Parkinson’s Disease (PD) is the second most prevalent neurodegenerative disorder, affecting millions worldwide. A common concern for individuals diagnosed with Parkinson’s, and their families, revolves around life expectancy. While Parkinson’s disease does impact longevity, understanding the factors involved can provide clarity and inform expectations. This article delves into what current research indicates about life expectancy after a Parkinson’s diagnosis, drawing upon a comprehensive study to provide insights into prognosis and related risk factors.
Parkinsonism and Survival Rates: An Overview
Idiopathic parkinsonism encompasses a group of neurological conditions that share similar symptoms with Parkinson’s disease, including slowness of movement, rigidity, tremor, and postural instability. These conditions include Parkinson’s disease itself, as well as atypical parkinsonian disorders such as Multiple System Atrophy (MSA) and Progressive Supranuclear Palsy (PSP). Research has consistently shown that individuals with idiopathic parkinsonism experience reduced survival compared to the general population.
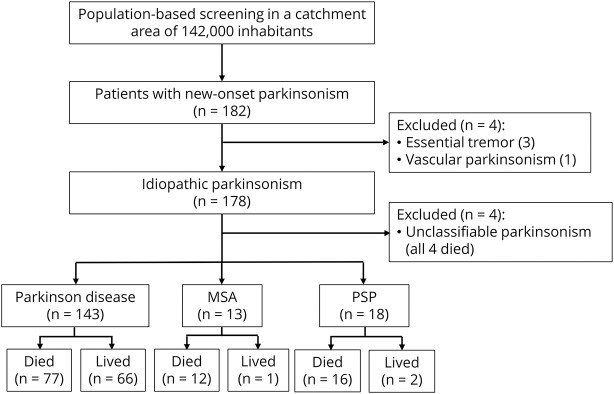
A significant population-based study conducted in Sweden aimed to investigate mortality rates and associated risk factors in individuals newly diagnosed with idiopathic parkinsonism. This study, which followed 182 patients for over a decade, provides valuable data on life expectancy in this patient group.
Key Findings on Parkinsonism and Life Expectancy:
- Reduced Survival: The study confirmed that individuals with idiopathic parkinsonism have a significantly higher mortality rate than the general population. The standardized mortality ratio (SMR) was found to be 1.84, meaning the death rate was 1.84 times higher than expected in a similar population without parkinsonism.
- Diagnosis Matters: Survival rates varied significantly depending on the specific diagnosis within parkinsonism. Patients with atypical parkinsonism (MSA and PSP) had a considerably worse prognosis compared to those with Parkinson’s disease.
- Parkinson’s Disease Survival: While Parkinson’s disease does reduce life expectancy compared to the general population (SMR of 1.58 in the study), the reduction is less pronounced than in atypical parkinsonism.
Figure 1: Patient Flowchart illustrating the diagnostic breakdown of participants in the study, highlighting the different categories within idiopathic parkinsonism.
Factors Influencing Life Expectancy in Parkinson’s Disease
While a Parkinson’s disease diagnosis does impact life expectancy on average, it’s crucial to understand that this is not a uniform outcome. Several factors can significantly influence an individual’s prognosis after being diagnosed with Parkinson’s. The Swedish study identified several key predictors of survival in PD patients.
Cognitive Function: A Critical Factor
One of the most significant findings of the study was the impact of cognitive function at the time of Parkinson’s diagnosis. Patients were categorized based on whether they had mild cognitive impairment (PD-MCI) at baseline or normal cognition.
- PD with Normal Cognition: Remarkably, the study found that individuals with Parkinson’s disease who presented with normal cognitive function at diagnosis had a life expectancy that was not significantly different from the general Swedish population. In fact, male patients in this group even showed a standardized mortality ratio below 1, suggesting a potentially longer life expectancy than the average.
- PD with Mild Cognitive Impairment (PD-MCI): In stark contrast, patients diagnosed with PD-MCI at baseline had a significantly reduced life expectancy. Their standardized mortality ratio was 2.17, and they faced a 2.4 times higher age-adjusted risk of death compared to PD patients with normal cognition.
This highlights the critical role of cognitive status in determining the long-term outlook for individuals with Parkinson’s disease. Early identification and management of cognitive issues in Parkinson’s are therefore of paramount importance.
Age at Diagnosis and Overall Health
Age at diagnosis is naturally a significant factor in life expectancy for any condition, including Parkinson’s. Older individuals at diagnosis will, on average, have a shorter remaining life span, regardless of Parkinson’s. The study confirmed that older age at the first visit was associated with a higher hazard ratio for death across all parkinsonism types.
However, it is important to note that within Parkinson’s disease itself, age may be less of a determining factor than other elements like cognitive status and disease phenotype. Overall health and the presence of other comorbidities will also play a role in individual life expectancy.
Motor and Non-Motor Symptoms
The severity and type of Parkinson’s symptoms also influence prognosis. The study examined various motor and non-motor features at baseline to determine their predictive value for survival.
