Introduction
The prompt diagnosis of cancer is critical, yet standardized methods for measuring its timeliness remain elusive. While the interval between a patient’s first presentation of cancer symptoms to a general practitioner (GP) and their subsequent referral to a specialist (the primary care interval) is a recognized metric, the number of GP consultations prior to referral is increasingly utilized as an indicator of diagnostic speed. This study, leveraging data from the National Audit Of Cancer Diagnosis In Primary Care, delves into the relationship between these two measures – primary care interval and pre-referral consultations – to evaluate the latter’s validity as a proxy for diagnostic timeliness. Understanding this association is crucial for developing effective strategies to expedite cancer diagnosis and improve patient outcomes within primary care settings.
Both the primary care interval and the number of pre-referral consultations offer unique perspectives on the diagnostic pathway, each with inherent strengths and limitations. Investigating their correlation is paramount. A strong correlation would suggest that either measure could reliably serve in research and quality monitoring. Conversely, a weak correlation would cast doubt on the use of pre-referral consultations as a measure of diagnostic timeliness. Crucially, if the number of pre-referral consultations accurately reflects the primary care interval, interventions aimed at reducing consultations could directly enhance the speed of cancer diagnosis. Such efforts might include improving GPs’ ability to recognize cancer symptoms during consultations, potentially through the integration of clinical decision support tools. This research, therefore, aims to rigorously examine the association between pre-referral consultations and primary care intervals, using data from a comprehensive national audit.
Materials and Methods
This study is grounded in the analysis of data from the National Audit of Cancer Diagnosis in Primary Care, conducted in England during 2009–2010. This audit was a key component of the National Awareness and Early Diagnosis Initiative, a program designed to improve cancer outcomes through earlier detection and intervention. Data collection was facilitated by GPs and other healthcare professionals across approximately 1170 general practices in England, representing about 14% of all practices and participating on a voluntary basis. Comparisons with national cancer registration data have confirmed the audit’s robust representativeness of the broader cancer patient population.
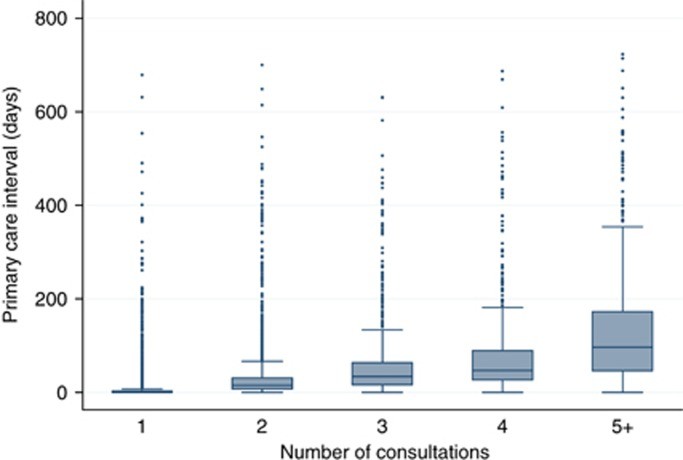
The analysis focused on patients aged 15 years and older who had complete records for both the number of pre-referral consultations and the primary care interval, with intervals ranging from 0 to 730 days. To ensure sufficient statistical power, the study concentrated on the 18 most prevalent cancer types identified within the audit. For each category of pre-referral consultations, we calculated the median primary care interval in days, along with the inter-quartile range. This analysis was performed for the entire cohort and then stratified by cancer type to identify cancer-specific patterns. Box plots were employed to visually represent these data distributions, highlighting the variability in primary care intervals across consultation categories.
Given that primary care interval data typically exhibit a right-skewed distribution, the Spearman’s rank correlation coefficient was used to assess the strength of the association between the number of pre-referral consultations and the primary care interval. This non-parametric measure is well-suited for ordinal data and robust to outliers. Furthermore, Receiver Operating Characteristic (ROC) curve analysis was conducted to evaluate the predictive capability of pre-referral consultations for identifying prolonged primary care intervals. For this ROC analysis, the primary care interval was treated as a continuous outcome, and the number of pre-referral consultations was dichotomized into ‘three or more’ versus ‘one or two’ consultations, aligning with categorization used in UK health policy. Linear regression models were utilized to explore whether the relationship between these measures varied across different patient subgroups, considering factors such as age, sex, ethnicity, and cancer type. Due to the non-normal distribution of the data, statistical significance testing was performed using bootstrapping with 1000 samples to provide more robust p-values.
