Crafting an effective nursing care plan is a cornerstone of modern healthcare, demanding a structured, step-by-step methodology to ensure all facets are meticulously addressed. This guide offers an in-depth exploration into developing nursing care plans, emphasizing the crucial role of NANDA nursing diagnoses in this process. Whether you are a nursing student or a seasoned professional, this resource will enhance your understanding and application of care plans, providing a robust database and examples for practical use. Dive into the essential components, objectives, and purposes of nursing care plans, and discover how to create plans that are not only excellent but also profoundly patient-centered.
Understanding Nursing Care Plans
A nursing care plan (NCP) is a formal, dynamic blueprint for patient care. It meticulously identifies a patient’s current health needs, potential risks, and outlines strategies to achieve desired health outcomes. Care plans are vital tools for communication among nurses, patients, and the broader healthcare team, ensuring a cohesive and coordinated approach to treatment. Without a well-defined care planning process, the consistency and quality of patient care would be significantly compromised.
The nursing care planning journey begins the moment a patient is admitted and continues to evolve. It’s a living document, continuously updated to reflect changes in the patient’s condition and the ongoing evaluation of their progress towards set goals. At its heart, effective nursing practice is rooted in the principle of planning and delivering individualized, patient-centric care, and the care plan is the primary tool to achieve this.
Exploring Types of Nursing Care Plans
Nursing care plans exist on a spectrum from informal to formal. An informal nursing care plan is essentially a mental strategy, a nurse’s internal roadmap for care. In contrast, a formal nursing care plan is a documented, structured guide, either written or digital, that organizes all essential patient care information.
Formal care plans further branch into standardized and individualized types. Standardized care plans are designed for groups of patients with common needs, providing a consistent baseline of care. Individualized care plans, on the other hand, are meticulously tailored to meet the specific and unique needs of each patient, going beyond the scope of standardized plans.
Delving into Standardized Care Plans
Standardized care plans serve as pre-approved guidelines, developed by nursing staff and healthcare institutions to guarantee consistent care for patients with similar conditions. They ensure that a minimum standard of care is met efficiently, streamlining nurses’ workflow by eliminating the need to repeatedly create plans for common patient needs within a unit.
It’s crucial to recognize that standardized care plans are not designed to address the nuanced needs of individual patients fully. However, they are invaluable as a starting point, a foundation upon which to build a more personalized approach through an individualized care plan.
The care plans presented in this guide are primarily standardized, intended to serve as a framework or direction for developing individualized care plans tailored to specific patient needs.
The Power of Individualized Care Plans
An individualized care plan takes a standardized plan and customizes it to align perfectly with a specific patient’s unique requirements and goals. This involves incorporating approaches known to be particularly effective for that individual. This personalized strategy allows for more holistic care, addressing the patient’s needs in a way that respects their individuality, strengths, and personal objectives.
Furthermore, individualized care plans have been shown to significantly enhance patient satisfaction. When patients perceive that their care is specifically designed for them, they feel more valued and understood, leading to greater contentment with their healthcare experience. In today’s healthcare environment, where patient satisfaction is increasingly recognized as a key indicator of quality, the importance of individualized care plans cannot be overstated.
Tips for Individualizing a Nursing Care Plan:
- Detailed Assessment: Begin with a comprehensive assessment to identify the patient’s unique needs, preferences, and goals.
- NANDA Diagnoses: Utilize NANDA-I nursing diagnoses to accurately reflect the patient’s health status and needs. This standardized language ensures clarity and precision in identifying patient problems.
- Patient Involvement: Actively involve the patient and their family in the care planning process. Their input is crucial for creating a plan that is truly patient-centered.
- Realistic Goals: Set SMART goals (Specific, Measurable, Achievable, Realistic, Time-bound) that are relevant to the individual patient’s circumstances.
- Tailored Interventions: Select nursing interventions that are specifically suited to the patient’s needs and preferences, drawing from evidence-based practices and considering the patient’s context.
- Flexibility: Ensure the care plan is flexible and can be adjusted as the patient’s condition changes or as new needs emerge.
- Cultural Sensitivity: Incorporate cultural considerations into the care plan, respecting the patient’s beliefs and values.
- Resource Awareness: Consider available resources and tailor the plan to be realistic within the given healthcare setting and patient’s home environment.
Objectives of Nursing Care Plans
The primary objectives of developing nursing care plans are multifaceted, all aimed at enhancing the quality and effectiveness of patient care:
- Promoting Evidence-Based Care: To ground nursing interventions in the best available evidence, ensuring patients receive the most effective and up-to-date treatments within a comforting and familiar healthcare setting.
- Supporting Holistic Care: To address the patient as a whole person, considering their physical, psychological, social, and spiritual dimensions in the management and prevention of disease. This aligns with the principles of holistic care, recognizing the interconnectedness of these aspects of health.
- Establishing Care Programs: To create structured approaches to care, such as care pathways and care bundles. Care pathways foster team consensus on standards of care and expected outcomes, while care bundles focus on best practices for specific conditions.
- Defining Goals and Outcomes: To clearly identify and differentiate between broad goals and specific, measurable expected outcomes for patient care.
- Enhancing Communication and Documentation: To improve communication among healthcare providers and to ensure thorough and accurate documentation of the care plan, facilitating continuity and coordination of care.
- Measuring Nursing Care Effectiveness: To provide a framework for evaluating the impact of nursing interventions and the overall quality of care provided.
Purposes and Importance of Nursing Care Plans
Nursing care plans serve several critical purposes, highlighting their indispensable role in patient care:
- Defining the Nurse’s Role: Care plans delineate the unique and independent contributions of nurses to patient well-being, emphasizing their role beyond simply following physician’s orders. They underscore the nurse’s autonomy in addressing patients’ holistic health needs.
- Guiding Individualized Patient Care: The care plan acts as a detailed roadmap for patient care, encouraging nurses to think critically and develop interventions specifically tailored to each individual’s unique needs and circumstances.
- Ensuring Continuity of Care: By providing a clear, documented plan, care plans enable nurses across different shifts and departments to deliver consistent, high-quality interventions, maximizing the benefits of treatment for patients through seamless care transitions.
- Coordinating Care Among Disciplines: Care plans ensure that all members of the healthcare team are informed about the patient’s needs and the planned actions, preventing fragmentation of care and promoting a unified approach.
- Facilitating Documentation and Accountability: Care plans serve as essential documentation, outlining necessary observations, nursing actions, and patient/family education. Accurate documentation in the care plan provides evidence that care was delivered and meets professional standards.
- Guiding Staff Assignments: In situations where patients require specialized skills, care plans can inform staff assignments, ensuring patients are matched with nurses possessing the necessary expertise for their specific needs.
- Monitoring Patient Progress: Care plans provide a benchmark for tracking a patient’s progress and making necessary adjustments to the care strategy as their health status and goals evolve over time.
- Supporting Reimbursement Processes: Insurance providers often rely on medical records, including care plans, to determine appropriate reimbursement for healthcare services, highlighting the care plan’s role in the financial aspects of healthcare delivery.
- Clarifying Patient Goals and Promoting Engagement: Care plans benefit both nurses and patients by fostering patient involvement in their treatment and care decisions, promoting a collaborative and patient-centered approach.
Key Components of a Nursing Care Plan
A comprehensive nursing care plan (NCP) typically includes several essential components, each contributing to its effectiveness and clarity. These usually encompass:
- Nursing Diagnoses: Based on NANDA-I, these are clinical judgments about individual, family, or community experiences/responses to actual or potential health problems and/or life processes. They provide the foundation for the care plan.
- Patient Problems/Needs: A clear statement of the health issues or needs identified through patient assessment and NANDA diagnosis.
- Expected Outcomes: Measurable, patient-centered goals that define the desired changes in the patient’s health status as a result of nursing care.
- Nursing Interventions: Specific actions that nurses will implement to achieve the expected outcomes. These interventions should be evidence-based and tailored to the patient’s needs.
