Staphylococcus aureus (S. aureus) is a bacterium commonly found on human skin and mucous membranes. While often harmless, it can cause infections if the skin or mucosal barrier is breached. Methicillin-resistant Staphylococcus aureus (MRSA) is a strain resistant to methicillin and other common antibiotics, posing a significant challenge in healthcare settings. This article provides a detailed guide on Mrsa Diagnosis, screening, and management, crucial for healthcare professionals aiming to optimize patient care and control the spread of this infection. Understanding the nuances of mrsa diagnosis is the first step in effective intervention.
It is essential to distinguish between MRSA colonisation and infection. Colonisation occurs when MRSA is present on the body without causing illness, residing on the skin or in the nose. Infection, however, happens when MRSA invades tissues and causes disease. Accurate mrsa diagnosis is critical to differentiate between these states and guide appropriate clinical responses.
The rise of MRSA is a global health concern. Recent reports indicate an increase in MRSA cases, highlighting the urgent need for effective diagnostic and preventative strategies. Healthcare professionals, especially pharmacists and pharmacy technicians, play a vital role in curbing MRSA transmission through antimicrobial stewardship and robust infection prevention and control measures. Effective mrsa diagnosis protocols are at the heart of these efforts.
The Growing Concern of MRSA: Epidemiology and Recent Trends
In the 1990s, MRSA was responsible for a significant proportion of S. aureus bloodstream infections. While interventions like national guidelines focusing on screening, isolation, and hand hygiene were introduced, MRSA prevalence remained a challenge. The UK, for instance, once had one of the highest MRSA rates in Europe. Mandatory surveillance and root cause analysis (RCA) for MRSA bacteraemia cases were implemented to combat this.
These measures have contributed to a reduction in MRSA bacteraemia incidence over time, as shown in Figure 1. However, recent data suggest a potential resurgence. A 2024 report indicated a 16.6% increase in MRSA cases compared to the previous year, coinciding with a rise in hospital-onset cases. Comparing current figures to pre-pandemic levels reveals a concerning trend of MRSA rates returning to, or even exceeding, previous levels. This resurgence underscores the ongoing importance of vigilant mrsa diagnosis and control strategies.
Pharmacists are crucial in supporting RCAs by evaluating antimicrobial prescribing and advising on decolonisation therapies. Learning from these reviews is disseminated to clinical teams to improve practice and prevent recurrence. Audits of antimicrobial prescribing are also conducted to ensure best practices are followed. This proactive approach, coupled with accurate mrsa diagnosis, is essential in managing MRSA effectively.
Infection Prevention and Control: Cornerstones of MRSA Management
MRSA is now endemic in many healthcare settings, particularly in high-risk areas like intensive care units, burn units, and orthopaedic wards. Patients with medical devices, trauma, or surgical wounds are at increased risk of MRSA colonisation or infection. The primary mode of transmission in healthcare is via healthcare workers’ hands, highlighting the critical importance of hand hygiene. Rarer transmission routes include contact with contaminated surfaces or objects.
Effective hand hygiene is the cornerstone of infection prevention and control (IPC). This includes hand washing with soap and water or using alcohol-based sanitizers. Covering cuts and abrasions is also crucial. Healthcare professionals must adhere to the five moments of hand hygiene (Figure 2) and promote compliance among colleagues. These moments are key points where hand hygiene is most effective in preventing transmission, thus impacting mrsa diagnosis and spread indirectly by reducing overall infection risk.
Other IPC measures include barrier nursing with gloves and aprons, and patient isolation in single rooms when feasible. These strategies, combined with rigorous hand hygiene and prompt mrsa diagnosis, are fundamental in controlling MRSA in healthcare environments.
