Abstract
Background
Effective delirium management in hospital settings is a multifaceted challenge that necessitates robust interprofessional and interdisciplinary communication and collaboration. This quality improvement project was designed to evaluate the impact of a specialized interprofessional education (IPE) course focused on delirium, assessing its effectiveness in empowering clinicians to spearhead quality improvement projects within their respective hospitals.
Method
This quality improvement project was conducted within a university-affiliated hospital. A cohort of clinicians, including physicians, nurses, and therapists, participated in a comprehensive 2-day IPE course centered on delirium management. The course was officially certified by the German Society of Intensive Care Medicine. Following the course, participants were tasked with developing and implementing quality improvement projects within their clinical areas. The outcomes of these projects were then presented and evaluated in a follow-up meeting held eight weeks post-training.
Results
A total of 16 clinicians, comprising eight nurses, six therapists, and two physicians from six distinct wards, participated in the IPE course. These participants formed five project groups. At the eight-week evaluation, four of the five groups presented projects that demonstrated successful and ongoing implementation. These projects included the establishment of a hospital-wide delirium expert panel, the creation of delirium-focused informational flyers for patient relatives, the development of a concise one-page information sheet for clinicians across the hospital, and a structured teaching module for therapist training. The implementation of the 4AT delirium assessment tool within electronic patient charts was initiated but required a longer timeframe, extending beyond the initial eight-week project period. Participant feedback indicated high satisfaction with the IPE course, with clinicians reporting a significant increase in their perceived competence in managing patients experiencing delirium.
Conclusions
The findings of this project indicate that a dedicated IPE course on delirium management is effective in motivating and enabling clinicians to initiate and execute delirium-specific quality improvement projects within their hospital environments. Further research is warranted to assess the long-term sustainability of these quality improvement projects and to determine the influence of various contextual factors, such as hospital culture and setting, on project outcomes.
BACKGROUND
Delirium is recognized as a severe and frequently underdiagnosed condition that poses significant risks to hospitalized patients. Defined by acute and fluctuating disturbances in attention and cognition, delirium is a common occurrence among hospitalized individuals, associated with increased morbidity and mortality. Despite its prevalence across various hospital wards and units, effective delirium management remains a complex clinical challenge.
Implementing effective delirium management strategies in critical care settings is a complex undertaking, often hindered by numerous factors. These include the intricate and varied causes of delirium, the frequent under-recognition of the condition, staffing shortages, polypharmacy, and various medical procedures. Conversely, several factors can facilitate improved delirium management, such as the adoption of clinical guidelines and protocols, a multidisciplinary and interprofessional approach to care, the use of non-pharmacological prevention and treatment methods, a focus on family- and patient-centered care, and comprehensive education for healthcare staff. Recognizing and addressing both these challenges and facilitating factors is crucial for enhancing delirium management. Regular service evaluations are essential to assess the quality of care provided and identify areas for improvement. In our hospital, we observed a perceived lack of delirium awareness, with delirium often seen as a common but benign condition. Additional challenges included high workloads due to nursing shortages, limited opportunities for documenting delirium, prioritization of routine tasks over delirium-specific care, a lack of established delirium management protocols, uncertainty about the implications of positive delirium assessments, insufficient knowledge among staff, and suboptimal interprofessional communication. These issues are consistent with common challenges reported in existing literature.
Interprofessional education (IPE) is defined as collaborative learning that involves members from two or more professions learning with, from, and about each other to enhance collaboration, improve the quality of care, and optimize service delivery. In the context of hospitals, IPE is crucial for improving patient outcomes, particularly in areas like delirium care, by fostering effective teamwork and communication. IPE programs are specifically designed to equip healthcare professionals from diverse disciplines with the necessary skills, knowledge, and attitudes to function cohesively as a team. The German Interdisciplinary Society of Intensive Care Medicine (DIVI) has recently developed a curriculum for an IPE course focused on delirium management. This curriculum aims to deepen and broaden delirium-specific knowledge and empower clinicians to refine their treatment strategies. The delirium curriculum, available in German, underscores the importance of interprofessional care in effectively diagnosing and managing delirium.
