Crafting a nursing diagnosis is a foundational skill for every healthcare professional involved in patient care. It’s more than just identifying a problem; it’s about creating a clinical judgment concerning a human response to health conditions or life processes. This judgment then becomes the cornerstone of a patient’s nursing care plan, guiding interventions and ensuring personalized, effective care. In essence, a well-written nursing diagnosis is the compass that directs nurses towards achieving optimal patient outcomes.
This guide will navigate you through the essential concepts of writing a nursing diagnosis specifically for a care plan. We will explore what a nursing diagnosis truly is, differentiate it from medical diagnoses, delve into its various types, and most importantly, provide a practical, step-by-step approach to formulating these crucial statements. Whether you’re a nursing student just starting your journey or a seasoned practitioner looking to refine your skills, this comprehensive guide will equip you with the knowledge and tools necessary to master the art of writing nursing diagnoses that drive effective care plans.
Understanding the Essence of a Nursing Diagnosis
At its core, a nursing diagnosis is a clinical judgment. This judgment, made by a registered nurse, concerns an individual, family, group, or community’s response to actual or potential health issues or life events. It’s a statement that pinpoints what nurses can independently address within their scope of practice. It’s derived from a thorough nursing assessment, acting as the crucial link between assessment data and the tailored nursing care plan.
The purpose of a nursing diagnosis extends beyond mere labeling; it serves several critical functions in healthcare:
- Enhancing Critical Thinking: For nursing students, formulating diagnoses is an invaluable exercise in problem-solving and critical thinking. It pushes them to analyze data, identify patterns, and prioritize patient needs.
- Prioritizing Care: Nursing diagnoses directly inform the prioritization of care. By clearly defining patient problems, nurses can strategically allocate resources and interventions to address the most pressing needs first.
- Guiding Interventions: A nursing diagnosis is not just an identification of a problem, but also a guide for selecting appropriate nursing interventions. It directs nurses towards actions that are most likely to achieve desired patient outcomes.
- Establishing Expected Outcomes: These diagnoses play a key role in setting measurable and realistic expected outcomes, which are essential for quality assurance and are often required by healthcare payers.
- Facilitating Communication: By providing a standardized language, nursing diagnoses ensure clear and effective communication among nurses and the entire healthcare team. This shared understanding is vital for coordinated patient care.
- Evaluating Care Effectiveness: Nursing diagnoses provide a benchmark for evaluating the effectiveness of nursing care. By tracking progress against the diagnosed problems, nurses can determine if interventions are beneficial and adjust the care plan as needed.
It’s crucial to differentiate nursing diagnoses from medical diagnoses and collaborative problems to fully grasp their unique role in patient care.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems
While both nursing and medical diagnoses are essential in patient care, they address different aspects of a patient’s health. A medical diagnosis, made by a physician, identifies a disease or pathology. For instance, Diabetes Mellitus or Pneumonia are medical diagnoses. These diagnoses focus on the illness itself and guide medical treatments like medication and surgery.
In contrast, a nursing diagnosis focuses on the patient’s response to the medical condition or health problem. For example, a patient with pneumonia might have the nursing diagnosis of Ineffective Airway Clearance related to increased mucus production. This nursing diagnosis directs nursing interventions such as suctioning, positioning, and respiratory treatments. Nursing diagnoses are concerned with the patient’s physical, psychological, and spiritual responses to illness.
Collaborative problems are potential complications arising from medical diagnoses or treatments. These are problems that nurses monitor for and manage in collaboration with physicians, using both nurse-initiated and physician-prescribed interventions. An example is Risk for Complications related to surgery. Here, the nurse monitors for signs of complications and implements measures to prevent or manage them, often following physician orders alongside independent nursing actions.
Understanding these distinctions is fundamental to writing accurate and effective nursing diagnoses that contribute meaningfully to patient care plans.
