Crafting a robust nursing care plan is a cornerstone of exceptional patient care. It’s a detailed roadmap that guides nurses in addressing patient needs, setting goals, and implementing effective interventions. At the heart of creating these care plans lies the crucial step of nursing diagnosis. Selecting the right nursing diagnosis is paramount, as it dictates the entire direction of the care plan. To master this essential skill, nursing professionals and students alike often turn to specialized resources, and Nursing Diagnosis Books For Care Plans stand out as indispensable tools.
This comprehensive guide delves into the world of nursing diagnosis books, exploring why they are essential for developing superior care plans. We will explore the features that make these books valuable, recommend some of the top resources available, and guide you on how to effectively utilize them to enhance your care planning process.
Understanding Nursing Care Plans and Their Importance
A nursing care plan (NCP) is more than just a document; it’s a dynamic and systematic approach to patient care. It serves as a formal blueprint that meticulously identifies a patient’s current health needs and anticipates potential risks. Think of it as the central communication hub for everyone involved in patient care – nurses, patients themselves, and the broader healthcare team. Effective care plans ensure that everyone is on the same page, working collaboratively towards the best possible patient outcomes. Without this structured planning, the consistency and quality of patient care can significantly suffer.
The process of nursing care planning is not static. It begins the moment a patient is admitted and continues to evolve throughout their care journey. Nurses constantly update and refine the care plan based on the patient’s changing condition and the ongoing evaluation of their progress. This commitment to individualized, patient-centered care is the bedrock of excellence in modern nursing practice.
Types of Nursing Care Plans: Formal vs. Informal, Standardized vs. Individualized
Nursing care plans aren’t one-size-fits-all. They can be broadly categorized as informal or formal, and further refined as standardized or individualized.
- Informal Nursing Care Plans: These are mental strategies, existing in the nurse’s mind as a quick approach to immediate patient needs. They are often used for routine tasks and immediate adjustments in care.
- Formal Nursing Care Plans: These are documented guides, either written or digital, that meticulously organize patient care information. Formal plans ensure comprehensive and consistent care, especially for complex patient needs.
Formal care plans further branch into two essential types:
-
Standardized Care Plans: These are pre-developed templates designed for groups of patients with common needs. They streamline care for routine conditions, ensuring consistent baseline care and efficient use of nursing time. However, they are not tailored to individual patient nuances. The sample care plans often found online serve as standardized templates, offering a starting point for more personalized plans.
-
Individualized Care Plans: These plans take standardization a step further by adapting them to the specific and unique needs of each patient. They incorporate approaches proven effective for a particular individual, leading to more personalized and holistic care. This tailored approach not only enhances patient outcomes but also significantly boosts patient satisfaction. When patients feel their care is specifically designed for them, they are more engaged and satisfied with their healthcare experience. In today’s healthcare landscape, where patient satisfaction is a key indicator of quality care, individualized care plans are paramount.
The Objectives and Purposes of Nursing Care Plans
Why are nursing care plans so critical? They serve several key objectives and purposes:
Objectives:
- Promote Evidence-Based Care: Care plans encourage the use of the latest research and best practices in nursing, ensuring patients receive the most effective treatments in a comfortable and familiar environment.
- Support Holistic Care: They facilitate a comprehensive approach to patient well-being, considering physical, psychological, social, and spiritual needs in disease management and prevention.
- Establish Structured Care Programs: Care plans are foundational for developing care pathways and bundles, which streamline team-based care and ensure adherence to best practices for specific conditions.
- Clearly Define Goals and Outcomes: They help nurses articulate specific, measurable goals and expected outcomes for patient care.
- Enhance Communication and Documentation: Care plans serve as vital communication tools, ensuring all members of the healthcare team are informed and care is accurately documented.
- Measure Nursing Care Effectiveness: They provide a framework for evaluating the quality and impact of nursing interventions.
Purposes:
- Defines the Nurse’s Role: Care plans highlight the unique and independent contributions of nurses in patient care, beyond simply following physician orders.
- Provides Direction for Individualized Care: They act as a personalized roadmap, guiding nurses to think critically and tailor interventions to each patient’s specific needs.
- Ensures Continuity of Care: Care plans enable consistent, high-quality care across different nursing shifts and departments, maximizing the benefits of treatment for patients.
- Coordinates Care Among Teams: They ensure all healthcare team members are aware of patient needs and the actions required, preventing gaps and overlaps in care.