This project aimed to evaluate whether an IPE course focused on delirium management could empower clinicians to initiate and conduct quality improvement projects. The focus was on projects that incorporate interprofessional and interdisciplinary approaches within their hospital settings, ultimately leading to better interprofessional care delirium diagnosis and management.
METHODS
This quality improvement (QI) project was reported in accordance with the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines and adhered to principles of Good Clinical Practice.
Context
The study was conducted at Sana Kliniken Niederlausitz, a university-affiliated specialist care hospital in Germany with 543 beds and 1,200 employees. Prior to this project, the hospital lacked formal delirium management protocols or systematic service assessments related to delirium care.
Intervention
The DIVI-certified IPE course on delirium management consisted of 20 teaching units, each lasting 45 minutes, focusing on delirium within intensive care and emergency medicine contexts. The curriculum provided essential knowledge about delirium, educated participants on current delirium management strategies, and offered guidance on implementation using the plan-do-check-act (PDCA) cycle. Designed for interprofessional and interdisciplinary teams, the course allowed providers to select educational approaches including case-based discussions, reflective learning through experience sharing, simulated scenarios like role-playing, and problem-based learning focused on designing and launching quality improvement projects. The program was delivered over two full working days, including breaks, and concluded with a four-hour evaluation meeting eight weeks later.
Recognizing that effective delirium management implementation is a complex process, the course addressed various influencing factors. These include the nature of the intervention itself, organizational culture (structures, processes, and readiness for change), local conditions (staffing levels, legal and regulatory frameworks), and clinician-related factors (attitudes, knowledge, competencies). Barriers and facilitators within each of these areas were also considered as critical components affecting the success of delirium management initiatives.
Measures
At the conclusion of the initial two-day IPE course, participants were organized into groups. They were instructed to reflect on opportunities to improve delirium management within their wards and units. This reflection included identifying and assessing both barriers and facilitators to effective delirium care in their specific clinical settings. Each group then presented a brief summary of their discussions and defined a realistic, achievable goal for the subsequent eight-week period, focusing on quality improvement initiatives.
Analysis
The primary evaluation focused on assessing the participants’ ability to independently conduct their self-defined QI projects within their respective clinical areas. The primary outcome measure was the number of projects successfully presented at the eight-week evaluation meeting, indicating the effectiveness of the IPE course in fostering practical quality improvements in interprofessional care delirium diagnosis and management.
Ethical Considerations
As this initiative was classified as a service evaluation and quality improvement project, it was determined that formal ethics approval was not required. The project aimed to enhance patient care through educational intervention and process improvement, aligning with routine hospital quality assurance activities.
RESULTS
The IPE course on delirium management was conducted in August 2023, with a follow-up evaluation meeting held on October 3, 2023. The participant group comprised 16 clinicians: 50% registered nurses (n=8), 37.5% therapists (n=6), and 12.5% physicians (n=2). Participants represented various disciplines and departments, including the emergency department, intensive care unit, geriatric acute ward, neurological ward, stroke unit, and interdisciplinary physiotherapy and occupational therapy services.
Development of the projects
Throughout the IPE course, participants had numerous opportunities for interaction and were actively encouraged to initiate practice changes. They expressed appreciation for the interprofessional and interdisciplinary discussions, which facilitated the sharing of diverse perspectives and ideas. Ultimately, participants formed five distinct project groups. Initially, the groups focused on identifying barriers to effective delirium management. These barriers were categorized into organizational (e.g., staff shortages, lack of documentation systems), local (e.g., time constraints, infrequent delirium assessments), and clinician-related factors (e.g., knowledge gaps, negative attitudes). Table 1 summarizes these reported barriers. The diverse perspectives of nurses, physicians, and therapists on these barriers facilitated the development of targeted solutions. The groups then collaboratively developed feasible project ideas that were SMART: Specific, Measurable, Achievable, Realistic, and Timely.
