Chronic Obstructive Pulmonary Disease (COPD) is a significant global health concern, known for its preventable and treatable nature, yet remaining a leading cause of morbidity and mortality worldwide. As healthcare systems grapple with the increasing prevalence and economic burden of COPD, robust research is crucial for informing effective public health strategies and healthcare delivery. Administrative databases, like those derived from National Health Insurance (NHI) programs, offer a valuable resource for conducting large-scale COPD studies due to their extensive population coverage and longitudinal data. A cornerstone of utilizing these databases for research is the accuracy of diagnostic codes, particularly the ICD-9 diagnosis code for COPD. This article delves into the validity and limitations of using ICD-9-CM codes to identify COPD cases within healthcare databases, emphasizing the importance of validation studies for ensuring research integrity and applicability.
The Role of ICD-9-CM Codes in COPD Identification within Databases
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes are widely used to categorize and code diagnoses and procedures in healthcare settings. For COPD research using administrative databases, specific ICD-9-CM codes (491, 492, and 496) are commonly employed to identify patient cohorts. These codes, while efficient for large-scale data analysis, are primarily designed for billing and administrative purposes, not necessarily for clinical research accuracy. Therefore, the positive predictive value – the probability that patients identified by these codes truly have COPD – becomes a critical factor in determining the reliability of research findings.
Previous studies have utilized claim data from databases like Taiwan’s National Health Insurance Research Database (NHIRD) to investigate COPD. However, questions remain regarding the accuracy of COPD diagnosis based solely on ICD-9-CM codes within these datasets. This is not unique to COPD; the inherent limitations of diagnostic codes in capturing the full clinical picture are a broader concern in database research across various diseases. To address this gap, a validation study was conducted to evaluate the effectiveness of ICD-9-CM codes in accurately identifying COPD patients in the NHIRD, and to explore factors that could enhance diagnostic accuracy.
Study Methodology: Validating COPD Diagnosis from Claim Data
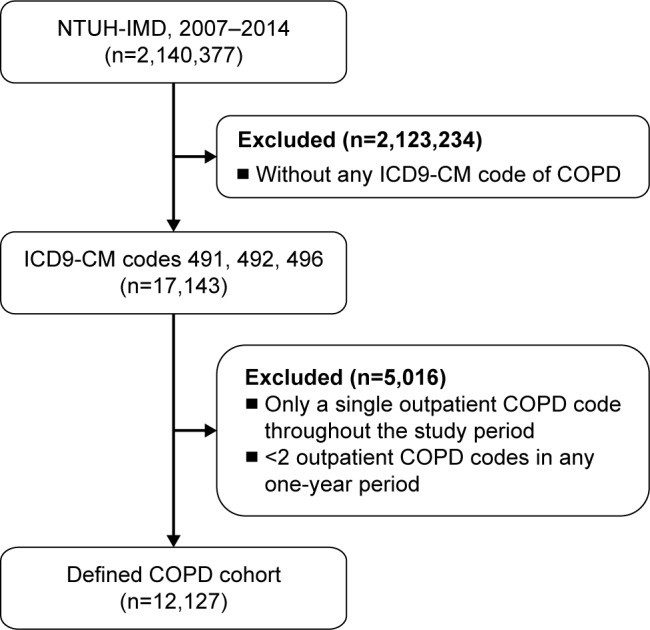
A cross-sectional study was designed to compare COPD diagnoses derived from claim data with physician-verified diagnoses at a major medical center in Taiwan. Data spanning from 2007 to 2014 were analyzed, focusing on patients identified as having COPD based on ICD-9-CM codes within the NHIRD. The study aimed to determine the positive predictive value of these codes and to identify factors that could improve the accuracy of COPD identification.
Data Sources and Patient Cohort
The study utilized data from both the National Taiwan University Hospital (NTUH) Integrated Medical Database (NTUH-IMD) and reimbursement claim data from Taiwan’s NHI program at NTUH. This approach allowed for a comprehensive review, supplemented by chart reviews when necessary, to ensure data accuracy. The NTUH-IMD provided detailed patient records, while the claim data mirrored the information available in the NHIRD.
Patients were included in the COPD cohort if they met a common criterion based on ICD-9-CM codes: at least two outpatient claims within a year or at least one inpatient claim coded for COPD (ICD-9-CM codes 491, 492, and 496). This initial cohort was intentionally broad to examine the baseline accuracy of using diagnostic codes alone.
COPD Verification and Classification
Recognizing that spirometry, the gold standard for COPD diagnosis, is not always consistently performed in real-world clinical practice, the study employed physician-verified COPD as the reference standard. Two experienced pulmonologists, blinded to the claim data status, independently reviewed patient information, including clinical manifestations, smoking history, and spirometry data when available. They categorized patients into three groups: COPD, indeterminate, and not COPD. Discrepancies were resolved through discussion to reach a consensus diagnosis. This rigorous verification process ensured a robust gold standard against which to evaluate the ICD-9-CM code-based diagnosis.