- Gait and Balance Issues: Symptoms related to postural instability and gait disorder (PIGD), such as freezing of gait and balance problems, were associated with shorter survival. This is likely due to the increased risk of falls and related complications, such as pneumonia, which was identified as a common cause of death in the study.
- Hyposmia (Reduced Sense of Smell): Severe hyposmia, or a significantly reduced sense of smell, was also found to be a predictor of shorter survival in Parkinson’s disease. Hyposmia is a common non-motor symptom of PD, and its association with prognosis may reflect underlying disease severity or specific disease subtypes.
- Disease Severity: Higher scores on the Unified Parkinson’s Disease Rating Scale (UPDRS), particularly the motor section (Part III), at baseline were indicative of a poorer prognosis. This suggests that the overall burden of Parkinson’s symptoms at diagnosis is related to life expectancy.
- Tremor: Interestingly, tremor, often considered a hallmark symptom of Parkinson’s, was not found to be correlated with survival in this study. This suggests that while tremor is a defining feature of PD, other symptom domains may be more critical determinants of long-term outcome.
Figure 2: Kaplan-Meier survival curves illustrating the differences in survival probability between Parkinson’s Disease and Atypical Parkinsonism (MSA/PSP) diagnostic groups.
Dopamine Transporter Imaging and Neurobiological Factors
The study utilized dopamine active transporter (DAT) imaging, a specialized scan that reflects the level of dopamine activity in the brain, to investigate neurobiological predictors of survival.
- Reduced DAT Uptake: Lower DAT uptake in the striatum, particularly in the caudate nucleus region of the brain, was associated with a shorter survival in Parkinson’s disease. This finding suggests that the extent of dopamine neuron degeneration, as measured by DAT imaging, is related to prognosis. The more significant the dopamine deficiency, the potentially poorer the long-term outlook.
- CSF Leukocytosis: An intriguing finding was the association between a subtle increase in mononuclear leukocytes (a type of white blood cell) in the cerebrospinal fluid (CSF) and reduced survival. While only a small percentage of PD patients (13.1%) exhibited this CSF leukocytosis, it was a strong predictor of mortality, with a 6.31 times increased risk of death. This could indicate an inflammatory component in certain Parkinson’s cases that contributes to disease progression and reduced life expectancy.
Figure 3: Kaplan-Meier survival curves highlighting the impact of various phenotypes within Parkinson’s Disease on survival probability, including cognitive impairment, gait issues, and sense of smell.
Implications for Parkinson’s Disease Prognosis and Management
This comprehensive study provides valuable insights into life expectancy after a Parkinson’s disease diagnosis and highlights the importance of considering various factors beyond just the diagnosis itself.
Key Takeaways for Understanding Parkinson’s Prognosis:
- Parkinson’s Disease is Variable: Life expectancy after a Parkinson’s diagnosis is not fixed. It varies significantly based on individual factors, particularly cognitive status at diagnosis.
- Normal Life Expectancy Possible: Individuals with Parkinson’s disease who maintain normal cognitive function at diagnosis may have a largely normal life expectancy. This is a crucial point of hope and reassurance for many newly diagnosed patients.
- Cognitive Impairment is a Major Prognostic Factor: Early detection and management of cognitive impairment in Parkinson’s are critical for improving overall outcomes and potentially influencing life expectancy.
- Multifaceted Approach to Prognosis: Prognosis in Parkinson’s is influenced by a combination of factors, including age, cognitive status, motor and non-motor symptoms, neurobiological markers, and potentially inflammatory processes.
- Continued Research Needed: Further research is essential to validate these findings, explore the mechanisms behind these prognostic factors, and develop targeted interventions to improve life expectancy and quality of life for individuals with Parkinson’s disease.
Living Well with Parkinson’s Disease:
While Parkinson’s disease does impact life expectancy, focusing solely on survival statistics can be detrimental to quality of life. It is important to remember that:
- Treatment Advances: Medical treatments for Parkinson’s disease have advanced significantly, helping to manage symptoms and improve quality of life.
- Lifestyle Modifications: Lifestyle factors such as exercise, healthy diet, and social engagement can play a vital role in managing Parkinson’s and promoting overall well-being.
- Individualized Care: Parkinson’s care should be individualized, taking into account each person’s unique circumstances, symptoms, and goals.
- Focus on Quality of Life: While life expectancy is a consideration, focusing on maximizing quality of life and living well with Parkinson’s is paramount.
Conclusion:
Understanding life expectancy after a Parkinson’s disease diagnosis requires considering a range of factors, with cognitive status at diagnosis emerging as a particularly critical determinant. While Parkinson’s can reduce life expectancy, especially in the presence of cognitive impairment or atypical parkinsonism, many individuals with Parkinson’s, particularly those with normal cognition at diagnosis, can expect to live a long and fulfilling life. Continued research and advancements in treatment offer hope for further improving prognosis and enhancing the lives of those affected by Parkinson’s disease.
Disclaimer: This article is for informational purposes only and does not provide medical advice. Individuals with Parkinson’s disease should consult with their healthcare providers for personalized guidance on diagnosis, treatment, and prognosis. This article is based on the research study cited as the original source and aims to present the study findings in an accessible format for a general audience.