Table 1. Barriers Reported by Participating Clinicians
| Organizational Barriers | Local Barriers | Clinician Barriers |
|---|---|---|
| Staff shortage | Time pressure | Missing interest and knowledge |
| Missing documentation | No frequent assessment | Missing feedback |
| Priority of routine care | Delirium not discussed during rounds | Complaining attitude |
| Missing training | Missing protocols and flyers | Feeling shy to perform assessment |
| Short length of stay | Anxious for delirious patients | |
| Missing prioritization of delirium |
Details of the process measures and outcome
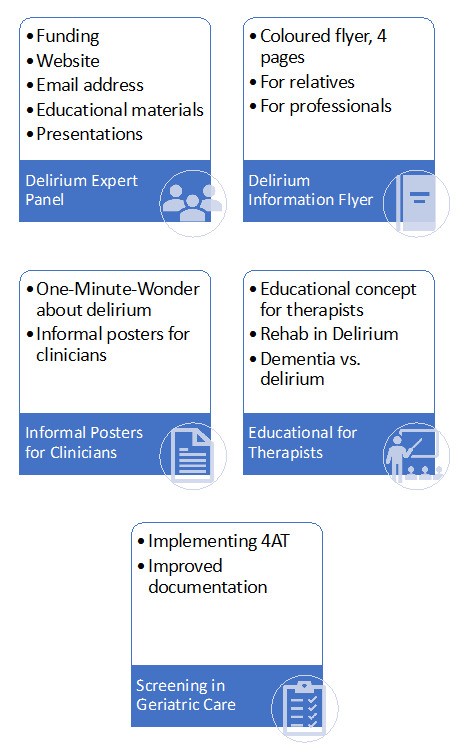
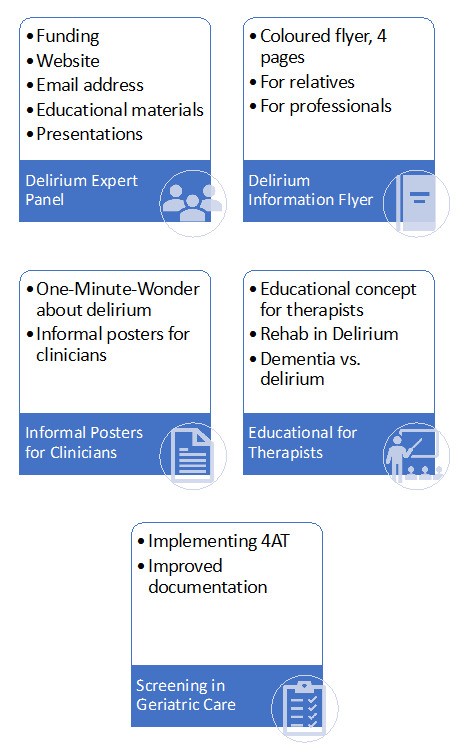
Participants formed five project groups, each focusing on a distinct aspect of delirium management improvement:
- Project Delirium Expert Panel: This project aimed to establish a structured plan for an interprofessional expert group within the hospital to champion delirium care. By the eight-week follow-up, the group had developed a comprehensive project plan for the upcoming year. Key components included establishing an online presence, disseminating delirium-related information to hospital staff, recruiting additional members to the panel, organizing interprofessional team training, and creating educational materials for both staff and family caregivers.
- Project Delirium Flyer: The objective was to design and produce an informative flyer for relatives of patients experiencing delirium, particularly within intensive care units. The group presented a draft of a full-color, folded flyer containing essential delirium information, guidance on what relatives could expect, and practical advice on how they could support patients. The design elements were thoughtfully developed. Following group discussion, the scope of the flyer was expanded to be relevant across the entire hospital, not just intensive care units.
- Project Team Education: This project focused on enhancing delirium education for multidisciplinary and multiprofessional teams throughout the hospital. The group developed a concise, one-page summary sheet on delirium. This resource was designed to be easily printable as a flyer, suitable for display on walls, and to serve as a quick reference point, directing staff to more detailed information provided by the delirium expert panel.