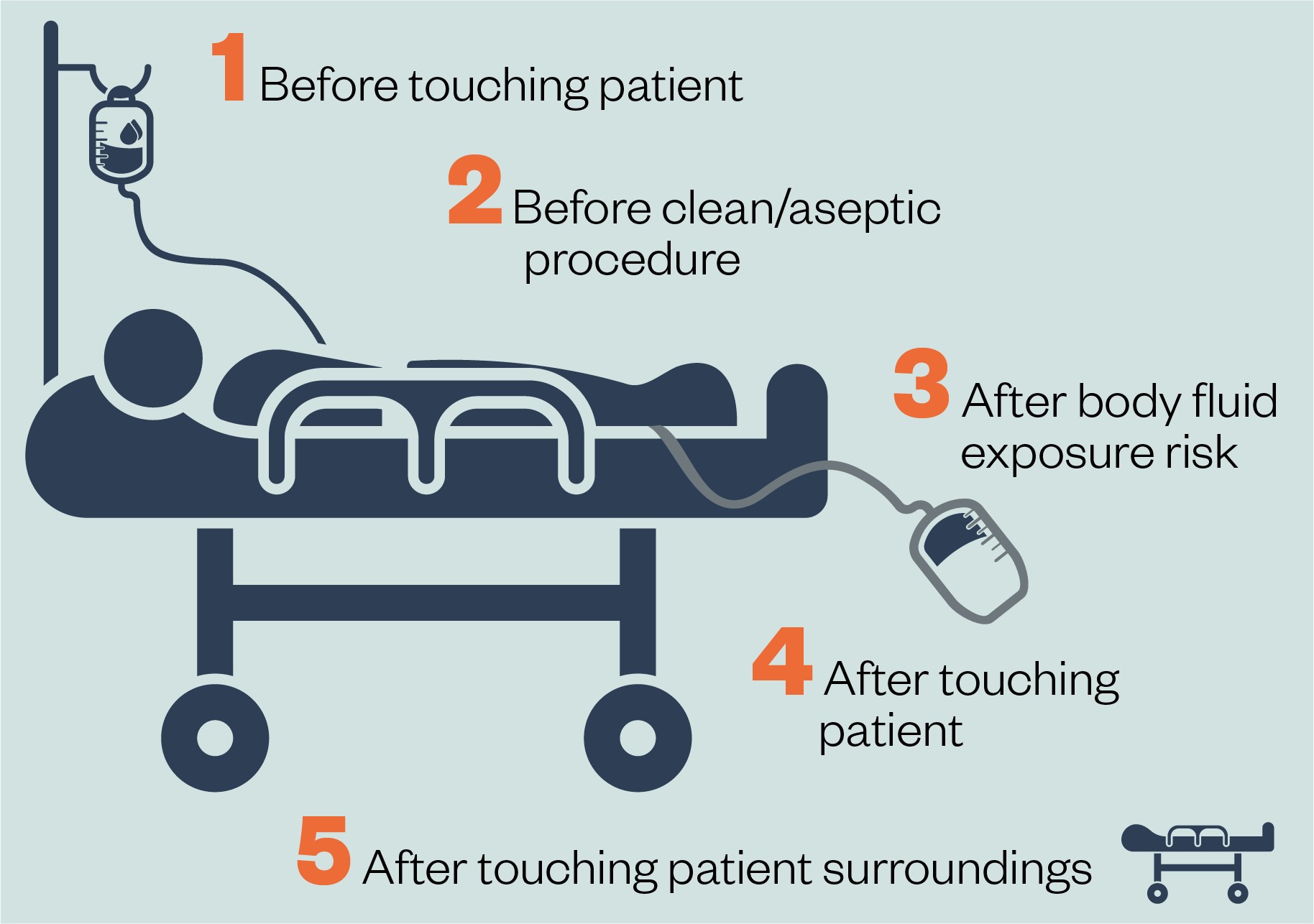 Five moments for hand hygieneFigure 2: Five moments for hand hygiene. Reproduced from the World Health Organization’s guidelines on hand hygiene in healthcare.
Five moments for hand hygieneFigure 2: Five moments for hand hygiene. Reproduced from the World Health Organization’s guidelines on hand hygiene in healthcare.
Detection of MRSA: Diagnosing Colonisation and Infection
Mrsa diagnosis relies on microbiological methods to detect the presence of the bacteria, whether as colonisation or active infection. Screening and diagnostic testing are distinct processes, each serving different clinical purposes.
Diagnosing MRSA Colonisation
MRSA colonisation is identified through microbiological screening. Guidelines recommend screening for specific patient groups (Box 1), with local policies potentially including additional high-risk groups. Nasal screening is commonly used as the anterior nares are frequently colonised. However, screening of damaged skin areas may also be necessary. The extent of screening sites (e.g., groin, axilla, perineum) is guided by local and national guidelines.
Box 1: Recommendations for MRSA Screening
Secondary care:
- All patients admitted to high-risk specialties*;
- Patients with a history of MRSA colonisation or infection.