Results
The analysis included 13,035 patients, revealing a median primary care interval of 5 days, with an inter-quartile range of 0–23 days. A significant majority of patients (82%) were referred after either one (57.5%) or two (24.6%) GP consultations. These groups exhibited median primary care intervals of 0 (inter-quartile range 0–3 days) and 15 days (inter-quartile range 7–31 days), respectively. Conversely, a smaller proportion (18%) required three or more consultations before referral: 9.2% with three consultations, 3.9% with four, and 4.8% with five or more. These patients experienced considerably longer median primary care intervals of 34 days (inter-quartile range 16–64), 47 days (inter-quartile range 27–90), and 97 days (inter-quartile range 46–173), respectively. This data underscores a clear trend: as the number of pre-referral consultations increases, so does the primary care interval.
Table 1. Median primary care interval (number of days) and inter-quartile range by pre-referral consultations category (n=13 035).
| Median primary care interval by number of pre-referral consultations category (1**–5+)** | ||||||
|---|---|---|---|---|---|---|
| N | % Of patients with 3+ consultations | Median primary care interval, all patients (n=13 035/100%) | Inter-quartile range | 1 (**n=7499/57.5%)** | Inter-quartile range | |
| All patients | 13 035 | 17.9 | 5 | 0–23 | 0 | 0–3 |
| By cancer | ||||||
| Multiple myeloma | 176 | 46.0 | 21 | 5–55 | 1 | 0–12 |
| Unknown primary | 136 | 41.2 | 14 | 0–37.5 | 0 | 0–3 |
| Stomach | 237 | 32.1 | 14 | 0–57 | 0 | 0–4.5 |
| Lung | 1421 | 32.8 | 14 | 3–40 | 3 | 0–10 |
| Renal | 272 | 22.1 | 12 | 1–37 | 1 | 0–12.5 |
| Prostate | 2201 | 15.2 | 12 | 3–28 | 4 | 0–13 |
| Lymphoma | 590 | 25.8 | 9 | 0–32 | 1 | 0–5 |
| Pancreatic | 303 | 31.4 | 8 | 1–35 | 0 | 0–4 |
| Ovarian | 324 | 27.8 | 8 | 0–27 | 0 | 0–5 |
| Oesophageal | 500 | 22.6 | 7 | 0–33 | 0 | 0–1 |
| Colorectal | 1999 | 21.3 | 7 | 0–32 | 0 | 0–3.5 |
| Leukaemia | 358 | 17.6 | 6.5 | 0–23 | 1 | 0–6 |
| Oropharyngeal | 178 | 21.9 | 6 | 0–27 | 0 | 0–3 |
| Brain | 159 | 21.4 | 4 | 0–19 | 0 | 0–1.5 |
| Bladder | 721 | 14.6% | 4 | 0–18 | 0 | 0–3 |
| Endometrial | 358 | 9.8 | 1 | 0–19 | 0 | 0–2 |
| Melanoma | 735 | 5.4 | 0 | 0–6 | 0 | 0–1 |
| Breast | 2367 | 2.9 | 0 | 0–1 | 0 | 0–0 |
| By referral type | ||||||
| ‘Routine’ | 2030 | 24.4 | 13 | 1–42 | 1 | 0–7 |
| ‘Other’ | 1122 | 19.1 | 5 | 0–26 | 0 | 0–5 |
| ‘Emergency’ | 1642 | 25.9 | 4 | 0–21 | 0 | 0–2 |
| ‘Two-week’ referral | 824 | 14.5 | 3 | 0–20 | 0 | 0–2 |
This pattern was consistently observed across all 18 cancer types examined. Notably, patients diagnosed with multiple myeloma and lung cancer had the highest proportions of three or more pre-referral consultations (46% and 32.8%, respectively) and correspondingly longer median primary care intervals (21 and 14 days). In contrast, patients with breast cancer and melanoma showed the lowest proportions of three or more pre-referral consultations (2.9% and 5.4%, respectively) and the shortest median primary care intervals (0 days for both). This variation across cancer types suggests that the nature of the cancer and its symptomatic presentation significantly influence the diagnostic pathway within primary care.