- Serves as Legal Documentation: Care plans accurately document observations, nursing actions, and patient instructions, providing evidence of care provided and meeting legal and regulatory requirements.
- Guides Staff Assignment: They assist in matching patient needs with nursing staff skills, ensuring appropriate expertise is applied to each patient’s care.
- Monitors Patient Progress: Care plans facilitate tracking patient progress and making necessary adjustments to the plan as health status evolves.
- Supports Reimbursement: Insurance companies utilize care plan documentation to determine coverage and reimbursement for hospital care.
- Defines Patient Goals and Engagement: They empower patients by involving them in their treatment and care planning, fostering collaboration and adherence.
Essential Components of a Nursing Care Plan
A comprehensive nursing care plan typically incorporates several key components, each playing a vital role in guiding patient care:
- Nursing Diagnoses: These are clinical judgments about individual, family, or community experiences/responses to actual or potential health problems/life processes. They provide the foundation for the entire care plan. This is where nursing diagnosis books become invaluable, assisting nurses in accurately identifying and selecting the most appropriate diagnoses.
- Client Problems: A broader statement of the patient’s health issues, often encompassing medical diagnoses and patient concerns.
- Expected Outcomes: Specific, measurable, achievable, relevant, and time-bound (SMART) goals that define the desired changes in patient health status.
- Nursing Interventions: The specific actions nurses will take to achieve the expected outcomes. These interventions should be evidence-based and tailored to the patient’s needs and nursing diagnoses.
- Rationales: The scientific or evidence-based reasons behind each nursing intervention, explaining why the chosen action is expected to be effective.
- Evaluation: A continuous process of assessing the patient’s progress toward achieving the expected outcomes and the effectiveness of the care plan.
Navigating Care Plan Formats: 3-Column, 4-Column, and Student Plans
Nursing care plans can be structured in various formats, often categorized by the number of columns used to organize information. Common formats include three-column, four-column, and specialized student care plans.
-
Three-Column Format: This format typically includes columns for:
- Nursing Diagnosis: The identified nursing diagnosis.
- Outcomes and Evaluation: Desired patient outcomes and space for evaluating goal achievement.
- Interventions: Nursing actions to achieve the outcomes.
-
Four-Column Format: This expands on the three-column format by separating outcomes and evaluation into distinct columns:
- Nursing Diagnosis: The nursing diagnosis.
- Goals and Outcomes: Desired patient goals and specific, measurable outcomes.
- Interventions: Nursing actions.
- Evaluation: Assessment of goal achievement.
-
Student Care Plans: Designed for nursing students, these plans are more detailed and serve as learning tools. They often include an additional column for Rationales or Scientific Explanation to deepen understanding of the interventions. Student care plans are frequently handwritten to reinforce the learning process.
Step-by-Step Guide to Writing a Nursing Care Plan
Creating an effective nursing care plan involves a systematic, step-by-step approach. Here’s a breakdown of the process:
Step 1: Data Collection or Assessment:
This initial step is crucial. It involves building a comprehensive patient database using various assessment techniques. This includes:
- Physical Assessment: Hands-on examination of the patient’s physical condition.
- Health History: Gathering information about the patient’s past and present health status, including medical history, medications, allergies, and lifestyle factors.
- Interviews: Direct conversations with the patient and family to understand their perspectives, concerns, and needs.
- Medical Records Review: Examining existing medical documentation for relevant information.
- Diagnostic Studies: Analyzing results from laboratory tests, imaging, and other diagnostic procedures.
This thorough data collection allows nurses to identify relevant related factors, risk factors, and defining characteristics that will be used to formulate accurate nursing diagnoses. Critical thinking is paramount in this phase, integrating medical knowledge with patient-specific information to make informed clinical judgments.
Step 2: Data Analysis and Organization:
Once data is collected, the next step is to analyze, cluster, and organize it. This involves:
- Identifying Patterns: Looking for recurring themes and significant findings within the collected data.
- Clustering Data: Grouping related data points together to identify potential problem areas.
- Analyzing Data: Interpreting the clustered data to understand the patient’s health status and needs.
This organized data analysis forms the basis for formulating nursing diagnoses, setting priorities, and defining desired outcomes.
Step 3: Formulating Nursing Diagnoses:
Nursing diagnoses are standardized statements that identify a patient’s health problems that nurses can independently address. They are distinct from medical diagnoses, focusing on the patient’s response to illness or health conditions. Accurate nursing diagnoses are essential because they drive the entire care plan. This is where nursing diagnosis books become invaluable. They provide a comprehensive list of diagnoses, their defining characteristics, and related factors, assisting nurses in selecting the most appropriate diagnosis for each patient situation.
