In the dynamic field of healthcare, the focus is increasingly shifting towards preventative strategies and holistic well-being. As healthcare professionals, especially nurses, we are at the forefront of this movement, championing health promotion and wellness. A cornerstone of this approach lies in the effective use of nursing diagnoses, particularly wellness diagnoses, and translating them into actionable nursing care plans. This guide will delve into the intricacies of developing nursing care plans specifically tailored for wellness diagnoses, equipping you with the knowledge and tools to excel in promoting patient well-being.
Understanding Nursing Diagnosis in Wellness
A nursing diagnosis is a critical thinking process and clinical judgment that nurses use to describe a patient’s health condition or vulnerability to a condition. It’s not about identifying diseases (that’s the realm of medical diagnoses), but rather about understanding a patient’s response to health and life processes. This distinction is crucial, especially when we talk about wellness.
Wellness diagnoses, also known as health promotion diagnoses, are a specific type of nursing diagnosis. They focus on a patient’s strengths and their desire to enhance their well-being. Unlike problem-focused or risk diagnoses, wellness diagnoses are positive and proactive. They identify an individual’s readiness to improve their health status and engage in healthier behaviors.
The Purpose of Wellness Diagnoses
Wellness diagnoses serve several vital purposes in nursing practice:
- Empowering Patients: They shift the focus from illness to health, empowering patients to take an active role in their well-being.
- Promoting Health Behaviors: By identifying areas where patients are ready to improve, nurses can create targeted interventions to foster healthier lifestyles.
- Guiding Preventative Care: Wellness diagnoses are fundamental in preventative care, helping nurses anticipate and address potential health issues before they arise.
- Enhancing Holistic Care: They encourage a holistic approach to patient care, considering not just the absence of disease but also the presence of well-being in all dimensions of life.
- Facilitating Personalized Care: Wellness diagnoses allow for individualized care plans that are tailored to a patient’s specific needs, preferences, and readiness to change.
Wikipedia.com**
Wellness Diagnosis vs. Other Types of Nursing Diagnoses
To fully grasp the significance of wellness diagnoses, it’s essential to differentiate them from other types:
-
Problem-Focused Diagnosis (Actual Diagnosis): This type identifies an existing health problem. It’s based on present signs and symptoms. For example, “Acute Pain related to surgical incision as evidenced by patient reporting pain of 7/10 and guarding behavior.”
-
Risk Diagnosis: This diagnosis identifies potential problems. It indicates that a patient is vulnerable to developing a health issue due to certain risk factors. For example, “Risk for Infection as evidenced by surgical wound and compromised immune system.”
-
Syndrome Diagnosis: This diagnosis represents a cluster of actual or risk diagnoses that frequently occur together. For example, “Rape Trauma Syndrome.”
Key Difference: Wellness diagnoses are unique because they do not focus on problems or risks. Instead, they highlight a patient’s strengths and readiness to improve their health. They are about potential for growth and enhancement, not about deficits or vulnerabilities.
The Link: Wellness Diagnosis and Nursing Care Plans
A nursing care plan is a roadmap for patient care. It’s a formal process that outlines the nursing care needed to address a patient’s needs and achieve specific health outcomes. When it comes to wellness diagnoses, the nursing care plan becomes a proactive strategy to facilitate health enhancement.
The Nursing Process and Wellness Diagnoses:
The nursing process is a systematic approach to patient care, consisting of five steps: Assessment, Diagnosis, Planning, Implementation, and Evaluation (ADPIE). Wellness diagnoses are integrated into this process as follows:
-
Assessment: The nurse assesses the patient’s current health status, lifestyle, values, and readiness to enhance wellness. This involves identifying strengths, areas for potential improvement, and the patient’s motivation for change.
-
Diagnosis: Based on the assessment data, the nurse formulates a wellness diagnosis. This diagnosis identifies the patient’s readiness to improve a specific aspect of their health. Examples include “Readiness for Enhanced Nutrition” or “Readiness for Enhanced Sleep.”
