such as “Fluid Volume,” “Gas Exchange,” or “Tissue Perfusion.”
| Qualifier | Focus of the Diagnosis |
|---|---|
| Deficient | Fluid Volume |
| Imbalanced | Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange |
| Ineffective | Tissue Perfusion |
| Risk for | Injury |
2. Etiology (Related Factors)
The etiology identifies the probable cause(s) or contributing factors to the nursing diagnosis. It answers “why” the problem is occurring. Etiologies guide nursing interventions by addressing the root cause of the issue. The etiology is linked to the problem statement using the phrase “related to.”
- Example: Deficient Fluid Volume related to excessive vomiting and diarrhea. (Etiology: vomiting and diarrhea).
3. Defining Characteristics (Signs and Symptoms)
Defining characteristics are the observable cues (signs and symptoms) that cluster together and indicate the presence of a problem-focused nursing diagnosis. They validate the diagnosis. For risk diagnoses, risk factors take the place of defining characteristics. Defining characteristics are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by.”
- Example: Impaired Skin Integrity related to prolonged pressure as evidenced by redness and open area on sacrum. (Defining characteristics: redness and open area on sacrum).
The Diagnostic Process: A Step-by-Step Guide
Formulating accurate nursing diagnoses involves a systematic diagnostic process:
1. Data Analysis
This phase involves:
- Comparing data to standards: Identifying deviations from normal health patterns.
- Clustering cues: Grouping related data to identify patterns.
- Identifying gaps and inconsistencies: Recognizing missing information or conflicting data that needs further investigation.
2. Identifying Health Problems, Risks, and Strengths
After data analysis, the nurse:
- Identifies actual and potential problems: Determines if the data supports actual, risk, or possible nursing diagnoses.
- Differentiates nursing, medical, and collaborative problems: Distinguishes between problems nurses can address independently, those requiring medical treatment, and those requiring collaborative management.
- Identifies strengths and resources: Recognizes patient assets that can be used in the care plan.
3. Formulating Diagnostic Statements
This final step involves constructing the nursing diagnosis statement using the appropriate format (one-part, two-part, or three-part) and the PES format for problem-focused diagnoses.
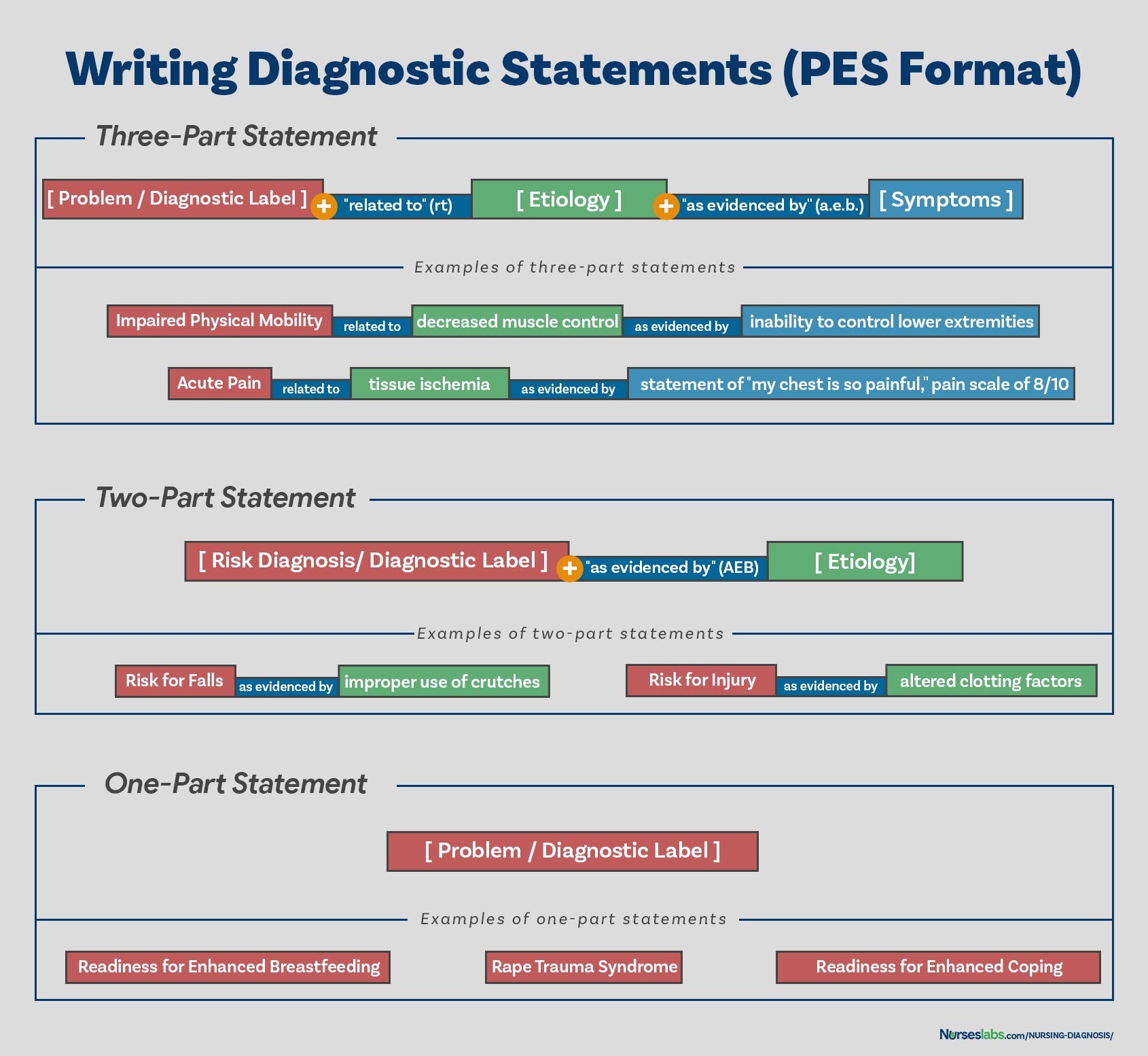
How to Write a NANDA Nursing Diagnosis: Mastering the PES Format