- Project Training for Therapists: Recognizing the crucial role of therapists in delirium care, this project aimed to develop a specialized training session for therapists. Given the hospital’s centralized organization of therapists, the training was designed to cover general delirium knowledge applicable to various patient populations across the hospital. Specific topics included differentiating delirium from dementia, utilizing the 4AT screening tool for delirium assessment in therapy settings, and implementing therapeutic interventions focused on patient safety and supportive care.
- Project 4AT Assessment in Geriatric Acute Ward: This project focused on the implementation of routine delirium assessments using the 4AT tool within the geriatric acute ward. The project group engaged with the IT department to integrate the 4AT assessment into the hospital’s electronic patient charts. This integration process, while time-consuming, was seen as crucial for supporting hospital-wide adoption of standardized delirium assessment. In the interim, the group explored the use of paper-based documentation sheets for recording 4AT assessments. This project was ongoing at the eight-week evaluation, demonstrating progress but not full completion within the defined timeframe.
Figure 1. Projects
Contextual elements that interacted with the intervention(s)
During the final discussion session, participants provided overwhelmingly positive feedback on the IPE course. They reported significant improvements in their knowledge and attitudes towards delirium management and interprofessional care delirium diagnosis. Participants expressed satisfaction with the course structure, process, content, and teaching methods. They also indicated increased confidence in their ability to provide care for patients with delirium and to undertake quality improvement projects within their hospital. Suggestions for further enhancing the learning experience included incorporating training in a simulation center or using actors to simulate interactions with patients experiencing delirium.
Observed associations between outcomes, interventions, and relevant contextual elements
At the project’s outset, basic delirium prevention measures, such as providing vision and hearing aids, calendars, and clocks, were generally in place. However, consistent delirium awareness and standardized management practices were variably implemented across departments. Delirium screening frequency differed, being irregular in general wards but routinely performed three times daily in intensive care units. In the emergency room, the primary focus was on managing severe hyperactive delirium. In general wards, delirium superimposed on dementia was identified as a major challenge, while in intensive care units, appropriate pharmacological treatment strategies were a key concern. The response to positive delirium assessments also varied across departments and professions, potentially influenced by the quality of interprofessional communication. Despite differing needs and priorities across settings, participants benefited significantly from interdisciplinary discussions and shared solution development. Following the initial two-day IPE course, participants demonstrated heightened delirium awareness, began integrating delirium screening into their daily routines, actively sought interprofessional communication, and acted as advocates for improved delirium care within their teams.
Further observations
Following the initial training days, participants reported that their colleagues showed considerable interest in their experiences, providing an opportunity for participants to disseminate information about delirium and raise overall awareness among hospital staff.
Participants also noted challenges in reconciling the ideals presented in the training with the realities of daily practice. These challenges included difficulties in consistently performing accurate delirium assessments, effectively communicating across professions, and navigating existing structural limitations within the hospital system.
Details about missing data
The interactive and dynamic nature of the project, while beneficial for engagement and learning, made it challenging to systematically collect data on all potentially relevant aspects of the quality improvement process. This inherent limitation meant that some potentially valuable data points related to the nuances of project implementation were not captured.
DISCUSSION
This quality improvement project demonstrated that a two-day DIVI-certified IPE course on delirium management effectively equipped participants to assess local barriers and develop targeted improvement projects for their hospital wards and units. Remarkably, within eight weeks of course completion, four out of five clinician groups successfully presented projects that were not only implemented but also sustained. These projects included establishing a hospital delirium expert panel, creating delirium information flyers for families, developing a one-page delirium information sheet for clinicians, and designing a therapist training program. The implementation of the 4AT assessment in electronic patient charts was the only project still in progress at the evaluation point. Furthermore, participants reported high levels of satisfaction with the IPE course and expressed increased confidence in their ability to care for patients with delirium and enhance interprofessional care delirium diagnosis.