Primary care:
- Patients presenting with suspected MRSA infection.
* High-risk specialties include vascular, renal/dialysis, neurosurgery, cardiothoracic surgery, haematology/oncology/bone marrow transplant, orthopaedics/trauma, intensive care units, high dependency units, and coronary care units.
Microbiological mrsa diagnosis screening involves selective culture methods to identify methicillin-resistant strains. This typically includes direct or enrichment culture, often using chromogenic selective MRSA medium. Molecular methods can also be employed. The identification stage confirms S. aureus species and resistance to cefoxitin.
Healthcare organisations often have alert systems to identify patients with a history of MRSA. Familiarity with these systems is crucial when reviewing patients’ therapies to ensure appropriate decolonisation is considered when indicated. This historical data is valuable in informing current mrsa diagnosis and management strategies.
Diagnosing MRSA Infection
Mrsa diagnosis of infection requires clinical samples taken from the patient and sent for laboratory analysis. The sample type depends on the suspected infection site, ranging from blood cultures for suspected sepsis to wound swabs or sputum samples.
S. aureus can be cultured from various samples, including blood, pus, sputum, urine, and joint fluid. Once cultured and identified as S. aureus, antimicrobial susceptibility testing is performed to determine methicillin resistance, thus confirming mrsa diagnosis.
Clinically, MRSA infection is indistinguishable from methicillin-susceptible S. aureus (MSSA) infection. However, MRSA infections are more strongly associated with hospital-acquired infections and tend to have higher fatality rates in bacteraemia cases. Risk factors for MRSA infection include recent hospitalisation, invasive devices, prior MRSA history, long-term care residence, antibiotic use, intravenous drug use, lack of response to first-line antibiotics, and recurrent skin or soft tissue infections, particularly if purulent. Recognizing these risk factors aids in prompt mrsa diagnosis and initiation of appropriate treatment.
Actionable Steps Following Suspected MRSA Infection
When MRSA infection is suspected, prompt action is crucial. Empirical antibiotics may be started based on local guidelines, tailored to the suspected infection syndrome and patient severity. Ideally, clinical samples for mrsa diagnosis should be collected before starting antibiotics to optimize culture yield.
In patients known to be MRSA-colonised or at high risk, clinicians may choose antibiotics with MRSA coverage empirically, pending culture results. Once laboratory confirmation of MRSA is obtained, targeted treatment regimens effective against MRSA should be implemented. Rapid and accurate mrsa diagnosis is therefore essential for timely and effective treatment.
Nasal and Skin Decolonisation Strategies
MRSA decolonisation is not routinely recommended for asymptomatic community carriers. However, for colonised patients undergoing high-risk surgery (Box 1), decolonisation is advised to reduce surgical site infection risk and prevent transmission.
Complete MRSA eradication may not always be achievable, but reducing bacterial load minimizes endogenous infection risk and transmission. Local policies guide post-decolonisation screening and repeat decolonisation. Effective decolonisation strategies are an adjunct to accurate mrsa diagnosis and IPC measures.
Decolonisation protocols vary based on local guidance, considering procedure type, patient risk factors (including allergies), and potential for transmission. Factors like allergies to product ingredients (e.g., arachis oil), risk of chemical injuries in preterm babies with chlorhexidine, infection impact, local formularies, and resistance patterns are considered.
Nasal Decolonisation Methods
NICE guidelines recommend nasal mupirocin ointment combined with chlorhexidine body wash before procedures with potential S. aureus surgical site infections. Neomycin/chlorhexidine nasal cream is an alternative for mupirocin-resistant MRSA or allergies. (Box 2 provides dosing information). Patient counselling on nasal ointment/cream administration is essential for adherence and effectiveness.
Box 2: Dosing for Nasal Decolonisation Products
Mupirocin nasal ointment:
- Apply to both nostrils three times daily for five days.
Neomycin/chlorhexidine nasal cream:
- Apply to both nostrils four times daily for ten days.
- Contains arachis oil (peanut oil) – avoid in peanut/soy allergies.
These are general guidelines, and local policies may vary.
Skin Decolonisation Regimens
Skin cleansers, typically chlorhexidine 4% skin cleanser, are used with nasal ointments for MRSA skin decolonisation. Product-specific instructions, including contact time, should be followed. Cleansers should not be used on broken skin. Side effects, like irritation or chemical burns (especially in preterm babies with chlorhexidine 4%), need consideration. Allergy considerations, such as soya oil in some chlorhexidine formulations, are also important.