- Rationales: Scientific principles or evidence that justify the selected nursing interventions, explaining why each intervention is expected to be effective.
- Evaluation: A method for assessing the patient’s progress toward achieving the expected outcomes and the effectiveness of the nursing care plan.
These components are meticulously organized to provide a structured and logical approach to patient care planning.
Formats for Nursing Care Plans
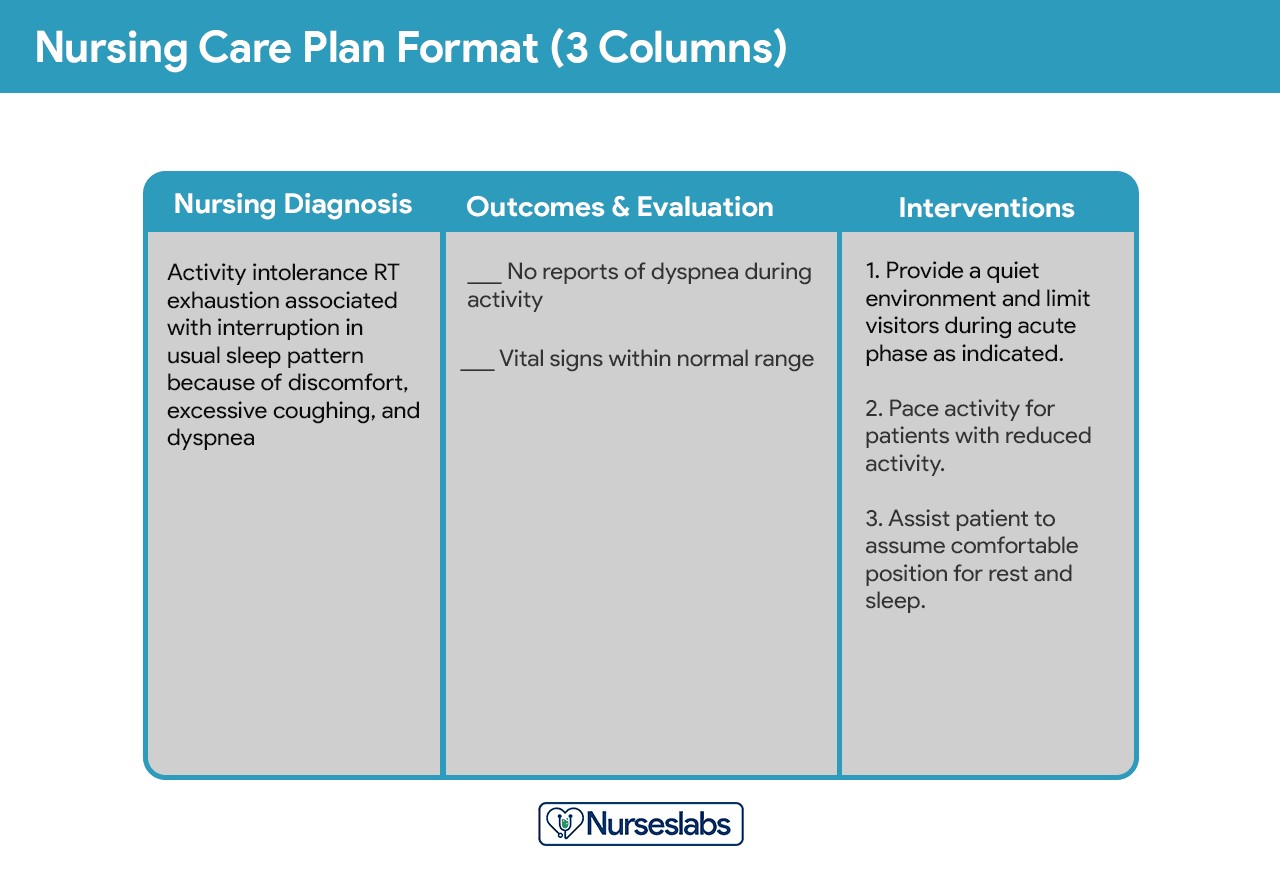
Nursing care plans can be structured in various formats, often categorized by the number of columns used to organize the information. Common formats include three-column, four-column, and sometimes five-column plans.
Three-Column Format
The three-column format is a streamlined approach, typically including columns for:
- Nursing Diagnosis (NANDA): Clearly stated using standardized NANDA-I terminology.
- Outcomes and Evaluation: Combining desired patient outcomes and the criteria for evaluating their achievement in one column.
- Nursing Interventions: Listing the specific nursing actions planned to address the diagnosis and achieve the outcomes.
This format is concise and focuses on the essential elements of the care plan.
Three-column nursing care plan format
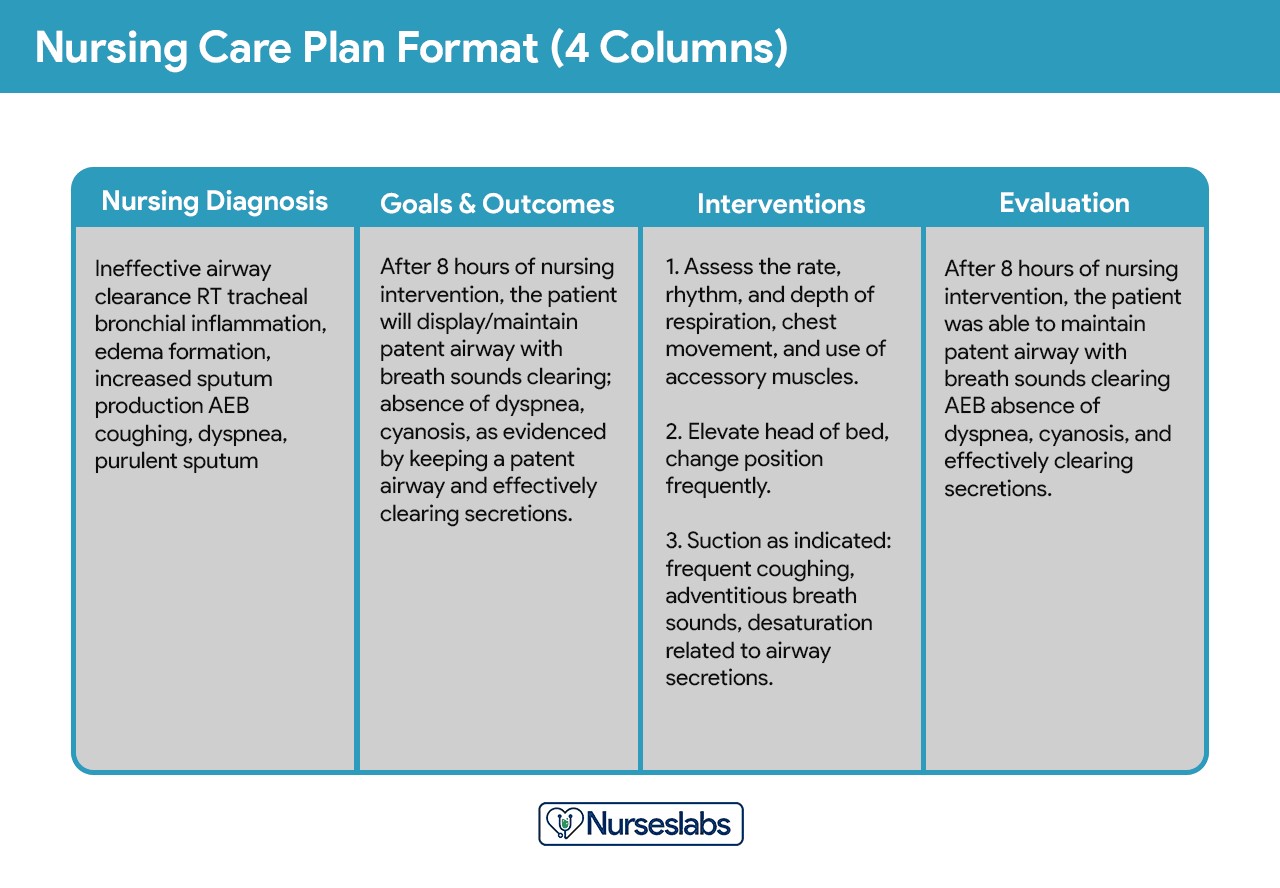
Four-Column Format
The four-column format provides a more detailed structure, separating outcomes and evaluation into distinct columns:
- Nursing Diagnosis (NANDA): As with the three-column format, this uses NANDA-I diagnoses.