Figure 1 visually represents the distribution of primary care intervals for each category of pre-referral consultations, reinforcing the trend of increasing intervals with more consultations.
For the entire cohort of patients with any of the 18 cancers, the Spearman’s rank correlation coefficient between the number of pre-referral consultations and the primary care interval was 0.70 (p<0.001), indicating a strong positive correlation. Spearman’s rank correlation coefficients for individual cancer types ranged from 0.55 for prostate cancer to 0.77 for brain cancer, demonstrating at least a moderate correlation across all cancer types. The ROC area under the curve (AUC) for predicting three or more pre-referral consultations using primary care interval was 0.88, with 95% confidence intervals of 0.87 to 0.89, indicating good discriminatory ability. Sensitivity analysis using different binary cut-offs for pre-referral consultations yielded similar ROC AUC values, confirming the robustness of this finding.
Table 2. Spearman’s rank correlation co-efficient and ROC AUC values for the association between primary care interval and category of number of pre-referral consultations (n=13 035).
| N | Spearman’s r | Spearman’s *r P-***value** | ROC area under the curvea | ROC area 95% lower CI | ROC area 95% upper CI | |
|---|---|---|---|---|---|---|
| All patients | 13035 | 0.70 | 0.88 | 0.87 | 0.89 | |
| By cancer | ||||||
| Breast | 2367 | 0.56 | 0.96 | 0.93 | 0.98 | |
| Prostate | 2201 | 0.55 | 0.84 | 0.82 | 0.86 | |
| Colorectal | 1999 | 0.71 | 0.86 | 0.84 | 0.88 | |
| Lung | 1421 | 0.62 | 0.83 | 0.81 | 0.86 | |
| Melanoma | 735 | 0.61 | 0.87 | 0.81 | 0.94 | |
| Bladder | 721 | 0.72 | 0.90 | 0.87 | 0.93 | |
| Lymphoma | 590 | 0.70 | 0.87 | 0.84 | 0.90 | |
| Oesophageal | 500 | 0.75 | 0.87 | 0.84 | 0.91 | |
| Endometrial | 358 | 0.64 | b | 0.89 | 0.84 | 0.94 |
| Leukaemia | 358 | 0.59 | 0.81 | 0.76 | 0.87 | |
| Ovarian | 324 | 0.68 | 0.86 | 0.82 | 0.91 | |
| Pancreatic | 303 | 0.71 | 0.89 | 0.85 | 0.93 | |
| Renal | 272 | 0.60 | 0.84 | 0.79 | 0.90 | |
| Stomach | 237 | 0.76 | 0.88 | 0.83 | 0.92 | |
| Oropharyngeal | 178 | 0.72 | 0.85 | 0.79 | 0.91 | |
| Multiple myeloma | 176 | 0.73 | 0.88 | 0.83 | 0.93 | |
| Brain | 159 | 0.77 | 0.92 | 0.87 | 0.96 | |
| Unknown primary | 136 | 0.76 | 0.87 | 0.81 | 0.93 | |
| By referral type | ||||||
| ‘Two-week’ referral | 8241 | 0.72 | 0.89 | 0.88 | 0.90 | |
| ‘Emergency’ | 1642 | 0.72 | b | 0.88 | 0.87 | 0.90 |
| ‘Routine’ | 2030 | 0.67 | 0.85 | 0.83 | 0.87 | |
| ‘Other’ | 1122 | 0.67 | 0.88 | 0.85 | 0.90 |
Linear regression analysis revealed no significant interactions between the number of pre-referral consultations and patient demographics such as age, sex, or ethnicity. However, a significant interaction was observed with cancer type (p<0.001), indicating that the strength of the association varies across different cancers. Furthermore, while there was a statistically significant interaction with referral type (p=0.016), the association between pre-referral consultations and primary care interval remained robust across all referral types, ranging from Spearman’s r of 0.67 for routine referrals to 0.72 for ‘two-week’ referrals.
