Left Bundle Branch Block (LBBB) is a significant finding on an electrocardiogram (ECG) that indicates a delay or blockage in the electrical conduction pathway of the heart’s left ventricle. Accurate diagnosis of LBBB is crucial as it can be associated with underlying cardiac conditions and can affect the interpretation of ST-segment changes, particularly in the context of myocardial ischemia. This article will delve into the ECG diagnostic criteria for LBBB, its electrophysiological basis, and key features for accurate interpretation.
The ECG criteria for diagnosing LBBB are specific and readily identifiable on a standard 12-lead ECG. The primary diagnostic features include:
- QRS duration ≥ 120 milliseconds: This is a hallmark of LBBB, indicating prolonged ventricular depolarization due to delayed conduction in the left bundle branch.
- Dominant S wave in lead V1: In lead V1, which reflects right ventricular activity, a deep and prominent S wave is observed as the left ventricle depolarizes late.
- Broad monophasic R wave in lateral leads (I, aVL, V5-V6): Lateral leads, representing the left ventricle, show a wide, single peaked R wave, reflecting the slow and delayed depolarization of the left ventricle.
- Absence of Q waves in lateral leads (I, aVL, V5-V6): Normally, small Q waves represent septal depolarization from left to right. In LBBB, septal depolarization is reversed, leading to the absence of these Q waves in lateral leads.
- Prolonged R wave peak time > 60 milliseconds in leads V5-V6: The time it takes to reach the peak of the R wave in lateral leads is prolonged, reflecting the delayed left ventricular activation.
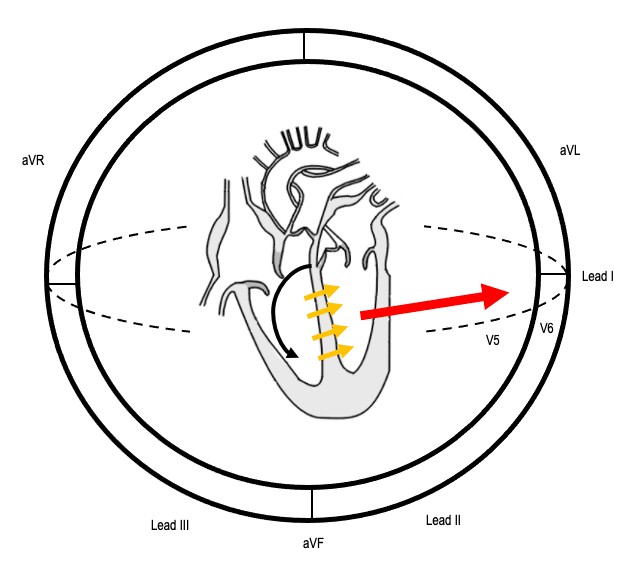
Image alt text: ECG conduction sequence in Left Bundle Branch Block illustrating initial right bundle branch impulse, reversed septal activation, and lateral depolarization vector.
Understanding the electrophysiology of LBBB is key to grasping these ECG changes. In a normal heart, electrical impulses travel simultaneously down both the left and right bundle branches. In LBBB, a block in the left bundle branch forces the electrical impulse to travel initially through the right bundle branch, depolarizing the right ventricle first. The impulse then spreads to the left ventricle via slower cell-to-cell conduction across the septum. This altered sequence of depolarization explains the characteristic ECG findings. Normally, septal activation occurs from left to right, generating small Q waves in lateral leads. However, in LBBB, the septum depolarizes from right to left, eliminating these typical lateral Q waves. The overall depolarization vector shifts, producing tall R waves in lateral leads (I, aVL, V5-V6) and deep S waves in right precordial leads (V1-V3). The delay in left ventricular activation also extends the QRS duration beyond 120ms and results in the notched or “M-shaped” appearance of the R wave in some cases, especially in lateral leads.