Classifying Nursing Diagnoses: Navigating Taxonomy II
To standardize and organize nursing diagnoses, a classification system known as Taxonomy II is widely used. This system, developed by NANDA International (NANDA-I), provides a hierarchical structure for nursing diagnoses, making it easier to select the most appropriate diagnosis for a patient.
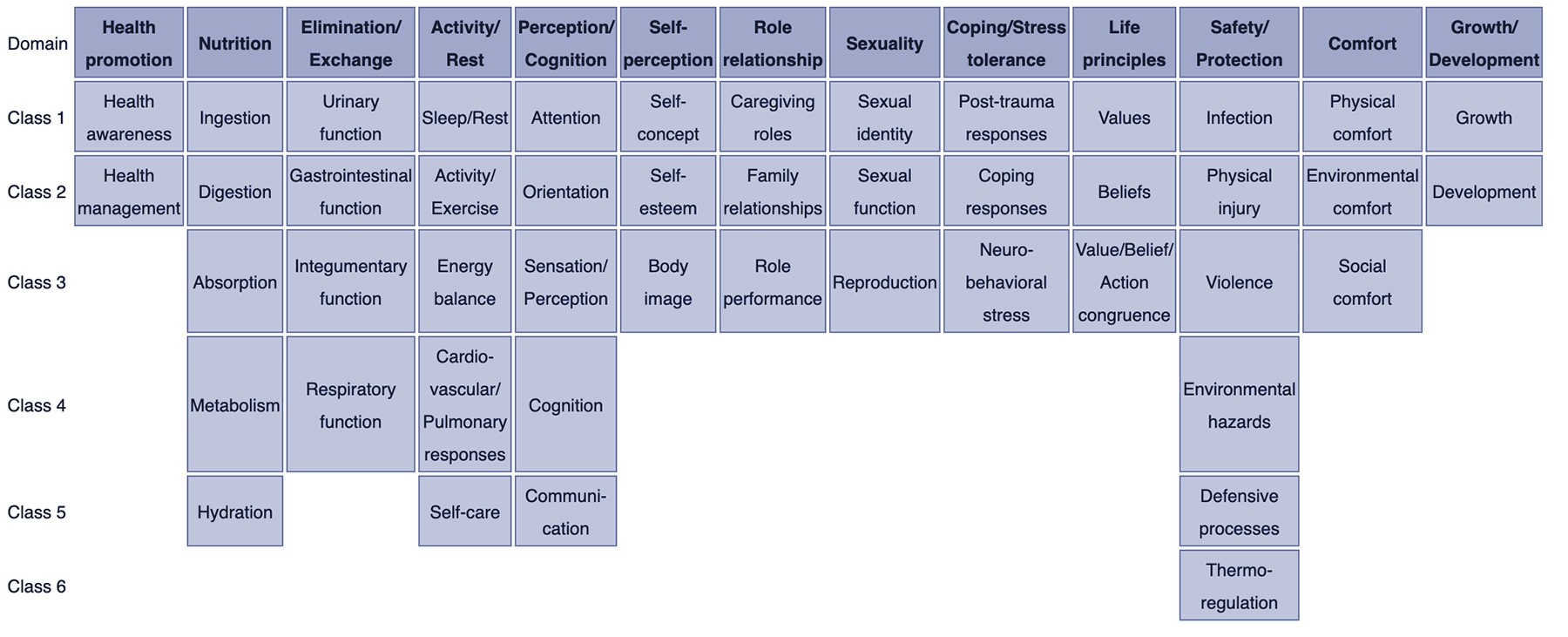
Taxonomy II is organized into three levels:
-
Domains (13): These are the broadest level, representing areas of human functioning. Examples include Health Promotion, Nutrition, Elimination and Exchange, Activity/Rest, Perception/Cognition, Self-Perception, Role Relationship, Sexuality, Coping/Stress Tolerance, Life Principles, Safety/Protection, Comfort, and Growth/Development.
-
Classes (47): Within each domain are classes, which are more specific categories. For example, within the domain Nutrition, classes include Ingestion, Digestion, Absorption, Metabolism, and Hydration.