Discussion
The findings from this National Audit of Cancer Diagnosis in Primary Care provide compelling evidence that the number of pre-referral consultations is a valid measure for assessing the primary care interval in cancer diagnosis. The consistently strong and positive correlation between these two measures across a large cohort and various cancer types underscores the utility of pre-referral consultations as a readily available indicator of diagnostic timeliness. The study highlights that cancers requiring more consultations tend to be associated with longer primary care intervals, such as multiple myeloma, while cancers like breast cancer, which are often diagnosed more swiftly, typically involve fewer consultations.
These results offer valuable insights into potential improvements in diagnostic timelines. For instance, the substantial difference in median primary care intervals between patients requiring five or more consultations compared to those requiring fewer consultations suggests a considerable window for improvement. Reducing the number of pre-referral consultations, especially for cancers where multiple consultations are common, could lead to significant reductions in the overall time to diagnosis. It is important to note that these potential gains represent a theoretical maximum, achievable under ideal conditions where symptom presentation and access to diagnostic resources are optimized.
While the correlation between pre-referral consultations and primary care interval might appear intuitive, empirical evidence supporting this association has been limited. This study adds substantial weight to the notion that diagnostic delays in primary care are often reflected in a higher number of consultations. The findings also reinforce existing evidence suggesting that diagnosing cancers with non-specific symptoms (e.g., multiple myeloma, stomach cancer) is inherently more complex than diagnosing cancers with more distinct presentations (e.g., breast cancer, melanoma).
Strengths of this study include its large sample size, the broad range of cancer types included, and the application of robust statistical methods. However, certain limitations should be considered. Potential misclassification of consultations due to recording inaccuracies or symptom misattribution, particularly in patients with comorbidities, cannot be entirely ruled out. Although the audit data were not independently validated, consistency with patient-reported experiences in the Cancer Patient Experience Survey lends credibility to the findings. Generalizability should be considered cautiously, as participating practices may differ from non-participating practices in terms of organizational factors and care quality. Finally, the study could not determine whether prolonged primary care intervals or multiple pre-referral consultations were justifiable or preventable in individual cases.
Considering the implications for clinical practice and policy, a more proactive approach to referral and investigation for patients presenting with non-specific symptoms might reduce the number of consultations needed for diagnosis. However, this must be balanced against the potential for increased patient anxiety and healthcare costs associated with investigations for benign conditions. Expanding GP access to specialist diagnostic tests is increasingly advocated and could play a role in reducing pre-referral consultations. Future research should focus on monitoring the impact of GP-led investigations on diagnostic timeliness and resource utilization, potentially through primary care audit programs that include diagnostic imaging and endoscopy use. Point-of-care diagnostic technologies also hold promise for reducing the number of consultations before referral and warrant further development and evaluation.
The findings strongly support interventions aimed at enhancing GPs’ ability to accurately and promptly assess cancer symptoms, such as the implementation of clinical decision support tools. Furthermore, public health initiatives to raise patient awareness of persistent symptoms could help reduce delays between consultations, although this may not directly impact the number of consultations required. Future research and policy efforts should prioritize cancers that are ‘difficult-to-suspect’ due to vague or non-specific symptoms (e.g., multiple myeloma, lung, stomach, and pancreatic cancer), as these are typically associated with longer primary care intervals and more pre-referral consultations.
Conclusion
In conclusion, both the number of pre-referral consultations and the primary care interval are valid and interconnected measures of the timeliness of cancer diagnosis within primary care. Improving GPs’ ability to effectively evaluate cancer symptoms should be a key focus for research and policy initiatives aimed at accelerating cancer diagnosis. Development and evaluation of interventions should particularly target cancers that are challenging to diagnose due to non-specific symptom presentation.
Acknowledgments
The authors express their sincere gratitude to all primary care professionals in participating practices for their diligent data collection and submission. We also acknowledge the support from respective Cancer Networks, the Royal College of General Practitioners, and the National Cancer Action Team for their contributions to the audit. Data access for this research was granted by the National Audit of Cancer Diagnosis in Primary Care steering group, in line with the project’s aim to utilize anonymous data for early diagnosis research. This study was supported by a Post-Doctoral Fellowship awarded to GL by the National Institute for Health Research. The views expressed are those of the authors and do not necessarily reflect the official positions of the NHS, the National Institute for Health Research, or the Department of Health.