-
Planning: This is where the nursing care plan for the wellness diagnosis is developed. It involves setting goals (desired outcomes for enhanced wellness), and planning nursing interventions (actions to help the patient achieve those goals).
-
Implementation: The nurse puts the care plan into action. This involves carrying out the planned interventions, such as providing education, counseling, or support to promote healthier behaviors.
-
Evaluation: The nurse evaluates the effectiveness of the care plan. This involves assessing whether the patient has achieved the desired wellness outcomes and adjusting the plan as needed.
Creating Nursing Care Plans for Wellness Diagnoses: A Step-by-Step Guide
Developing effective nursing care plans for wellness diagnoses requires a thoughtful and patient-centered approach. Here’s a step-by-step guide:
Step 1: Accurate Assessment Focused on Wellness
- Identify Strengths: Focus on what the patient is doing well. What healthy habits do they already have? What are their resources and support systems?
- Assess Readiness for Enhancement: Is the patient motivated to improve their health in a specific area? Are they expressing interest or asking questions about wellness topics?
- Explore Values and Beliefs: Understand what wellness means to the patient. What are their health priorities and values?
- Gather Subjective and Objective Data: Collect information through patient interviews, observations, and relevant health records. Focus on areas related to health promotion, such as nutrition, exercise, stress management, sleep, and social connections.
Step 2: Formulating the Wellness Diagnosis
-
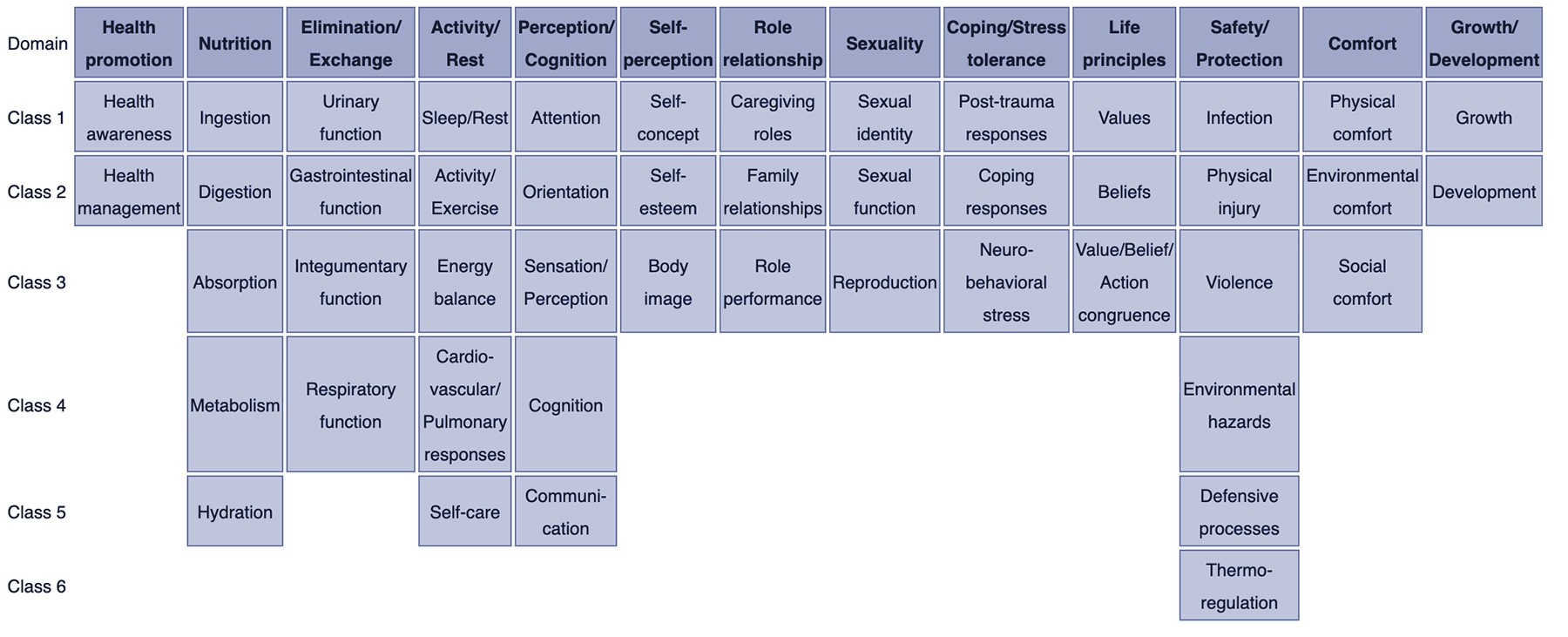
Use NANDA-I Approved Diagnoses: Refer to the NANDA-I (North American Nursing Diagnosis Association International) list of nursing diagnoses. Look for diagnoses related to “Readiness for Enhanced…” in various health domains. Examples include:
- Readiness for Enhanced Nutrition
- Readiness for Enhanced Knowledge
- Readiness for Enhanced Sleep
- Readiness for Enhanced Spiritual Well-being
- Readiness for Enhanced Self-Care
-
Keep it Concise: Wellness diagnoses are typically one-part statements, simply stating the “Readiness for Enhanced…” and the area of wellness. For instance, “Readiness for Enhanced Family Coping.”
Step 3: Setting Wellness Goals (Desired Outcomes)
- Patient-Centered Goals: Goals should be developed in collaboration with the patient and reflect what they want to achieve in terms of wellness enhancement.
- Specific, Measurable, Achievable, Relevant, Time-bound (SMART): Ensure goals are well-defined, quantifiable, realistic, aligned with the patient’s values, and have a timeframe for achievement.