- Goals and Outcomes: Clearly defined, measurable goals and expected outcomes for the patient.
- Nursing Interventions: Detailed interventions designed to meet the goals and outcomes.
- Evaluation: A separate column to document the evaluation of patient progress and the effectiveness of interventions.
This format allows for a more explicit separation of the planning and evaluation phases.
Four-column nursing care plan template
Below, you’ll find sample templates for different nursing care plan formats, which you can adapt and use as needed.
Download: Printable Nursing Care Plan Templates and Formats
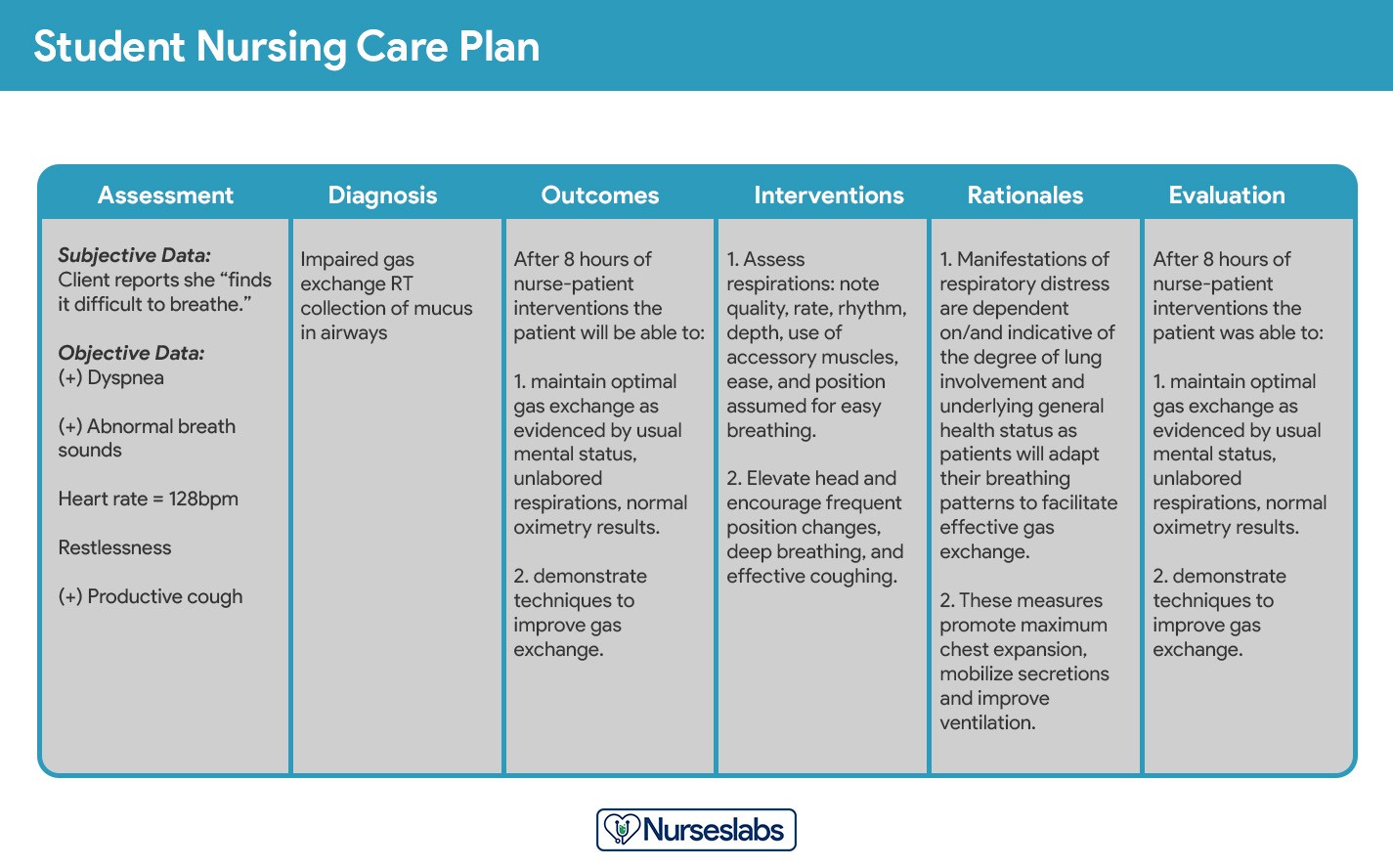
Student Care Plans: A Detailed Approach
Student care plans are typically more comprehensive than those used by practicing nurses. This is because they serve as a vital learning tool for nursing students, helping them to deeply understand the care planning process.
Student nursing care plans are more detailed.
Often, student care plans are handwritten and include an additional column for “Rationale” or “Scientific Explanation.” This rationale column is placed after the nursing interventions, requiring students to articulate the scientific basis for each chosen intervention, further solidifying their understanding of the principles behind nursing care.
Step-by-Step Guide to Writing a Nursing Care Plan
Creating a nursing care plan effectively involves a systematic approach. Here are the steps to guide you through the process:
Step 1: Patient Data Collection and Assessment
The initial step is to gather comprehensive patient data. This involves utilizing various assessment techniques and data collection methods, such as:
- Physical Assessment: Conducting a thorough physical assessment to evaluate the patient’s current health status.
- Health History: Obtaining a detailed health history, including past medical conditions, surgeries, allergies, and current medications.
- Patient Interview: Engaging in an interview with the patient to understand their symptoms, concerns, and perspectives on their health.
- Medical Records Review: Examining the patient’s medical records, including physician’s notes, diagnostic test results, and previous care plans.
- Diagnostic Studies: Reviewing results from relevant diagnostic tests and procedures.
This comprehensive client database forms the foundation of the care plan. During this phase, nurses identify related or risk factors and defining characteristics that will be used to formulate NANDA nursing diagnoses. Some institutions or nursing programs may provide specific assessment formats to guide this process.
Critical thinking is paramount during patient assessment. It requires integrating knowledge from various scientific disciplines and professional guidelines to make informed evaluations. This process is crucial for complex clinical decision-making, aiming to accurately identify patients’ healthcare needs within a supportive environment and using reliable information.
Step 2: Analyzing and Organizing Patient Data
Once patient data is collected, the next step is to analyze, cluster, and organize this information. This involves:
- Data Analysis: Interpreting the collected data to identify patterns, trends, and significant findings related to the patient’s health.
- Data Clustering: Grouping related data points together to identify potential health problems and needs. For example, clustering symptoms like shortness of breath, fatigue, and chest pain might indicate a respiratory or cardiac issue.
- Prioritization: Determining the most critical health problems that require immediate attention based on the analyzed data.
- Formulating Nursing Diagnoses: Using the clustered data to develop NANDA nursing diagnoses that accurately represent the patient’s health status and needs.
- Setting Desired Outcomes: Based on the diagnoses, identifying what the nurse and patient hope to achieve in terms of health improvement.
This step transforms raw data into actionable insights, setting the stage for effective care planning.
Step 3: Formulating NANDA Nursing Diagnoses
Nursing diagnoses, particularly those based on NANDA-I, provide a standardized and precise way to identify and address specific patient needs and responses to health issues. They are clinical judgments about actual or potential health problems that nurses are qualified and licensed to treat independently.
