Amyotrophic Lateral Sclerosis (ALS), often referred to as Lou Gehrig’s disease, is a challenging neurodegenerative condition that affects motor neurons, the nerve cells controlling voluntary muscle movement. At the ALS Program at the Hospital for Special Surgery, a designated ALS Certified Center of Excellence, we are committed to providing comprehensive care, from in-person and telehealth consultations to cutting-edge treatment research and clinical trials. Understanding the prognosis, particularly concerning life expectancy with an ALS diagnosis, is crucial for patients and their families. This article aims to provide a detailed overview of ALS, focusing on what to expect regarding life expectancy and the factors that influence it.
Demystifying ALS: A Progressive Motor Neuron Disease
ALS is characterized as a progressive disease, meaning its symptoms worsen over time. It targets motor neurons, which extend from the brain through the brainstem and spinal cord to muscles throughout the body. These neurons are responsible for movements we consciously control, such as walking, speaking, breathing, and swallowing. In ALS, these motor neurons degenerate and die, leading to muscle weakness, atrophy, and eventually paralysis. Importantly, ALS typically does not impair sensory functions or cognitive abilities; individuals retain their senses and mental sharpness even as the disease progresses.
ALS is broadly classified into two categories based on the location of affected motor neurons:
- Upper Motor Neuron Disease: Impacts motor neurons in the brain.
- Lower Motor Neuron Disease: Affects motor neurons originating from the spinal cord or brainstem.
In both types, the damage to motor neurons is irreversible and ultimately fatal.
Navigating Life Expectancy After an ALS Diagnosis
One of the most pressing concerns for individuals diagnosed with ALS and their loved ones is life expectancy. It’s essential to understand that life expectancy with an ALS diagnosis is highly variable and depends on numerous factors. While the average life expectancy after diagnosis is generally cited as two to five years, this is just an average. Statistics show a broader picture:
- 50% of individuals with ALS live for at least three years following their diagnosis.
- 25% live for five years or more.
- Up to 10% may live for more than ten years.
Exceptional cases, like that of the renowned physicist Stephen Hawking, who lived for over 50 years after his ALS diagnosis, demonstrate the wide spectrum of disease progression. These figures underscore that while ALS is a serious condition, the course of the disease varies significantly from person to person. Therefore, focusing solely on average life expectancy can be misleading and may not accurately reflect an individual’s potential prognosis.
Recognizing the Symptoms of ALS
The manifestation and progression of ALS symptoms are unique to each individual, depending on the specific proportion of upper and lower motor neurons affected. This variability means the initial symptoms can differ considerably, as can the rate at which the disease advances. Despite these individual differences, progressive muscle weakness and paralysis are universal experiences for all people with ALS.
As ALS progresses, the deterioration of nerve cells leads to muscle atrophy and weakness, often making limbs appear thinner. Paradoxically, muscles can also become spastic, leading to involuntary movements and increased muscle tone in certain areas of the body.
Early symptoms of ALS can be subtle and easily overlooked. Common early indicators include:
- Muscle Weakness: Particularly in the hands, arms, or legs.
- Impaired Limb Function: Difficulty using arms and legs for daily activities.
- Muscle Twitching and Cramping: Especially in the hands and feet.
- Speech and Swallowing Difficulties: Weakness in muscles controlling speech, swallowing, and breathing.
- Speech Changes: Slow or slurred speech (dysarthria) and reduced voice projection.
In later stages, ALS leads to severe breathing and swallowing difficulties, which are often the ultimate causes of mortality associated with the disease.
Unraveling the Causes of ALS
The precise cause of ALS remains incompletely understood, but current research points to a complex interplay of factors contributing to motor neuron degeneration. While specific risk factors are still under investigation, research is actively exploring the roles of genetics and environmental influences. Notably, a 2009 study suggested a potential link between tobacco smoking and an increased risk of ALS.
Several biological mechanisms are considered potentially responsible for the development of ALS:
- Defective Glutamate Metabolism: Imbalances in glutamate, a neurotransmitter.
- Free Radical Injury: Damage from unstable molecules.
- Mitochondrial Dysfunction: Problems with cellular energy production.
- Gene Defects: Genetic mutations.
- Apoptosis: Programmed cell death.
- Cytoskeletal Protein Defects: Issues with cell structure.
- Autoimmune and Inflammatory Mechanisms: Immune system dysfunction.
- Protein Aggregation: Accumulation of abnormal protein clumps.
- Viral Infections: Potential role of viral agents.
It is increasingly likely that specific genetic mutations and inherited predispositions can modify disease susceptibility and progression in ALS.
Who is Affected by ALS?
Demographically, ALS shows some trends in its prevalence. In the United States:
- Approximately 60% of reported ALS cases are men.
- 93% of patients are Caucasian.
Epidemiological studies in the US indicate that over 5,600 people are diagnosed with ALS annually, which translates to about 15 new cases each day. It’s estimated that around 30,000 Americans are living with ALS at any given time.
The typical age of onset for ALS is between 40 and 70 years, with an average age of diagnosis around 55. However, ALS can occur in younger individuals, with rare cases reported in people in their 20s and 30s.