- Focus on Positive Outcomes: Goals should describe the desired state of enhanced wellness. For example, instead of “Reduce sedentary behavior,” a wellness goal could be “Patient will increase daily physical activity to 30 minutes of moderate exercise within 4 weeks.”
Step 4: Planning Wellness Interventions
- Education and Information: Provide patients with accurate and relevant information about health promotion topics. Tailor the education to their learning style and level of understanding.
- Counseling and Support: Offer guidance and support to help patients make healthy behavior changes. This might involve motivational interviewing, problem-solving, and building self-efficacy.
- Skills Training: Teach patients practical skills they need to adopt healthier habits. For example, cooking healthy meals, stress management techniques, or exercise routines.
- Resource Referral: Connect patients with community resources that can support their wellness goals. This could include nutritionists, fitness centers, support groups, or smoking cessation programs.
- Environmental Modifications: Suggest changes in the patient’s environment to support healthy choices. For example, creating a home exercise space or stocking the kitchen with healthy foods.
- Collaborative Approaches: Work with other healthcare professionals (dietitians, physical therapists, health educators) to provide comprehensive wellness support.
Step 5: Implementation and Evaluation
- Implement Interventions: Carry out the planned interventions consistently and patiently. Build rapport with the patient and provide ongoing encouragement.
- Monitor Progress: Regularly assess the patient’s progress towards their wellness goals. Track relevant indicators, such as changes in behavior, knowledge, or self-reported well-being.
- Evaluate Goal Achievement: Determine if the patient has met their wellness goals within the established timeframe.
- Modify the Care Plan: If goals are not being met or if the patient’s needs change, revise the care plan. Adjust interventions, modify goals, or re-assess the wellness diagnosis as needed.
Example: Nursing Care Plan for “Readiness for Enhanced Nutrition”
Let’s illustrate with an example of a nursing care plan for the wellness diagnosis “Readiness for Enhanced Nutrition.”
Patient Scenario: A 45-year-old woman expresses interest in improving her diet to increase energy levels and maintain a healthy weight. She reports currently eating a diet high in processed foods and often skips breakfast. She is motivated to make changes but feels unsure where to start.