-
Nursing Diagnoses: This is the most specific level, containing the actual nursing diagnosis labels. Diagnoses are arranged alphabetically within each class.
Using Taxonomy II helps ensure that nursing diagnoses are consistent and universally understood. It provides a framework for nurses to think systematically about patient problems and select diagnoses that accurately reflect the patient’s needs.
Types of Nursing Diagnoses: Actual, Risk, Health Promotion, and Syndrome
Nursing diagnoses are further categorized into four main types, each serving a distinct purpose in care planning:
-
Problem-Focused (Actual) Nursing Diagnosis: This type describes a client problem that is currently present at the time of assessment. It’s supported by defining characteristics – the signs and symptoms the patient is exhibiting. For example, Acute Pain related to surgical incision as evidenced by patient report of pain at 7/10, guarding behavior, and increased heart rate.
-
Risk Nursing Diagnosis: This diagnosis identifies potential problems that a patient is vulnerable to developing. It’s based on risk factors – conditions or situations that increase the patient’s susceptibility. For example, Risk for Infection as evidenced by surgical incision, compromised immune system, and presence of invasive lines. It’s important to note that risk diagnoses are just as crucial as actual diagnoses as preventative care is paramount.
-
Health Promotion Nursing Diagnosis: This type focuses on a patient’s desire to improve their well-being and health status. It’s used when a patient is already at a good level of health but wants to enhance it. For example, Readiness for Enhanced Nutrition as evidenced by patient expressing interest in learning about healthy eating and requesting dietary information.
-
Syndrome Nursing Diagnosis: This diagnosis is used when a cluster of actual or risk nursing diagnoses are likely to occur together in certain circumstances. These are typically one-part statements. For example, Rape Trauma Syndrome encompasses a range of potential diagnoses that may occur after sexual assault.
Understanding these different types is essential for selecting the correct diagnosis and tailoring the care plan to meet the patient’s specific needs, whether they are facing an existing problem, at risk of developing one, or seeking to improve their health.
Essential Components of a Nursing Diagnosis Statement
A well-formulated nursing diagnosis statement typically includes three key components, especially for problem-focused diagnoses, often remembered using the acronym PES:
-
Problem (Diagnostic Label): This is a concise statement of the patient’s health problem or response. It uses standardized NANDA-I terminology to ensure clarity and consistency. The label often includes a qualifier that adds specific meaning. Examples of qualifiers include Deficient, Impaired, Ineffective, and Risk for. The focus of the diagnosis is the area of concern, such as Fluid Volume, Gas Exchange, or Tissue Perfusion. For instance, Deficient Fluid Volume or Ineffective Tissue Perfusion.
-
Etiology (Related Factors): This component identifies the probable cause(s) or contributing factors to the health problem. It’s not a medical diagnosis but rather factors within the nurse’s realm of intervention. Etiology is linked to the problem using the phrase “related to.” For example, for Deficient Fluid Volume, a possible etiology could be related to excessive vomiting and diarrhea.
-
Signs and Symptoms (Defining Characteristics): For actual nursing diagnoses, this component includes the observable cues, signs, and symptoms that demonstrate the presence of the problem. These are linked to the problem and etiology using the phrase “as evidenced by” or “as manifested by.” For Deficient Fluid Volume related to excessive vomiting and diarrhea, defining characteristics might be as evidenced by decreased urine output, dry mucous membranes, and weak pulse.
For risk diagnoses, instead of defining characteristics, risk factors are used, linked with “as evidenced by.” For health promotion and syndrome diagnoses, the statement is often simpler, sometimes just including the diagnostic label or label with related factors for clarification.
The Diagnostic Process: A Step-by-Step Approach
Formulating a nursing diagnosis is a systematic process that involves three main phases:
-
Data Analysis: This initial phase involves a thorough review of all collected patient data from the nursing assessment. This includes:
- Comparing Data to Standards: Nurses compare patient data to established norms and healthy ranges. For example, is the patient’s blood pressure within normal limits? Is their respiratory rate typical? Deviations from these standards may indicate a problem.
