A lumbar puncture, also known as a spinal tap, is a crucial diagnostic procedure used in the evaluation of multiple sclerosis (MS). This test involves extracting and examining a sample of cerebrospinal fluid (CSF), the protective liquid that surrounds the brain and spinal cord. For individuals undergoing investigation for MS, understanding the role and process of a lumbar puncture is essential.
What is a Lumbar Puncture and How is it Performed?
A lumbar puncture is typically conducted as an outpatient procedure and takes around 30 minutes to complete, utilizing local anaesthesia to minimize discomfort. The patient is usually positioned lying on their side or sitting up, allowing the clinician to access the lumbar region. This area, located in the lower back between the lowest ribs and the pelvis, provides a safe entry point.
During the procedure, a thin, flexible needle is carefully inserted between the vertebrae in the lumbar spine and into the space containing the cerebrospinal fluid. Once correctly positioned, a small amount of CSF is withdrawn for laboratory analysis. Patients may experience pressure or mild discomfort during the needle insertion, but significant pain is uncommon due to the local anaesthetic.
 Close-up of electrophoresis gel showing oligoclonal bands
Close-up of electrophoresis gel showing oligoclonal bands
Why is a Lumbar Puncture Necessary for MS Diagnosis?
The analysis of cerebrospinal fluid obtained through a lumbar puncture plays a vital role in supporting a diagnosis of multiple sclerosis. CSF analysis can reveal several key indicators that are often associated with MS, helping to differentiate it from other neurological conditions. The primary components examined in CSF for MS diagnosis include:
White Blood Cell Count
An elevated number of white blood cells in the CSF is a common finding in individuals with MS. Typically, in MS patients, the white blood cell count in CSF can be up to seven times higher than normal levels. However, a significantly higher count might suggest an infection, such as Lyme disease, rather than MS, highlighting the importance of considering other clinical factors and test results.
Neurofilaments
Neurofilaments are structural proteins found within nerve axons. The presence of neurofilaments in the CSF indicates nerve damage and myelin breakdown, which are hallmarks of MS. Detecting neurofilaments in CSF can provide evidence of ongoing myelin attack. Furthermore, monitoring neurofilament levels through repeat lumbar punctures can be useful in assessing the effectiveness of disease-modifying therapies. A decrease in neurofilament levels may suggest that the treatment is successfully protecting the nerves.
Oligoclonal Bands
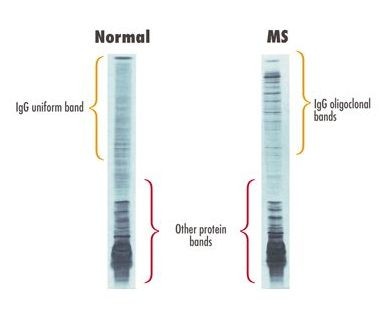
Oligoclonal bands are abnormal bands of antibodies found in the CSF. In MS, the immune system mistakenly targets myelin, leading to an increased production of antibodies that cross the blood-brain barrier and attack the myelin sheath. Consequently, individuals with MS often exhibit higher levels of antibodies in their CSF compared to their blood. Therefore, a blood sample is usually taken concurrently for comparison.
The electrophoresis test is used to detect oligoclonal bands. This technique involves placing a CSF sample on a gel and applying an electric voltage. Antibodies of similar size migrate together, forming visible bands. While a single band (monoclonal) is considered normal, the presence of two or more bands, termed oligoclonal bands, suggests immune system activity within the central nervous system. Oligoclonal bands are found in 80-95% of people with MS, making their presence a strong indicator, although not exclusively diagnostic of MS.
Managing Potential Side Effects: Post Lumbar Puncture Headache
One of the more common side effects following a lumbar puncture is a headache, often described as a severe, splitting headache. This post lumbar puncture headache is thought to be caused by a reduction in CSF pressure due to the fluid removal. While typically resolving within 24 hours, these headaches can persist longer in some individuals.
To minimize the risk of headache, it is generally recommended to lie flat for at least six hours after the procedure and to stay well-hydrated by drinking plenty of water. The type of needle used can also influence the likelihood of headaches. Atraumatic needles, such as Sprotte needles, are designed to reduce the incidence of post-lumbar puncture headaches. Although not universally used, these needles are recommended by medical guidelines, and patients concerned about headaches can inquire about their availability.
Conclusion
In conclusion, a lumbar puncture is a valuable diagnostic tool in the process of diagnosing multiple sclerosis. By analyzing the cerebrospinal fluid for white blood cells, neurofilaments, and oligoclonal bands, clinicians can gain important insights into the disease process. Understanding the procedure and its role in MS diagnosis empowers patients and facilitates informed discussions with their healthcare providers. While potential side effects like headaches exist, strategies and advanced needle types are available to mitigate these risks, making the lumbar puncture a relatively safe and informative procedure for MS evaluation.
References
Link H, Huang YM. Oligoclonal bands in multiple sclerosis cerebrospinal fluid: an update on methodology and clinical usefulness. Journal of Neuroimmunology 2006;180(1-2):17-28. Summary (link is external)
Lechner-Scott J, et al. The frequency of CSF oligoclonal banding in multiple sclerosis increases with latitude. Multiple Sclerosis Journal 2012;18(7):974–982. Summary (link is external)
Davis A, et al Change practice now! Using atraumatic needles to prevent post lumbar puncture headache European Journal of Neurology 2014 21(2) 305-311 Summary (link is external)