NANDA International (NANDA-I) is the leading organization in developing and standardizing nursing diagnoses. Using NANDA-I diagnoses ensures:
- Standardized Language: A common language for nurses to communicate about patient problems across different settings and regions.
- Evidence-Based Practice: Diagnoses are regularly reviewed and updated based on current research and clinical practice.
- Clarity and Precision: NANDA-I diagnoses are specific and clearly defined, reducing ambiguity in care planning.
- Improved Documentation: Standardized diagnoses facilitate clear and concise documentation of patient needs and nursing care.
- Enhanced Professionalism: Using a recognized diagnostic framework enhances the professional standing of nursing practice.
For a detailed guide on formulating nursing diagnoses, refer to resources specifically focused on NANDA and nursing diagnosis methodology.
Step 4: Setting Priorities for Nursing Diagnoses
Prioritizing nursing diagnoses involves establishing a hierarchy for addressing patient problems and planning interventions. This step ensures that the most critical needs are addressed first. Prioritization is guided by:
- Life-Threatening Issues: Problems that pose an immediate threat to the patient’s life (e.g., airway obstruction, severe bleeding) are always the highest priority.
- Maslow’s Hierarchy of Needs: Applying Maslow’s Hierarchy of Needs helps prioritize basic physiological needs (e.g., breathing, circulation) before higher-level needs (e.g., safety, love, self-esteem).
- Patient Preferences: Considering the patient’s own priorities and concerns is crucial for patient-centered care.
- Urgency: Determining which problems require immediate intervention versus those that can be addressed later.
Diagnoses are often categorized as high, medium, or low priority. High-priority diagnoses are those that are life-threatening or have the greatest potential to cause harm.
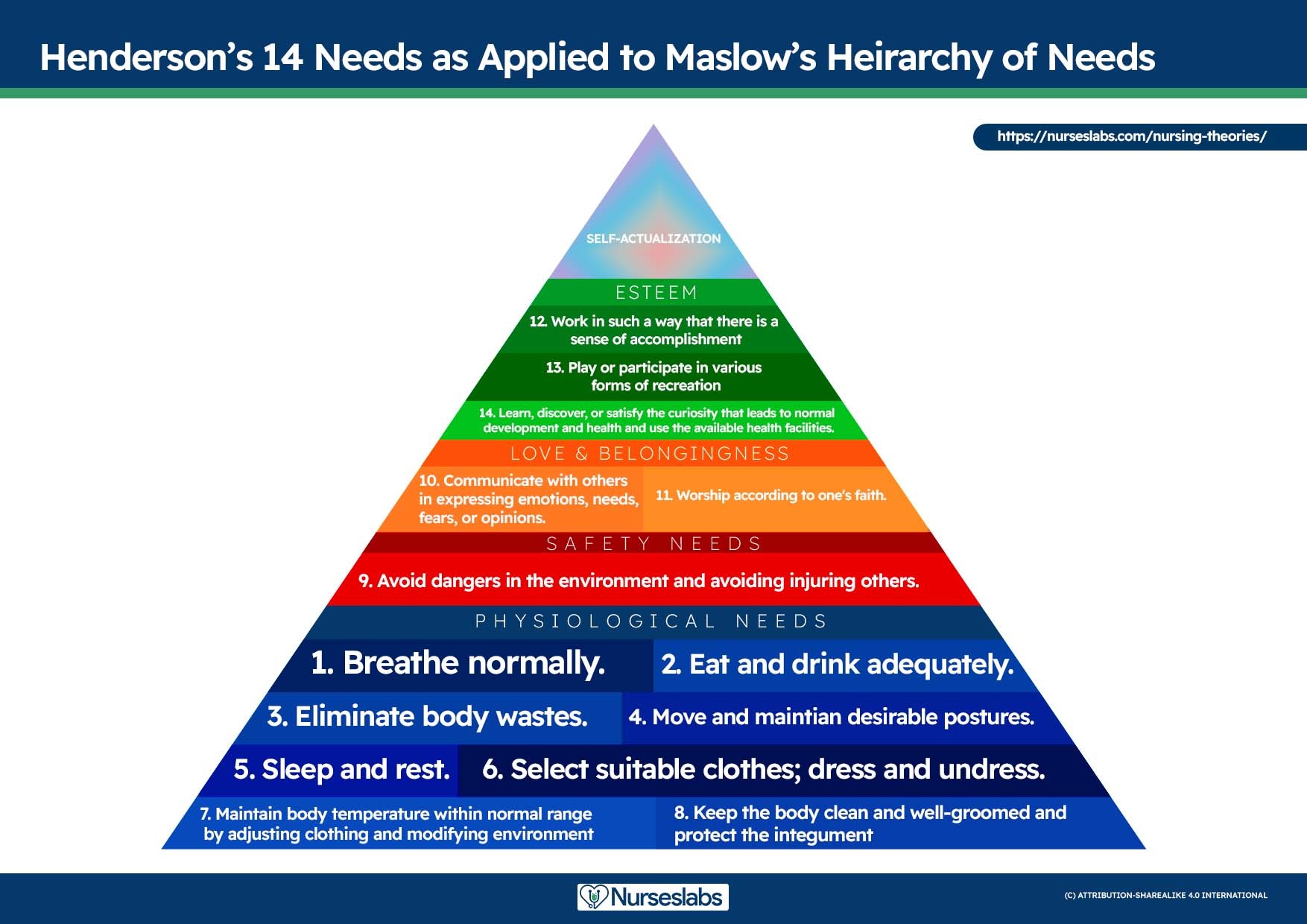
Maslow’s Hierarchy of Needs in Nursing Prioritization:
Maslow’s Hierarchy of Needs provides a valuable framework for prioritizing nursing care. Developed by Abraham Maslow, this theory posits that human needs are hierarchical, with basic physiological needs at the base and self-actualization at the peak. In nursing, this hierarchy helps in planning patient care by ensuring that fundamental needs are met before addressing higher-level needs.
-
Physiological Needs (Highest Priority): These are the most basic needs required for survival. In a healthcare context, these include:
- Airway: Ensuring a patent airway.
- Breathing: Supporting effective respiration and oxygenation.
- Circulation: Maintaining adequate blood flow and blood pressure.
- Nutrition: Providing adequate nutrition and hydration.
- Elimination: Addressing bowel and bladder function (Toileting).
- Sleep: Promoting rest and sleep.
- Comfort: Managing pain and ensuring physical comfort.
- Temperature Regulation: Maintaining normal body temperature.
-
Safety and Security Needs: Once physiological needs are met, safety and security become priorities. These include:
- Physical Safety: Preventing injury, falls, and accidents (fall precautions, side rails, clear pathways).
- Psychological Safety: Fostering a sense of trust and security (therapeutic relationship, reducing anxiety).
- Infection Control: Preventing infection through hand hygiene and appropriate isolation measures.
- Security of Environment: Ensuring a safe and predictable environment.
-
Love and Belonging Needs: These needs relate to social connection and belonging. In nursing care, this involves:
- Social Interaction: Facilitating supportive relationships and preventing social isolation (bullying prevention).
- Communication: Employing active listening and therapeutic communication techniques.
- Family Involvement: Supporting family relationships and involvement in care.
-
Self-Esteem Needs: These involve feelings of confidence, achievement, and respect. Nursing interventions can support self-esteem by:
- Promoting Independence: Encouraging patient participation in self-care and decision-making.
- Recognizing Achievements: Acknowledging and praising patient progress and efforts.
- Body Image Support: Addressing concerns related to body image disturbance and promoting self-acceptance.
-
Self-Actualization Needs (Lowest Priority in Acute Care): These are the highest-level needs, related to personal growth and fulfillment. While less often a primary focus in acute care, nurses can support self-actualization by:
- Facilitating Spiritual Growth: Supporting patients’ spiritual needs and practices.
- Promoting Goal Setting: Helping patients identify and work towards personal goals.
- Creating Empowering Environments: Fostering an environment that supports patient autonomy and self-discovery.