- Clustering Cues: Nurses look for patterns and related cues in the data. Grouping together related signs and symptoms helps to identify potential problems. For instance, if a patient has a fever, cough, and reports shortness of breath, these cues cluster together and point towards a potential respiratory issue.
- Identifying Gaps and Inconsistencies: Nurses also identify missing information or data that doesn’t make sense. Gaps in data may require further assessment, while inconsistencies need clarification.
-
Identification of Health Problems, Risks, and Strengths: After analyzing the data, nurses move to identify specific health problems, potential risks, and patient strengths:
- Determining Nursing Diagnoses: Based on the clustered cues, nurses identify potential nursing diagnoses. They differentiate between nursing diagnoses, medical diagnoses, and collaborative problems, ensuring they are focusing on patient responses that nurses can independently address.
- Recognizing Strengths and Resources: It’s equally important to identify the patient’s strengths, resources, and coping abilities. These strengths can be leveraged in the care plan to promote healing and wellness.
-
Formulation of Diagnostic Statements: The final phase is writing the nursing diagnosis statement itself. This involves selecting the appropriate NANDA-I diagnostic label and constructing a clear, concise statement using the PES format (for problem-focused diagnoses) or appropriate format for other types.
Writing Effective Nursing Diagnosis Statements: Applying PES Format
The PES format is a widely used and effective method for writing nursing diagnosis statements, particularly for problem-focused diagnoses. It ensures that all essential components are included in a structured manner:
- P – Problem (Diagnostic Label): Begin with the standardized NANDA-I diagnostic label that identifies the patient’s health problem. For example, Impaired Physical Mobility.
- E – Etiology (Related Factors): Connect the problem to its likely cause or contributing factors using the phrase “related to.” For example, related to pain and stiffness.
- S – Signs and Symptoms (Defining Characteristics): For actual diagnoses, add the evidence that supports the diagnosis using the phrase “as evidenced by.” For example, as evidenced by inability to ambulate independently, reluctance to move, and verbal report of pain in joints.
Putting it all together, a complete three-part nursing diagnosis statement using PES format would be:
Impaired Physical Mobility related to pain and stiffness as evidenced by inability to ambulate independently, reluctance to move, and verbal report of pain in joints.
Variations in Statement Formats
While the three-part PES format is standard for actual diagnoses, other types of nursing diagnoses may use different formats:
- One-Part Statements: Health promotion and syndrome diagnoses often use a one-part statement, consisting only of the diagnostic label. For example, Readiness for Enhanced Coping or Rape Trauma Syndrome. Related factors may be added to health promotion diagnoses for clarity, but are not required.
- Two-Part Statements: Risk and possible nursing diagnoses typically use two-part statements.
- Risk Diagnoses: Include the diagnostic label and risk factors, connected by “as evidenced by.” For example, Risk for Infection as evidenced by surgical incision and immunosuppression.
- Possible Diagnoses: State the suspected problem, followed by “possible related to” and the reason for suspicion. For example, Possible Spiritual Distress related to loss of faith in God secondary to suffering. (Note: Possible diagnoses require further data to confirm or rule out).
Understanding these variations allows for accurate and appropriate formulation of nursing diagnoses for all patient situations and diagnosis types.
Nursing Diagnosis Examples for Care Plans
Here are some examples of nursing diagnoses commonly used in care plans, categorized for clarity:
For Patients with Respiratory Issues:
- Ineffective Airway Clearance related to increased mucus production as evidenced by adventitious breath sounds (rhonchi), weak cough, and oxygen saturation of 90%.
- Ineffective Breathing Pattern related to pain and anxiety as evidenced by rapid, shallow respirations, and reports of shortness of breath.
- Impaired Gas Exchange related to alveolar-capillary membrane changes as evidenced by confusion, cyanosis, and arterial blood gas results showing hypoxemia.