1. Assessment:
- Strengths: Patient is motivated to improve her diet and recognizes the need for change.
- Readiness for Enhancement: Expresses clear interest in nutrition and asks for guidance.
- Values/Beliefs: Values healthy weight and increased energy levels.
- Data: Diet history reveals high intake of processed foods, infrequent breakfast consumption. BMI is in the overweight range.
2. Wellness Diagnosis: Readiness for Enhanced Nutrition
3. Goals (Desired Outcomes):
- Short-term Goal (within 2 weeks): Patient will identify 3-4 strategies to incorporate more fruits and vegetables into her daily diet.
- Long-term Goal (within 2 months): Patient will consistently consume a balanced diet that includes whole grains, lean protein, fruits, and vegetables, as evidenced by a food journal and self-report.
4. Nursing Interventions:
- Education: Provide patient with information about balanced nutrition, portion control, and the benefits of fruits and vegetables. Use visual aids and handouts.
- Meal Planning Guidance: Help the patient create a sample meal plan that incorporates more fruits, vegetables, and whole grains.
- Healthy Recipe Resources: Share healthy recipes and cooking tips.
- Grocery Shopping Strategies: Discuss strategies for making healthy choices at the grocery store, such as reading food labels and planning shopping lists.
- Support and Encouragement: Offer ongoing support and encouragement. Follow up regularly to discuss progress and address challenges.
5. Evaluation:
- Ongoing Monitoring: Review the patient’s food journal weekly to assess dietary changes. Discuss her experiences and provide feedback.
- Goal Evaluation: At 2 weeks, evaluate if the patient can identify 3-4 strategies for increasing fruit and vegetable intake. At 2 months, evaluate if she is consistently following a balanced diet based on her food journal and self-report.
- Plan Modification: Adjust interventions as needed based on the patient’s progress and feedback. For example, if she struggles with meal planning, provide more detailed guidance and examples.
Optimizing Wellness in Nursing Practice
Integrating wellness diagnoses and care plans into nursing practice is not just about following a process; it’s about embracing a philosophy of care that prioritizes health promotion and patient empowerment.
Key Considerations for Optimization:
- Shift in Mindset: Move from a primarily disease-focused approach to a wellness-oriented approach. Recognize that promoting health is just as important as treating illness.
- Education and Training: Ensure nurses are adequately trained in wellness assessment, wellness diagnosis formulation, and the development of health promotion care plans.
- Interdisciplinary Collaboration: Foster collaboration with other healthcare professionals to provide comprehensive wellness services.
- Patient Engagement: Actively involve patients in the wellness planning process. Make care plans truly patient-centered and tailored to their individual needs and preferences.
- Documentation and Communication: Document wellness diagnoses and care plans clearly in patient records. Communicate wellness goals and interventions to the entire healthcare team.
- Evaluation of Outcomes: Track the impact of wellness interventions on patient outcomes. Use data to improve wellness programs and care planning strategies.
By embracing wellness diagnoses and diligently crafting nursing care plans for health promotion, nurses can make a profound difference in the lives of their patients, fostering not just the absence of disease, but the presence of genuine well-being. This proactive and empowering approach is the future of nursing and healthcare, leading to healthier individuals and communities.
Recommended Resources
To deepen your understanding and skills in nursing diagnosis and care planning, consider these resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: A comprehensive guide with evidence-based interventions for various nursing diagnoses.
- Nursing Care Plans – Nursing Diagnosis & Intervention: Offers a wide range of care plans reflecting current evidence-based practice, including wellness-focused plans.
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick reference tool for identifying diagnoses and planning care efficiently.
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: Provides detailed information on diagnoses, interventions, and documentation.
- All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: A comprehensive resource covering diverse patient populations and care settings.
References and Sources
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- NANDA International, Inc. (2018). Nursing diagnoses: Definitions and classification 2018-2020. Eleventh edition.