By applying Maslow’s Hierarchy, nurses can systematically address patient needs, starting with the most fundamental and progressing to higher-level needs as the patient’s condition stabilizes and improves.
Virginia Henderson’s 14 Needs as applied to Maslow’s Hierarchy of Needs. Learn more about it here.
Step 5: Establishing Patient Goals and Desired Outcomes
Following prioritization, the nurse and patient collaboratively set goals for each NANDA nursing diagnosis. Goals, or desired outcomes, are statements that describe the intended results of nursing care, reflecting what the nurse aims to achieve through nursing interventions. Well-defined goals:
- Provide direction for planning interventions.
- Serve as criteria for evaluating patient progress.
- Enable the nurse and patient to determine problem resolution.
- Motivate both the patient and nurse by providing a sense of accomplishment.
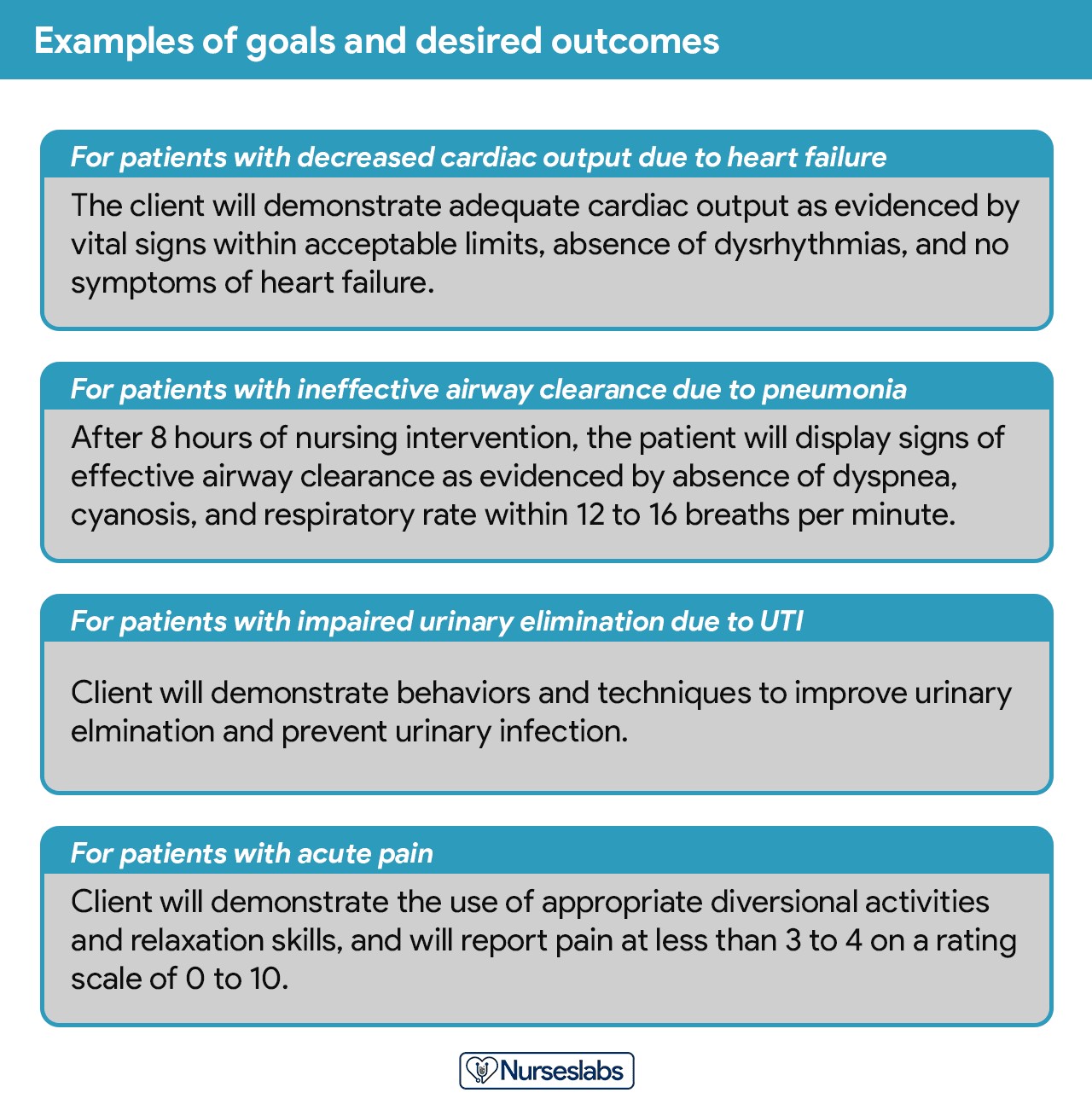
Examples of goals and desired outcomes. Notice how they’re formatted and written.
For each NANDA nursing diagnosis, an overarching goal is established. The terms “goal outcomes” and “expected outcomes” are often used interchangeably.
Effective goals should be SMART, an acronym standing for:
- Specific: Clearly defined, leaving no room for ambiguity.
- Measurable: Quantifiable, allowing for objective assessment of progress.
- Attainable: Achievable given the patient’s current condition and resources.
- Realistic: Relevant to the patient’s needs and capabilities.
- Time-Oriented: Including a timeframe for achievement.
Additionally, goals should adhere to the REEPIG standards, ensuring high-quality care planning:
- Realistic: Feasible with available resources.
- Explicitly Stated: Clearly articulated to avoid misinterpretation.
- Evidence-Based: Supported by research or best practices.
- Prioritized: Aligned with the urgency of patient needs.
- Involve: Including patient and multidisciplinary team input.
- Goal-Centered: Directly addressing the identified goals.
Short-Term and Long-Term Goals
Goals and expected outcomes must be measurable and patient-centered. They focus on problem prevention, resolution, and rehabilitation. Goals are categorized as:
- Short-Term Goals: Achievable in a short period, typically hours to days, often used in acute care settings to address immediate needs.
- Long-Term Goals: Achievable over a longer timeframe, weeks to months, common for patients with chronic conditions or in long-term care settings.
- Discharge Planning Goals: Long-term goals focused on continued care and problem resolution after discharge, often involving referrals to home health or therapy services.
Components of Well-Formulated Goals and Desired Outcomes
Goal statements typically include four key components:
- Subject: Usually the patient or a part of the patient (often implied and not explicitly stated, e.g., “patient will” is assumed).
- Verb: An action verb describing what the patient will do, learn, or experience (e.g., “will demonstrate,” “will verbalize,” “will maintain”).
- Conditions or Modifiers: Describing the circumstances under which the behavior will occur (e.g., “using crutches,” “with assistance,” “after education”).
- Criterion of Desired Performance: The standard for evaluating performance (e.g., “independently,” “correctly,” “within normal limits”). This is often optional but adds specificity.
Tips for Writing Effective Goals and Outcomes:
- Frame goals in terms of patient responses, not nurse activities. Start with “Client will…” to maintain patient focus.
- Focus on what the patient will do, not what the nurse hopes to achieve.
- Use observable, measurable terms for outcomes, avoiding vague language.
- Ensure outcomes are realistic given patient resources, limitations, and care duration.
- Verify goals are compatible with other healthcare therapies.
- Derive each goal from only one NANDA nursing diagnosis for clear evaluation.
- Ensure the patient values and considers the goals important to foster cooperation.
Step 6: Selecting Nursing Interventions
Nursing interventions are the specific actions nurses perform to help patients achieve their goals. These interventions should directly address the etiology of the NANDA nursing diagnosis. For risk diagnoses, interventions should aim to reduce risk factors. While identified during the planning phase, interventions are implemented during the implementation phase of the nursing process.