Data Analysis and Endpoints
The primary endpoint was the positive predictive value of COPD diagnosis using ICD-9-CM codes from claim data, validated against physician diagnoses. The study also explored how different criteria for applying ICD-9-CM codes (varying the number of outpatient or inpatient codes required) affected the positive predictive value. Furthermore, researchers investigated patient characteristics, such as age, sex, comorbidities, and spirometry test results, to determine their association with diagnostic accuracy. Statistical analyses, including logistic regression, were used to identify independent factors influencing the positive predictive value of claim data-defined COPD.
Key Findings: Accuracy and Factors Influencing ICD-9 Code Validity for COPD
The study population initially comprised 12,127 subjects who met the criteria for COPD based on ICD-9-CM codes in their claim data. Physician verification revealed that 7,701 (63.5%) of these subjects were confirmed to have COPD. This initial finding highlights a crucial point: relying solely on a common criterion of ICD-9-CM codes resulted in a positive predictive value of 63.5%. This indicates that over a third of patients identified using these codes might not actually have COPD, emphasizing the potential for misclassification in database studies.
Impact of Stricter ICD-9-CM Code Criteria
To explore if stricter criteria could improve accuracy, the researchers tested more stringent definitions for COPD based on claim data. Applying a criterion of three or more outpatient codes or two or more inpatient codes increased the positive predictive value to 72.2%. While this improvement is statistically significant, it still indicates that a considerable proportion of patients identified by even stricter ICD-9-CM code criteria may not have physician-verified COPD.
Influence of Patient Characteristics and Spirometry
Multivariate logistic regression analysis identified several independent factors associated with the positive predictive value of ICD-9-CM code-defined COPD. Age ≥65 years and a claim for spirometry emerged as the two most significant factors. Older age was associated with a higher likelihood of accurate COPD diagnosis using claim data, potentially due to increased COPD prevalence in older populations and greater healthcare utilization. Crucially, having a claim for spirometry was strongly associated with a higher positive predictive value.
The study further demonstrated that incorporating spirometry testing into the diagnostic criteria significantly enhanced accuracy. When spirometry testing was added as a prerequisite to ICD-9-CM codes, the positive predictive value increased substantially to 84.6%. This finding underscores the critical role of spirometry in COPD diagnosis and suggests that combining ICD-9-CM codes with evidence of spirometry significantly improves the identification of true COPD cases within administrative databases.
Discussion: Implications for Research and Database Utilization
This study provides critical insights into the validity of using ICD-9 diagnosis codes for COPD in administrative health databases. The findings clearly demonstrate that relying solely on ICD-9-CM codes, even with stricter criteria, has limitations in accurately identifying COPD patients. The positive predictive values observed, ranging from 63.5% to 72.2% for ICD-9-CM codes alone, highlight the potential for misclassification and the need for caution when interpreting research based solely on these codes.
The study strongly emphasizes the importance of validation studies when utilizing administrative databases for disease-specific research. The accuracy of diagnostic codes can be influenced by various factors, including coding practices, the level of clinical detail captured by the coding system, and the primary purpose of data collection (billing vs. research). Therefore, validating diagnostic codes against a clinical gold standard, such as physician verification, is essential for ensuring the reliability and generalizability of research findings.
The significant improvement in positive predictive value when spirometry is incorporated into the case definition has important practical implications. For researchers using the NHIRD or similar databases, including spirometry testing as a criterion, when feasible, can substantially enhance the accuracy of COPD cohort identification. This approach leverages the strengths of administrative data while mitigating the limitations of relying solely on diagnostic codes.
Generalizability and Future Research
While this study was conducted at a single medical center in Taiwan, the findings likely have broader implications for other healthcare systems utilizing ICD-9-CM codes and administrative databases. The standardized nature of the NHI program in Taiwan, with uniform coding and reimbursement practices across accredited healthcare providers, suggests that the results may be generalizable to other medical centers within Taiwan. However, variations in coding quality and healthcare practices across different regions and countries necessitate further validation studies in diverse settings.
Future research should focus on exploring other potential factors that could further improve the accuracy of COPD identification in administrative databases. This may include incorporating additional clinical data available within the databases, such as medication records, healthcare utilization patterns, and demographic information. Furthermore, with the transition to ICD-10 coding systems, similar validation studies are crucial to assess the accuracy of ICD-10 diagnosis codes for COPD in identifying patient cohorts for research.
Conclusion: Enhancing COPD Research with Validated Diagnostic Approaches
In conclusion, this study provides valuable evidence regarding the validity of ICD-9 diagnosis codes for COPD within the Taiwan NHIRD. It underscores the limitations of using ICD-9-CM codes alone for accurately identifying COPD patients and highlights the significant improvement in diagnostic accuracy achieved by incorporating spirometry testing into the case definition. The findings emphasize the critical importance of validating disease-specific diagnoses when using administrative databases for clinical research. By adopting validated approaches, researchers can enhance the reliability and applicability of their findings, ultimately contributing to a better understanding of COPD and improved patient care.
Keywords: Icd 9 Diagnosis Code For Copd, chronic obstructive pulmonary disease, database, International Classification of Diseases code, Taiwan, validity