The PES format is a widely used and effective method for writing three-part nursing diagnosis statements for problem-focused diagnoses. PES stands for:
- P – Problem (Diagnostic Label): The NANDA-I diagnostic label that describes the patient’s health problem.
- E – Etiology (Related Factors): The factors contributing to or causing the problem, linked with “related to.”
- S – Signs and Symptoms (Defining Characteristics): The observable cues that validate the problem, linked with “as evidenced by.”
Example using PES format:
- P (Problem): Impaired Physical Mobility
- E (Etiology): related to pain
- S (Signs and Symptoms): as evidenced by reluctance to move, limited range of motion, and verbal report of pain.
Complete PES Statement: Impaired Physical Mobility related to pain as evidenced by reluctance to move, limited range of motion, and verbal report of pain.
Variations on Basic Statement Formats:
- One-Part Statements: Used for health promotion and syndrome diagnoses (e.g., Readiness for Enhanced Coping, Rape-Trauma Syndrome).
- Two-Part Statements: Used for risk and possible diagnoses, linking the diagnostic label to risk factors (e.g., Risk for Infection as evidenced by surgical incision).
Nursing Diagnosis for Care Plans: Building Effective Care
NANDA nursing diagnoses are the foundation for developing comprehensive nursing care plans. Once diagnoses are identified, nurses can then plan interventions to address the identified problems, achieve desired outcomes, and evaluate the effectiveness of care.
Recommended Resources for NANDA Nursing Diagnosis:
To further enhance your understanding and skills in writing NANDA nursing diagnoses, consider these recommended resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: A comprehensive guide with evidence-based interventions.
- Nursing Care Plans – Nursing Diagnosis & Intervention: Offers numerous care plans based on recent guidelines, including NANDA-I diagnoses.
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick reference tool for identifying correct diagnoses and planning care.
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: Provides detailed information for planning and documenting care for various diagnoses.
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: A broad resource covering care plans across specialties.
By mastering how to write a NANDA nursing diagnosis, nurses can significantly enhance their ability to provide patient-centered, effective, and evidence-based care. This skill is fundamental to professional nursing practice and improving patient outcomes.
References:
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.