The IPE course for delirium management effectively targeted interdisciplinary and interprofessional hospital staff. Delirium management training is crucial for improving patient care, and its effectiveness is enhanced through regular, ongoing education. Sustaining this training and ensuring it reflects the most current knowledge are equally important. The DIVI-certified delirium expert training model emphasizes current specialist knowledge and promotes a proactive, delirium-focused approach through enhanced interprofessional communication and collaboration. A key strength of this IPE course was its emphasis on practical application. Participants were not only trained but also guided to develop and implement projects using the PDCA cycle within small groups over eight weeks. This structured approach facilitated the translation of acquired knowledge into tangible improvements in practice. This hands-on, project-based methodology may be more effective than traditional, purely didactic training methods.
The PDCA cycle integrated into the training significantly facilitated the initial project implementations. Key factors for success included establishing an appropriate timeframe for project completion and ensuring active participation from all involved staff members. Identifying and openly discussing barriers within the specific local context was essential for developing feasible and practical solutions. One identified barrier was the need for ongoing training and structural improvements within the hospital to support sustained delirium management efforts. Enhancing interprofessional and interdisciplinary collaboration, another critical area, can be achieved through strategies such as shared daily rounds, implementation of quality indicators, and consistent documentation of daily care goals. Moving forward, it is essential to assess not only participant satisfaction with training programs but also the long-term sustainability of implemented strategies and the overall well-being of healthcare professionals involved in delirium care. Specific clinical areas, such as stroke and neurological units, may require tailored approaches to delirium management. To ensure ongoing improvement, follow-up audits and routine monitoring of implemented strategies are necessary.
At this stage of the project, a comprehensive cost-effectiveness evaluation was not feasible.
Strengths and Limitations
This project has several notable strengths: a) It employed a structured, interactive QI methodology involving clinicians from diverse wards and units across the hospital, leveraging intrinsic motivation and interdisciplinary expertise. b) The project’s detailed documentation ensures transparent reporting of each stage of the quality improvement process. c) The project received strong support from hospital management, who recognized the value of developing a delirium-specific QI group.
The generalizability of the findings is subject to certain limitations: a) IPE-related factors, such as teaching methods, the level of interaction, the allocated time, and individual presenter styles, may have variably influenced participant learning, although feedback was overwhelmingly positive, suggesting this limitation may be minor. b) The specific setting—a university-affiliated hospital in East Germany—and its unique culture and team communication dynamics may limit the direct transferability of results to other settings and cultures. c) Most of the reported projects focused on the initial planning stages, which, while crucial for establishing structures and processes in hospital-wide initiatives, represent an early phase of impact. d) The long-term sustainability and broader impact of these projects on patient outcomes, staff well-being, economic factors, and societal benefits remain unproven at this early stage, although ongoing follow-up by the research team is intended to address this.
CONCLUSIONS
The IPE course on delirium management successfully motivated and empowered participating clinicians to develop and implement delirium-specific quality improvement projects within their hospital. Further research is needed to rigorously evaluate the long-term sustainability of these projects and to quantify the impact of contextual factors on their success across different healthcare settings and organizational cultures. Future steps will focus on establishing robust delirium management protocols, disseminating knowledge and best practices, continuously improving the quality of delirium care, and comprehensively evaluating the realized benefits of these initiatives for patients and healthcare systems.
Acknowledgement
The authors extend their sincere gratitude to all participating healthcare professionals whose dedication and engagement were essential to the success of this quality improvement project.
Contributions
All authors (FS, VH, UG, HCH, TD, RvH, CH, CHo, AK, SP, and PN) made substantial contributions to the conception and design of the work; FS, VH, and PN drafted the manuscript; UG, HCH, TD, RvH, CH, CHo, AK, and SP critically revised it for important intellectual content; all authors (FS, VH, UG, HCH, TD, RvH, CH, CHo, AK, SP, and PN) approved the final submitted version and agreed to be accountable for all aspects of the work.
Ethic approval and registration
This quality improvement project was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. Given its nature as a service evaluation and quality improvement initiative, formal ethics approval was not required.
Funding
This research received no specific funding.
Declaration of Interests
The authors declare no conflicts of interest related to this work.