The Diagnostic Journey for ALS
Diagnosing ALS is a complex process as there is no single definitive test. The diagnostic journey involves excluding other neurological conditions that present with similar symptoms. A comprehensive diagnostic evaluation typically includes:
- Electrodiagnostic Tests: Electromyography (EMG) and Nerve Conduction Velocity (NCV) studies to assess nerve and muscle function in bulbar (speech and swallowing), cervical (arms, diaphragm), thoracic (breathing muscles), and lumbar (legs) regions.
- Blood and Urine Studies: To rule out immunological or inflammatory diseases, including serum protein electrophoresis, thyroid and parathyroid hormone levels, and 24-hour urine heavy metal analysis.
- Spinal Tap (Lumbar Puncture): To analyze cerebrospinal fluid.
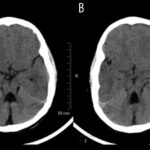
- Imaging Studies: X-rays, Magnetic Resonance Imaging (MRI), and CT scans, particularly of the cervical spine, to visualize the nervous system and rule out structural issues.
- Muscle and/or Nerve Biopsy: In some cases, to examine tissue samples.
- Thorough Neurological Examination: Clinical assessment by a neurologist.
The specific tests conducted are determined by the physician based on the individual’s physical examination and prior medical test results.
Current Treatment Approaches for ALS
Currently, there is no cure for ALS, nor are there treatments to reverse the damage already caused. However, significant progress has been made in developing treatments that can slow disease progression and manage symptoms.
Multidisciplinary Care and Medications for ALS
The cornerstone of ALS treatment involves a multidisciplinary approach, bringing together teams of specialists to support patients and families in navigating the challenges of living with ALS. This team typically includes neurologists, pulmonologists, physical therapists, occupational therapists, speech therapists, nutritionists, social workers, and palliative care specialists. This comprehensive care model has been shown to improve quality of life and even extend survival in people with ALS.
FDA-Approved Medications and Promising Clinical Trials
Two medications, riluzole (Rilutek, Teglutik) and edaravone (Radicava), are FDA-approved for ALS and have demonstrated a modest ability to slow disease progression. Furthermore, ongoing clinical trials worldwide are exploring novel therapeutic strategies to combat ALS, offering hope for future breakthroughs.
Assistive Devices and Therapies to Enhance Daily Living
A wide range of assistive devices and therapeutic interventions are available to help individuals with ALS maintain independence and quality of life for as long as possible:
-
Proper Body Positioning and Support
-
Exercise Regimens, Physical and Occupational Therapy
-
Walking Aids and Assistive Devices
-
Braces and Splints
-
Customized Wheelchairs
-
Home Modifications for Accessibility
-
Communication Technologies
-
Dietary Modifications and Nutritional Support
-
Feeding Tubes
-
Diaphragm Pacemakers
-
Ventilatory Support
Many individuals with ALS choose to participate in research studies and clinical trials to contribute to advancing the understanding and treatment of this disease. Resources like the US National Institutes of Health Clinical Trials Registry and the HSS ALS Program website provide information on ongoing research opportunities.
References
- Dean KE, Shen B, Askin G, Schweitzer AD, Shahbazi M, Wang Y, Lange D, Tsiouris AJ. A specific biomarker for amyotrophic lateral sclerosis: Quantitative susceptibility mapping. Clin Imaging. 2021 Jul;75:125-130. doi: 10.1016/j.clinimag.2020.12.018. Epub 2021 Jan 4. PMID: 33548870.
- Shtilbans A, Choi SG, Fowkes ME, Khitrov G, Shahbazi M, Ting J, Zhang W, Sun Y, Sealfon SC, Lange DJ. Differential gene expression in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011 Jul;12(4):250-6. doi: 10.3109/17482968.2011.560946. Epub 2011 Mar 4. PMID: 21375368.
- Schweitzer AD, Liu T, Gupta A, Zheng K, Seedial S, Shtilbans A, Shahbazi M, Lange D, Wang Y, Tsiouris AJ. Quantitative susceptibility mapping of the motor cortex in amyotrophic lateral sclerosis and primary lateral sclerosis. AJR Am J Roentgenol. 2015 May;204(5):1086-92. doi: 10.2214/AJR.14.13459. PMID: 25905946; PMCID: PMC4889122.
- Wainger BJ, Macklin EA, Vucic S, McIlduff CE, Paganoni S, Maragakis NJ, Bedlack R, Goyal NA, Rutkove SB, Lange DJ, Rivner MH, Goutman SA, Ladha SS, Mauricio EA, Baloh RH, Simmons Z, Pothier L, Kassis SB, La T, Hall M, Evora A, Klements D, Hurtado A, Pereira JD, Koh J, Celnik PA, Chaudhry V, Gable K, Juel VC, Phielipp N, Marei A, Rosenquist P, Meehan S, Oskarsson B, Lewis RA, Kaur D, Kiskinis E, Woolf CJ, Eggan K, Weiss MD, Berry JD, David WS, Davila-Perez P, Camprodon JA, Pascual-Leone A, Kiernan MC, Shefner JM, Atassi N, Cudkowicz ME. Effect of Ezogabine on Cortical and Spinal Motor Neuron Excitability in Amyotrophic Lateral Sclerosis: A Randomized Clinical Trial. JAMA Neurol. 2021 Feb 1.