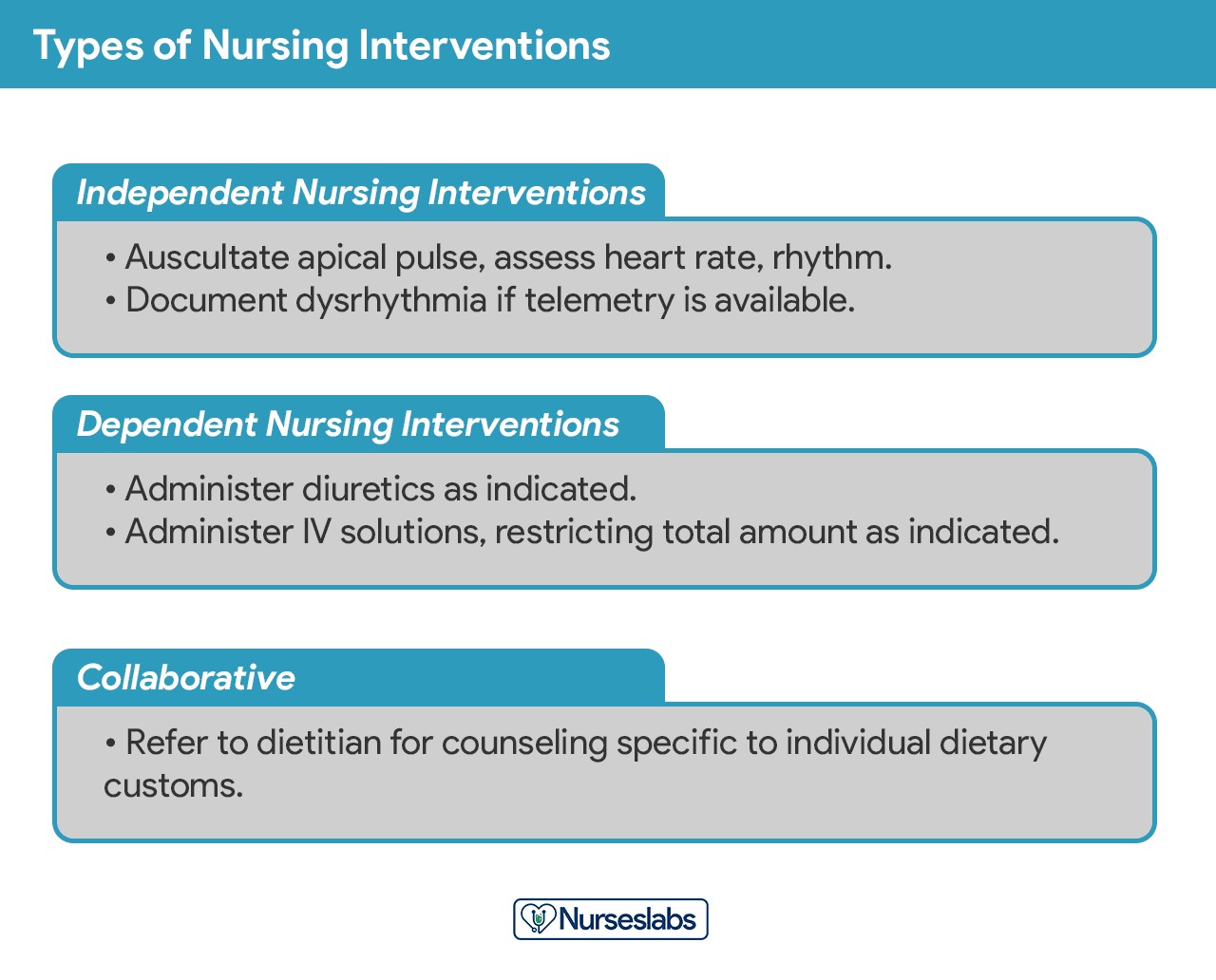
Types of Nursing Interventions
Nursing interventions are broadly categorized into:
Types of nursing interventions in a care plan.
-
Independent Nursing Interventions: Actions nurses are licensed to initiate based on their professional judgment and skills. These include:
- Ongoing assessment and monitoring.
- Emotional support and counseling.
- Providing comfort measures.
- Patient education and teaching.
- Physical care and hygiene.
- Referrals to other healthcare professionals.
-
Dependent Nursing Interventions: Actions carried out under physician’s orders or supervision. These include:
- Administering medications and intravenous therapy.
- Performing diagnostic tests.
- Implementing medical treatments.
- Managing diet and activity orders.
- Providing explanations related to medical orders.
-
Collaborative Interventions: Actions carried out in partnership with other healthcare team members (physicians, therapists, social workers, dietitians). These are developed through interdisciplinary consultation to gain diverse professional perspectives.
Effective Nursing Interventions should be:
- Safe and appropriate for the patient’s age, health, and condition.
- Achievable with available resources and time.
- Consistent with the patient’s values, culture, and beliefs.
- Aligned with other therapies the patient is receiving.
- Based on nursing knowledge, experience, and relevant scientific evidence.
Tips for Writing Nursing Interventions:
- Date and Sign the Plan: Essential for accountability, evaluation, and future planning.
- Be Specific and Clear: Start with an action verb indicating what the nurse will do. Include qualifiers (how, when, where, frequency, amount) for clarity. Examples: “Educate patient on medication side effects before discharge,” “Assess pain level every 2 hours using a pain scale.”
- Use Accepted Abbreviations: Only use abbreviations approved by the healthcare institution.
Step 7: Providing Rationales for Interventions
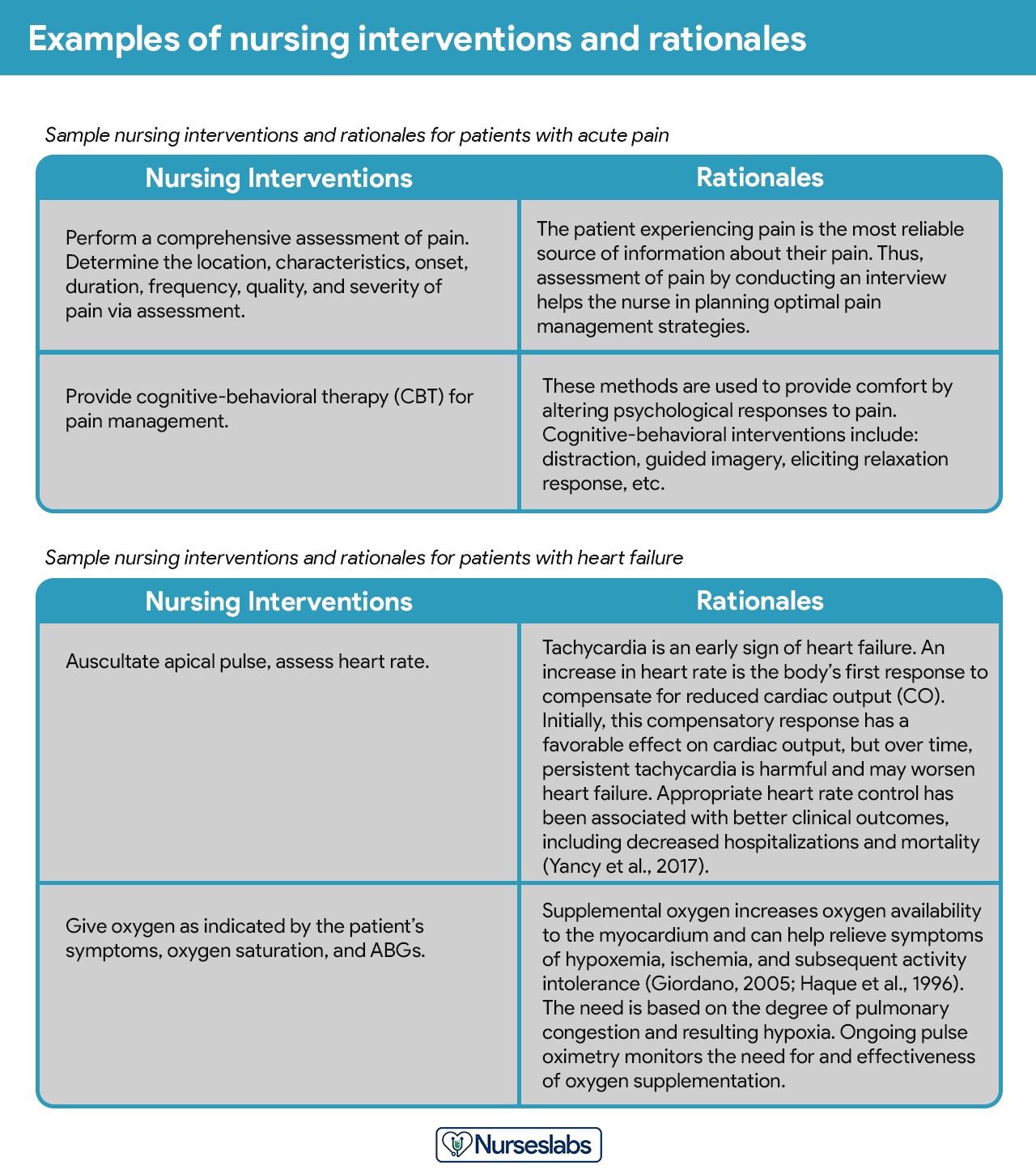
Rationales, or scientific explanations, justify why a particular nursing intervention was chosen. They explain the scientific principles that support the intervention’s effectiveness.