Submitted: November 23, 2023 CEST
Accepted: February 01, 2024 CEST
References
- Kuusisto-Gussmann E, Höckelmann C, von der Lühe V, Schmädig R, Baltes M, Stephan A. Patients’ experiences of delirium: A systematic review and meta-summary of qualitative research. J Adv Nurs. 2021;77(9):3692-3706. doi:10.1111/jan.14865
- Wilson JE, Mart MF, Cunningham C, et al. Delirium. Nat Rev Dis Primers. 2020;6(1):90. doi:10.1038/s41572-020-00223-4
Google ScholarPubMed CentralPubMed
- Ormseth CH, LaHue SC, Oldham MA, Josephson SA, Whitaker E, Douglas VC. Predisposing and Precipitating Factors Associated With Delirium: A Systematic Review. JAMA Netw Open. 2023;6(1):e2249950. doi:10.1001/jamanetworkopen.2022.49950
Google ScholarPubMed CentralPubMed
-
National Institute for Health and Clinical Excellence (NICE). DELIRIUM: diagnosis, prevention and management. Clinical guideline 103. 2010. https://www.nice.org.uk/guidance/cg103
-
Adamis D, Macdonald A, McCarthy G, Morandi A, Bellelli G, Meagher D. Towards understanding the nature and need of delirium guidelines across nations and cultures. Aging Clin Exp Res. 2022;34(3):633-642. doi:10.1007/s40520-021-01978-w
Google ScholarPubMed CentralPubMed
- Aldecoa C, Bettelli G, Bilotta F, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192-214. doi:10.1097/eja.0000000000000594
- Bellelli G, Morandi A, Zanetti E, et al. Recognition and management of delirium among doctors, nurses, physiotherapists, and psychologists: an Italian survey. Int Psychogeriatr. 2014;26(12):2093-2102. doi:10.1017/s1041610214001653
- Davis D, Searle SD, Tsui A. The Scottish Intercollegiate Guidelines Network: risk reduction and management of delirium. Age Ageing. 2019;48(4):485-488. doi:10.1093/ageing/afz036
- Trogrlić Z, Ista E, Ponssen HH, et al. Attitudes, knowledge and practices concerning delirium: a survey among intensive care unit professionals. Nurs Crit Care. 2016;22(3):133-140. doi:10.1111/nicc.12239
- Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in Older Persons: Advances in Diagnosis and Treatment. JAMA. 2017;318(12):1161-1174. doi:10.1001/jama.2017.12067
Google ScholarPubMed CentralPubMed
- Yürek F, Lachmann C. Postoperatives Delir [Postoperative Delirium]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2023;58(09):480-481. doi:10.1055/a-2127-8081
- Morandi A, Piva S, Ely EW, et al. Worldwide Survey of the “Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Drugs, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Empowerment” (ABCDEF) Bundle. Crit Care Med. 2017;45(11):e1111-e1122. doi:10.1097/ccm.0000000000002640
Google ScholarPubMed CentralPubMed
- Nydahl P, Dewes M, Dubb R, et al. Survey among critical care nurses and physicians about delirium management. Nurs Crit Care. 2018;23(1):23-29. doi:10.1111/nicc.12299
- Sahawneh F, Boss L. Non-pharmacologic interventions for the prevention of delirium in the intensive care unit: An integrative review. Nurs Crit Care. 2021;26(3):166-175. doi:10.1111/nicc.12594
- Trogrlić Z, van der Jagt M, Bakker J, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care. 2015;19(1):157. doi:10.1186/s13054-015-0886-9
Google ScholarPubMed CentralPubMed
- Kotfis K, van Diem-Zaal I, Roberson SW, et al. The future of intensive care: delirium should no longer be an issue. Crit Care. 2022;26(1):200. doi:10.1186/s13054-022-04077-y
Google ScholarPubMed CentralPubMed
- Luetz A, Balzer F, Radtke FM, et al. Delirium, sedation and analgesia in the intensive care unit: a multinational, two-part survey among intensivists. PLoS One. 2014;9(11):e110935. doi:10.1371/journal.pone.0110935
Google ScholarPubMed CentralPubMed