For Patients with Cardiovascular Issues:
- Decreased Cardiac Output related to altered contractility as evidenced by edema, fatigue, and weak peripheral pulses.
- Risk for Decreased Cardiac Tissue Perfusion as evidenced by hypertension, hyperlipidemia, and smoking history.
- Excess Fluid Volume related to decreased venous return as evidenced by weight gain, jugular vein distention, and crackles in lungs.
For Patients with Mobility Issues:
- Impaired Physical Mobility related to musculoskeletal impairment as evidenced by limited range of motion, unsteady gait, and difficulty changing positions.
- Risk for Falls as evidenced by muscle weakness, impaired balance, and use of assistive devices.
- Activity Intolerance related to generalized weakness as evidenced by reports of fatigue after minimal activity and abnormal heart rate response to activity.
For Patients with Nutrition and Elimination Issues:
- Imbalanced Nutrition: Less Than Body Requirements related to difficulty swallowing as evidenced by weight loss, poor muscle tone, and reported inadequate dietary intake.
- Constipation related to decreased physical activity and inadequate fluid intake as evidenced by infrequent bowel movements, abdominal distention, and reports of straining during defecation.
- Risk for Impaired Skin Integrity as evidenced by immobility, incontinence, and poor nutritional status.
For Patients with Psychosocial Issues:
- Anxiety related to unfamiliar hospital environment and uncertain prognosis as evidenced by restlessness, irritability, and verbalization of worry.
- Disturbed Sleep Pattern related to hospital routines and pain as evidenced by reports of difficulty falling asleep, frequent awakenings, and daytime fatigue.
- Deficient Knowledge related to new medication regimen as evidenced by expressed lack of understanding and frequent questions about medication.
These examples illustrate how nursing diagnoses are written for various patient problems and can be used as a starting point for developing personalized care plans. Remember to always tailor the diagnosis to the individual patient based on your comprehensive assessment.
Recommended Resources for Mastering Nursing Diagnosis
To further enhance your understanding and skills in writing nursing diagnoses, consider these highly recommended resources:
-
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: This comprehensive handbook is lauded for its evidence-based approach, offering a step-by-step system for client assessment, diagnosis, and care planning. It’s an excellent resource for building diagnostic reasoning and critical thinking skills.
-
Nursing Care Plans – Nursing Diagnosis & Intervention: This resource includes hundreds of care plans reflecting the latest evidence-based guidelines and incorporates ICNP diagnoses and contemporary health issues.
-
Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick, accessible tool for identifying correct diagnoses and planning patient care efficiently. It includes up-to-date nursing diagnoses and interventions for a wide range of disorders.
-
Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: This manual is invaluable for planning, individualizing, and documenting care for over 800 diseases and disorders. It offers subjectively and objectively defined diagnoses, sample applications, prioritized interventions with rationales, and documentation guidelines.
-
All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: This e-book provides over 100 care plans across various specialties, helping you become familiar with interprofessional patient problem approaches.
These resources provide in-depth information, examples, and practical guidance that can significantly improve your proficiency in writing nursing diagnoses and developing effective care plans.
Conclusion: The Power of a Well-Written Nursing Diagnosis
Mastering the art of writing nursing diagnoses is crucial for providing patient-centered and effective nursing care. A well-formulated nursing diagnosis is not just a label; it’s a precise clinical judgment that drives the entire nursing care plan. It ensures that interventions are targeted, outcomes are measurable, and care is truly individualized.
By understanding the types of nursing diagnoses, their components, and the step-by-step diagnostic process, you can create diagnoses that accurately reflect your patients’ needs and guide your actions as a nurse. Whether you are addressing an existing problem, preventing potential risks, or promoting wellness, the nursing diagnosis is your roadmap to delivering high-quality care. As you continue to practice and refine your skills, remember that each nursing diagnosis you write is a step towards improving patient outcomes and making a meaningful difference in their lives.
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.