Sample nursing interventions and rationale for a care plan (NCP)
Rationales are particularly important in student care plans to help students connect pathophysiological and psychological principles to nursing actions. They reinforce the evidence-based nature of nursing practice. While not always included in routine care plans for practicing nurses, understanding the rationale is crucial for effective intervention selection.
Step 8: Evaluation of the Care Plan
Evaluation is a continuous, planned process to assess the patient’s progress toward achieving the set goals and to determine the effectiveness of the nursing care plan. Evaluation is a critical phase of the nursing process because its findings dictate whether interventions should be continued, modified, or discontinued.
Evaluation involves:
- Collecting Data: Gathering data related to the patient’s goal achievement.
- Comparing Data to Outcomes: Analyzing whether the patient’s current status matches the desired outcomes set in the care plan.
- Drawing Conclusions: Determining the extent to which goals have been met and the effectiveness of interventions.
- Modifying the Care Plan: Adjusting the care plan based on the evaluation findings. This may involve revising diagnoses, goals, interventions, or the overall approach.
Step 9: Documenting the Care Plan
The final step is to document the patient’s care plan according to institutional policy. The care plan becomes a part of the patient’s permanent medical record and is accessible to all members of the healthcare team.
Documentation typically includes:
- Patient Assessment Data: Relevant findings from the initial and ongoing assessments.
- NANDA Nursing Diagnoses: Clearly stated and prioritized.
- Goals and Desired Outcomes: Measurable and patient-centered.
- Nursing Interventions: Specific, detailed, and dated.
- Evaluation Findings: Regularly updated assessments of patient progress and intervention effectiveness.
- Revisions to the Care Plan: Any changes made to the plan based on evaluation.
Different healthcare facilities and nursing programs may have specific formats for care plan documentation. Many formats are designed to systematically guide users through the steps of the nursing process, often utilizing a multi-column layout for clarity and organization.
Nursing Care Plan Examples and Resources
This section provides a comprehensive list of sample nursing care plans (NCP) and NANDA nursing diagnoses across various medical conditions and health issues. These are categorized for easy navigation and use.
(Please note: The following is a categorized index of nursing care plans as provided in the original article. For the purpose of this rewritten article focusing on ‘nanda nursing diagnosis and care plans’, it’s important to emphasize that these care plans should ideally be developed using NANDA-I diagnoses. While the original list is valuable, users should always ensure they are applying current NANDA-I approved diagnoses when creating their own care plans.)
Basic Nursing and General Care Plans
| Basic Nursing & General Care Plans |
|---|
| Acute Confusion (Delirium) and Altered Mental Status |
| Acute Pain and Pain Management |
| Activity Intolerance and Generalized Weakness |
| Cancer (Oncology Nursing) |
| Caregiver Role Strain and Family Caregiver Support Systems |
| Chronic Confusion (Dementia) |
| End-of-Life Care (Hospice Care or Palliative) |
| Fall Risk and Fall Prevention |
| Fatigue and Lethargy |
| Geriatric Nursing (Older Adult) |
| Grieving and Loss |
| Hypothermia and Cold Injuries |
| Hyperthermia (Fever) |
| Impaired Swallowing (Dysphagia) |
| Insomnia and Sleep Deprivation |
| Prolonged Bed Rest |
| Risk for Injury and Patient Safety |
| Self-Care and Activities of Daily Living (ADLs) |
| Surgery (Perioperative Client) |
| Systemic Lupus Erythematosus |
| Total Parenteral Nutrition |
Surgery and Perioperative Care Plans
| Surgery and Perioperative Care Plans |
|---|
| Amputation |
| Appendectomy |
| Cholecystectomy |
| Fracture UPDATED! |
| Hemorrhoids |
| Hysterectomy |
| Ileostomy & Colostomy |
| Laminectomy (Disc Surgery) |
| Mastectomy |
| Subtotal Gastrectomy |
| Surgery (Perioperative Client) |
| Thyroidectomy |
| Total Joint (Knee, Hip) Replacement |
Cardiac Care Plans
| Cardiac Care Plans |
|---|
| Angina Pectoris (Coronary Artery Disease) |
| Cardiac Arrhythmia (Digitalis Toxicity) |
| Cardiac Catheterization |
| Cardiogenic Shock |
| Congenital Heart Disease |
| Decreased Cardiac Output & Cardiac Support |
| Heart Failure UPDATED! |
| Hypertension UPDATED! |
| Hypovolemic Shock |
| Impaired Tissue Perfusion & Ischemia |
| Myocardial Infarction |
| Pacemaker Therapy |
Endocrine and Metabolic Care Plans
| Endocrine and Metabolic Care Plans |
|---|
| Addison’s Disease |
| Cushing’s Disease |
| Diabetes Mellitus (Type 1, Type 2) UPDATED! |
| Diabetic Ketoacidosis (DKA) and Hyperglycemic Hyperosmolar Nonketotic Syndrome (HHNS) |
| Eating Disorders: Anorexia & Bulimia Nervosa |
| Fluid Volume Deficit (Dehydration & Hypovolemia) |
| Fluid Volume Excess (Hypervolemia) |
| Gestational Diabetes Mellitus |
| Hyperthyroidism |
| Hypothyroidism |
| Imbalanced Nutrition (Malnutrition) |
| Obesity & Overweight |
| Thyroidectomy |
| Unstable Blood Glucose Levels (Hyperglycemia & Hypoglycemia) |
| Acid-Base Imbalances |
|---|
| Metabolic Acidosis |
| Metabolic Alkalosis |
| Respiratory Acidosis |
| Respiratory Alkalosis |
| Electrolyte Imbalances |
|---|
| Calcium (Ca) Imbalances: Hypercalcemia and Hypocalcemia |
| Magnesium (Mg) Imbalances: Hypermagnesemia and Hypomagnesemia |
| Potassium (K) Imbalances: Hyperkalemia and Hypokalemia |
| Sodium (Na) Imbalances: Hypernatremia and Hyponatremia |
Gastrointestinal Care Plans
| Gastrointestinal Care Plans |
|---|
| Appendectomy |
| Bowel Incontinence (Fecal Incontinence) |
| Cholecystectomy |
| Constipation |
| Diarrhea Nursing Care Plan and Management |
| Cholecystitis and Cholelithiasis |
| Gastroenteritis |
| Gastroesophageal Reflux Disease (GERD) |
| Hemorrhoids |
| Hepatitis |
| Ileostomy & Colostomy |
| Inflammatory Bowel Disease (IBD) |
| Intussusception |
| Liver Cirrhosis |
| Nausea & Vomiting |
| Pancreatitis |
| Peritonitis |
| Peptic Ulcer Disease |
| Subtotal Gastrectomy |
| Umbilical and Inguinal Hernia |
Hematologic & Lymphatic Care Plans
| Hematologic & Lymphatic Care Plans |
|---|
| Anaphylactic Shock |
| Anemia UPDATED! |
| Aortic Aneurysm |
| Bleeding Risk & Hemophilia |
| Deep Vein Thrombosis |
| Disseminated Intravascular Coagulation |
| Hemophilia |
| Kawasaki Disease |
| Leukemia |
| Lymphoma |
| Sepsis and Septicemia |
| Sickle Cell Anemia Crisis |