- Luz M, Brandão Barreto B, de Castro REV, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Ann Intensive Care. 2022;12(1):9. doi:10.1186/s13613-022-00985-y
Google ScholarPubMed CentralPubMed
- Mo Y, Zimmermann AE, Thomas MC. Practice Patterns and Opinions on Current Clinical Practice Guidelines Regarding the Management of Delirium in the Intensive Care Unit. J Pharm Pract. 2016;30(2):162-171. doi:10.1177/0897190015625396
- Paulino MC, Pereira IJ, Costa V, et al. Sedation, analgesia, and delirium management in Portugal: a survey and point prevalence study (Abordagem da sedação, da analgesia e do delirium em Portugal: inquérito nacional e estudo de prevalência). Rev Bras Ter Intensiva. 2022;34(2):227-236. doi:10.5935/0103-507x.20220020-pt
-
Centre for the Advancement of Interprofessional Education. CAIPE Statement of Purpose. 2016. Accessed January 15, 2024. https://www.CAIPE-Statement-of-Purpose-2016.pdf
-
Paul N, Grunow JJ, Rosenthal M, et al. Enhancing European Management of Analgesia, Sedation, and Delirium: A Multinational, Prospective, Interventional Before-After Trial. Neurocrit Care. Published online September 11, 2023. doi:10.1007/s12028-023-01837-8
- de Souza-Talarico JN, da Silva FC, de Motta Maia FO, et al. Screening and detection of delirium in an adult critical care setting: a best practice implementation project. JBI Evid Implement. 2021;19(4):337-346. doi:10.1097/xeb.0000000000000267
- Kamdar BB, Makhija H, Cotton SA, et al. Development and Evaluation of an Intensive Care Unit Video Series to Educate Staff on Delirium Detection. ATS Sch. 2022;3(4):535-547. doi:10.34197/ats-scholar.2022-0011oc
Google ScholarPubMed CentralPubMed
- Makhija H, Fine JM, Pollack D, et al. Development and Validation of an ICU Delirium Playbook for Provider Education. Crit Care Explor. 2023;5(7):e0939. doi:10.1097/cce.0000000000000939
Google ScholarPubMed CentralPubMed
- Nydahl P, Deffner T, Günther U, et al. DIVI Curriuculum Delirium Management (German: Das DIVI-Curriculum Delirmanagement). DIVI. 2023;14(2):14-15.
- Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986-992. doi:10.1136/bmjqs-2015-004411
Google ScholarPubMed CentralPubMed
- Barr J, Paulson SS, Kamdar B, et al. The Coming of Age of Implementation Science and Research in Critical Care Medicine. Crit Care Med. 2021;49(8):1254-1275. doi:10.1097/ccm.0000000000005131
Google ScholarPubMed CentralPubMed
- Moraes FDS, Marengo LL, Moura MDG, et al. ABCDE and ABCDEF care bundles: A systematic review of the implementation process in intensive care units. Medicine. 2022;101(25):e29499. doi:10.1097/md.0000000000029499
Google ScholarPubMed CentralPubMed
- van Bochove-Waardenburg M, van der Jagt M, de Man-van Ginkel J, Ista E. Sustained adherence to a delirium guideline five years after implementation in an intensive care setting: A retrospective cohort study. Intensive Crit Care Nurs. 2023;76:103398. doi:10.1016/j.iccn.2023.103398
- Kumpf O, Assenheimer M, Bloos F, et al. Quality indicators in intensive care medicine for Germany – fourth edition 2022. Ger Med Sci. 2023;21:Doc10. doi:10.3205/000324
Google ScholarPubMed CentralPubMed
- Morandi A, Di Santo SG, Zambon A, et al. Delirium, Dementia, and In-Hospital Mortality: The Results From the Italian Delirium Day 2016, A National Multicenter Study. J Gerontol A Biol Sci Med Sci. 2019;74(6):910-916. doi:10.1093/gerona/gly154
- Vater V, Olm HP, Nydahl P. Delirium in stroke: systematic review and meta-analysis (Delir bei Schlaganfall: systematisches Review und Metaanalyse). Med Klin Intensivmed Notfmed. 2023;119(1):49-55. doi:10.1007/s00063-023-01013-y