The morphology of the QRS complex in LBBB can vary slightly, particularly in the lateral leads. The R wave in leads I, aVL, V5, and V6 might present as “M-shaped,” notched, monophasic, or even as an RS complex in some instances.
Image alt text: ECG showing M-shaped QRS morphology in lateral leads indicative of Left Bundle Branch Block.
Image alt text: ECG demonstrating monophasic R wave QRS morphology in lateral leads consistent with Left Bundle Branch Block.
In lead V1, the QRS complex in LBBB typically presents as either an rS complex (a small R wave followed by a deep S wave) or a QS complex (a deep Q/S wave with no preceding R wave). The rS complex is more common, characterized by a small initial upward deflection (r wave) representing right ventricular depolarization, immediately followed by a large downward deflection (S wave) as the left ventricle depolarizes later.
A crucial aspect of ECG interpretation in LBBB is understanding “appropriate discordance.” This principle refers to the expected repolarization changes that occur secondary to abnormal depolarization. In LBBB, the abnormal depolarization is followed by altered repolarization, manifesting as ST-segment and T-wave changes that are typically discordant to the QRS complex. Specifically, lateral leads with tall, broad R waves often exhibit ST-segment depression and T-wave inversion. Conversely, leads with deep S waves, like V1-V3, can show some degree of ST elevation as a normal finding in LBBB. However, any concordant ST-segment changes, where the ST segment shift is in the same direction as the major QRS deflection, should raise suspicion for myocardial ischemia and warrant further investigation. For example, ST elevation in leads with upright QRS complexes in LBBB is highly concerning for acute myocardial infarction.
Image alt text: ECG of Left Bundle Branch Block with Atrial Fibrillation demonstrating appropriate discordance with ST depression in lateral leads and ST elevation in V2-V3.
LBBB is rarely found in individuals without underlying heart disease. The causes of LBBB are diverse and include structural heart diseases, ischemic heart disease, and conduction system diseases. Common etiologies include:
- Aortic stenosis
- Ischemic heart disease
- Hypertension
- Dilated cardiomyopathy
- Anterior Myocardial Infarction
- Lenègre-Lev disease (degenerative disease of the conducting system)
- Hyperkalemia
- Digoxin toxicity
Historically, new-onset LBBB in the setting of chest pain was considered a STEMI equivalent, prompting immediate reperfusion therapy. However, current evidence suggests that isolated new LBBB in chest pain patients does not uniformly indicate acute myocardial infarction. The focus has shifted to identifying high-risk features, such as excessive ST-segment discordance or concordant ST changes using criteria like the Sgarbossa criteria, to determine the likelihood of acute ischemia in patients with LBBB.
Incomplete LBBB is diagnosed when the ECG shows typical LBBB morphology but the QRS duration is less than 120 milliseconds. It shares similar QRS morphology features but with a less pronounced conduction delay.
Image alt text: ECG example of Incomplete Left Bundle Branch Block showing LBBB morphology with QRS duration less than 120ms.
It’s important to differentiate LBBB from other conditions that can mimic its ECG appearance. Right ventricular paced rhythms can produce a similar morphology because the ventricular depolarization sequence is also initiated from the right ventricle, spreading to the left ventricle. However, pacing spikes preceding the QRS complexes will be present in paced rhythms. Left ventricular hypertrophy (LVH) can also exhibit QRS widening and ST-T wave changes in lateral leads, but typically lacks the specific QRS morphology of LBBB.
In conclusion, accurate diagnosis of LBBB relies on recognizing specific ECG criteria, understanding its electrophysiological basis, and differentiating it from similar conditions. Key diagnostic features include QRS duration ≥ 120ms, dominant S wave in V1, broad R waves in lateral leads without Q waves, and prolonged R wave peak time. Recognizing appropriate discordance is vital for interpreting ST-segment changes in LBBB and identifying potential myocardial ischemia. LBBB is often associated with underlying cardiac disease, and its ECG recognition is a critical skill in clinical cardiology.