Infectious Diseases Care Plans
| Infectious Diseases Care Plans |
|---|
| Acquired Immunodeficiency Syndrome (AIDS) (HIV Positive) |
| Acute Rheumatic Fever |
| Dengue Hemorrhagic Fever |
| Herpes Zoster (Shingles) |
| Influenza (Flu) |
| Pulmonary Tuberculosis |
| Risk for Infection & Infection Control |
Integumentary Care Plans
| Integumentary Care Plans |
|---|
| Burn Injury |
| Dermatitis |
| Herpes Zoster (Shingles) |
| Pressure Ulcer (Bedsores) |
| Wound Care and Skin/Tissue Integrity |
Maternal and Newborn Care Plans
| Maternal and Newborn Care Plans |
|---|
| Abortion (Termination of Pregnancy) |
| Cervical Insufficiency (Premature Dilation of the Cervix) |
| Cesarean Birth |
| Cleft Palate and Cleft Lip |
| Gestational Diabetes Mellitus |
| Hyperbilirubinemia (Jaundice) |
| Labor Stages, Induced, Augmented, Dysfunctional, Precipitous Labor |
| Neonatal Sepsis |
| Perinatal Loss (Miscarriage, Stillbirth) |
| Placental Abruption |
| Placenta Previa |
| Postpartum Hemorrhage |
| Postpartum Thrombophlebitis |
| Prenatal Hemorrhage |
| Preeclampsia and Gestational Hypertension |
| Prenatal Infection |
| Preterm Labor |
| Puerperal & Postpartum Infections |
| Substance (Alcohol and Drug) Abuse in Pregnancy |
Mental Health and Psychiatric Care Plans
| Mental Health and Psychiatric Care Plans |
|---|
| Alcohol Withdrawal |
| Anxiety & Fear |
| Anxiety and Panic Disorders |
| Bipolar Disorders |
| Body Image Disturbance & Self-Esteem |
| Impaired Thought Processes & Cognitive Impairment |
| Major Depression |
| Personality Disorders |
| Schizophrenia |
| Sexual Assault |
| Substance Dependence and Abuse |
| Suicide Behaviors |
Musculoskeletal Care Plans
| Musculoskeletal Care Plans |
|---|
| Amputation |
| Congenital Hip Dysplasia |
| Fracture UPDATED! |
| Impaired Physical Mobility & Immobility |
| Juvenile Rheumatoid Arthritis |
| Laminectomy (Disc Surgery) |
| Osteoarthritis |
| Osteogenic Sarcoma (Osteosarcoma) |
| Osteoporosis |
| Rheumatoid Arthritis |
| Scoliosis |
| Spinal Cord Injury |
| Total Joint (Knee, Hip) Replacement |
Neurological Care Plans
| Neurological Care Plans |
|---|
| Alzheimer’s Disease UPDATED! |
| Brain Tumor |
| Cerebral Palsy |
| Cerebrovascular Accident (Stroke) UPDATED! |
| Guillain-Barre Syndrome |
| Meningitis |
| Multiple Sclerosis |
| Parkinson’s Disease |
| Seizure Disorder |
| Spinal Cord Injury |
Ophthalmic Care Plans
| Ophthalmic Care Plans |
|---|
| Cataracts |
| Glaucoma |
| Macular Degeneration |
Pediatric Nursing Care Plans
| Pediatric Nursing Care Plans |
|---|
| Child Abuse |
| Cleft Lip and Cleft Palate |
| Dying Child |
| Febrile Seizure |
| Hospitalized Child |
| Hydrocephalus |
| Otitis Media |
| Spina Bifida |
| Tonsillitis and Adenoiditis |
Reproductive Care Plans
| Reproductive Care Plans |
|---|
| Cryptorchidism (Undescended Testes) |
| Hysterectomy |
| Hypospadias and Epispadias |
| Mastectomy |
| Menopause |
| Prostatectomy |
Respiratory Care Plans
| Respiratory Care Plans |
|---|
| Airway Clearance Therapy & Coughing |
| Apnea |
| Asthma UPDATED! |
| Aspiration Risk & Aspiration Pneumonia |
| Bronchiolitis UPDATED! |
| Bronchopulmonary Dysplasia (BPD) UPDATED! |
| Chronic Obstructive Pulmonary Disease (COPD) UPDATED! |
| Croup Syndrome |
| Cystic Fibrosis UPDATED! |
| Epiglottitis |
| Hemothorax and Pneumothorax UPDATED! |
| Ineffective Breathing Pattern (Dyspnea) |
| Impairment of Gas Exchange |
| Influenza (Flu) UPDATED! |
| Lung Cancer UPDATED! |
| Mechanical Ventilation |
| Near-Drowning |
| Pleural Effusion |
| Pneumonia |
| Pulmonary Embolism |
| Pulmonary Tuberculosis |
| Tracheostomy |
Urinary Care Plans
| Urinary Care Plans |
|---|
| Acute Glomerulonephritis |
| Acute Renal Failure |
| Benign Prostatic Hyperplasia (BPH) |
| Chronic Renal Failure |
| Hemodialysis |
| Nephrotic Syndrome |
| Peritoneal Dialysis |
| Urolithiasis (Renal Calculi) |
| Urinary Elimination (Urinary Incontinence & Urinary Retention) |
| Urinary Tract Infection |
| Vesicoureteral Reflux (VUR) |
| Wilms Tumor (Nephroblastoma) |
Recommended Resources for NANDA Nursing Diagnosis and Care Plans
To further enhance your skills in developing effective nursing care plans and utilizing NANDA nursing diagnoses, consider these highly recommended resources:
Disclosure: The following are affiliate links from Amazon. We may earn a small commission from purchases, at no additional cost to you. For more details, please review our privacy policy.
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
This handbook is invaluable for its evidence-based approach to nursing interventions. It offers a user-friendly, three-step system to guide you through patient assessment, NANDA nursing diagnosis, and care plan development. It provides step-by-step instructions for implementing care and evaluating patient outcomes, enhancing your diagnostic reasoning and critical thinking skills.
Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
This comprehensive resource features over two hundred care plans, aligned with the latest evidence-based guidelines and NANDA-I diagnoses. This edition includes new care plans addressing LGBTQ health issues, electrolyte imbalances, and acid-base balance, making it an up-to-date and inclusive guide.
Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
A quick and efficient reference tool that provides all necessary information to identify accurate NANDA diagnoses for effective patient care planning. The latest edition features the most current nursing diagnoses and interventions, with an alphabetized listing covering over 400 disorders, facilitating rapid access to essential information.
Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
This manual is essential for identifying interventions to plan, individualize, and document care for over 800 diseases and disorders. It uniquely provides subjective and objective data, sample clinical applications, prioritized actions/interventions with rationales, and a comprehensive documentation section for each NANDA diagnosis, making it an indispensable tool for detailed care planning.
This e-book offers over 100 care plans across medical-surgical, maternity/OB, pediatrics, and psychiatric-mental health nursing, all utilizing NANDA-I diagnoses. Its interprofessional “patient problems” approach familiarizes you with patient-centered communication and collaborative care strategies.
By utilizing these resources and diligently applying the steps outlined in this guide, nurses can master the art and science of developing Nanda Nursing Diagnosis And Care Plans, ultimately enhancing patient outcomes and contributing to excellence in nursing practice.