Skin reactions are the most common side effect of nasal and skin decolonisation products. Patients should be advised on product use, hygiene practices (clean cloths, clothing, bedding), and what to do if adverse reactions occur. Effective decolonisation, guided by accurate mrsa diagnosis, is a multi-faceted approach.
Surgical Prophylaxis for MRSA-Colonised Patients
NICE guidelines recommend antibiotic prophylaxis for surgeries not classified as ‘clean non-prosthetic uncomplicated surgery’. For MRSA-colonised patients, prophylactic antibiotics must cover MRSA in addition to standard gram-positive and gram-negative coverage.
Local antibiotic guidelines should provide alternative regimens for MRSA-colonised patients. Intravenous teicoplanin is commonly used. Clearly stating the indication as surgical prophylaxis, including MRSA cover for colonisation, is crucial to avoid incorrect assumptions of a treatment course and prevent antibiotic overuse. This targeted prophylaxis, informed by mrsa diagnosis, is a key aspect of antimicrobial stewardship.
Treatment Strategies for MRSA Infection
Vancomycin and teicoplanin, both parenteral glycopeptide antibiotics, remain first-line treatments for MRSA infection. Vancomycin has a narrow therapeutic range requiring therapeutic drug monitoring (TDM) to optimize efficacy and minimize toxicity (nephrotoxicity, ototoxicity). Target trough levels vary by infection type (e.g., 15–20mg/L for deep-seated infections). Teicoplanin has a wider therapeutic range, and TDM use varies.
Pharmacists are essential in undertaking TDM to optimize patient therapy. Local guidelines should inform dosing and target levels for vancomycin and teicoplanin. Other antibiotics for MRSA management, based on sensitivity patterns, include linezolid, co-trimoxazole, daptomycin, clindamycin, rifampicin, ciprofloxacin, and delafloxacin. Fluoroquinolones, like ciprofloxacin, should be reserved for cases where other antibiotics are unsuitable due to safety concerns. Adherence to prescribed treatment is vital, and patient involvement in decision-making is crucial. Effective treatment, following accurate mrsa diagnosis, is paramount to patient outcomes.
Antimicrobial Stewardship and MRSA: A Collaborative Approach
Antimicrobial resistance (AMR) is a major global health threat, with MRSA being a significant contributor. Antimicrobial stewardship is crucial to preserve antibiotic effectiveness and reduce infection transmission. This involves appropriate antibiotic selection, optimal dosing and duration, and minimizing toxicity.
Pharmacists and pharmacy technicians are vital in reviewing antimicrobial prescriptions and promoting stewardship. Box 3 outlines their role in MRSA management within antimicrobial stewardship. This includes ensuring appropriate decolonisation and treatment, optimizing antibiotic use, supporting dose optimisation through TDM, and counselling patients on adherence and medication disposal. Effective mrsa diagnosis informs targeted antimicrobial stewardship interventions.
Box 3: Pharmacist/Technician Roles in Antimicrobial Stewardship for MRSA
- Adhere to IPC when reviewing MRSA patients.
- Prevent unnecessary decolonisation/treatment in asymptomatic colonisation.
- Support appropriate selection of:
- MRSA decolonisation therapy.
- Surgical prophylaxis antibiotics for MRSA-colonised patients.
- Antibiotics for MRSA infection.
- Ensure appropriate duration of decolonisation products.
- Regularly review antibiotic necessity in MRSA bacteraemia.
- Support dose optimisation (renal function, TDM).
- Counsel patients on decolonisation/antibiotics for compliance and disposal.
Conclusion: Enhancing MRSA Management Through Accurate Diagnosis
MRSA poses a significant challenge in healthcare due to its transmissibility, impact on patient outcomes, and healthcare costs. Healthcare professionals must understand mrsa diagnosis, screening, and management, alongside IPC guidelines, to effectively combat this pathogen. Pharmacy professionals play a crucial role in identifying patients needing decolonisation or antibiotic review through familiarity with local MRSA policies and alert systems. Continuous education and adherence to best practices in mrsa diagnosis and management are essential to mitigating the impact of MRSA.
This article has been reviewed and updated to ensure its continued relevance and accuracy in guiding healthcare professionals in the effective management of MRSA.
References