Step 4: Setting Priorities:
Prioritization involves ranking nursing diagnoses based on their urgency and importance to the patient’s well-being. This step ensures that the most critical needs are addressed first. Prioritization often utilizes Maslow’s Hierarchy of Needs, a framework that organizes human needs into a pyramid, with basic physiological needs at the base and higher-level needs at the top.
Maslow’s Hierarchy of Needs:
-
Physiological Needs (Highest Priority): These are fundamental for survival, including:
- ABC’s: Airway, Breathing, Circulation
- Nutrition (food and water)
- Elimination
- Sleep
- Shelter
- Exercise
- Sex
-
Safety and Security Needs: Focus on physical and emotional safety, including:
- Injury prevention (fall precautions, infection control)
- Security and stability
- Trust and safety
- Patient education on safety measures
-
Love and Belonging Needs: Social connection and intimacy:
- Supportive relationships
- Avoiding social isolation
- Therapeutic communication
- Intimacy
-
Self-Esteem Needs: Confidence and self-worth:
- Sense of achievement
- Acceptance and respect
- Independence and control
-
Self-Actualization Needs (Lowest Priority): Reaching one’s full potential:
- Personal growth
- Spiritual development
- Creativity and problem-solving
By considering Maslow’s Hierarchy, nurses can prioritize diagnoses effectively. Physiological and safety needs take precedence over psychosocial needs. Other factors influencing prioritization include patient values, beliefs, available resources, and the urgency of the situation. Patient involvement in this process is crucial to ensure their needs and preferences are considered.
Step 5: Establishing Client Goals and Desired Outcomes:
Once priorities are set, the nurse and patient collaborate to establish goals and desired outcomes for each nursing diagnosis. Goals describe the broad, overall aim of nursing care, while desired outcomes are specific, measurable changes expected in the patient’s health status. These outcomes serve as:
- Direction for Interventions: Guiding the selection of appropriate nursing actions.
- Evaluation Criteria: Providing benchmarks for measuring patient progress.
- Motivation for Patient and Nurse: Creating a sense of achievement as goals are met.
Goals and outcomes should be SMART:
-
Specific: Clearly defined and focused.
-
Measurable: Quantifiable and observable.
-
Attainable: Realistic and achievable for the patient.
-
Relevant: Meaningful and important to the patient’s needs.
-
Time-bound: With a defined timeframe for achievement.
Goals can be short-term (achievable within hours or days) or long-term (achievable over weeks or months). Most acute care settings focus on short-term goals, while long-term goals are more common in chronic care or home health settings. Discharge planning often involves setting long-term goals to ensure continued progress after hospitalization.
Desired outcome statements typically include four components:
- Subject: The patient (often implied).
- Verb: The action the patient will perform (e.g., “will demonstrate,” “will verbalize”).
- Conditions or Modifiers: Context for the behavior (e.g., “using proper technique,” “to the nurse”).
- Criterion of Desired Performance: The standard for acceptable performance (e.g., “correctly,” “independently”).
Step 6: Selecting Nursing Interventions:
Nursing interventions are the specific actions nurses will implement to help patients achieve their goals and desired outcomes. Interventions should be:
- Evidence-based: Supported by research and best practices.
- Patient-centered: Tailored to the patient’s individual needs and preferences.
- Realistic and Achievable: Feasible with available resources and time.
- Safe and Appropriate: Suitable for the patient’s age, health condition, and cultural values.
- Aligned with Other Therapies: Coordinated with other healthcare team members and treatment plans.
Nursing interventions can be:
-
Independent Interventions: Actions nurses can initiate based on their own judgment and expertise (e.g., patient education, emotional support, ongoing assessment).
-
Dependent Interventions: Actions requiring a physician’s order (e.g., medication administration, IV therapy, specific treatments).
-
Collaborative Interventions: Actions implemented in conjunction with other healthcare professionals (e.g., physical therapy, dietary consults, social work referrals).
Step 7: Providing Rationales:
Rationales are the scientific or evidence-based justifications for each nursing intervention. They explain why a particular intervention is expected to be effective in achieving the desired outcome. Rationales are particularly important for nursing students as they help connect nursing actions to underlying principles and deepen their understanding of care planning.
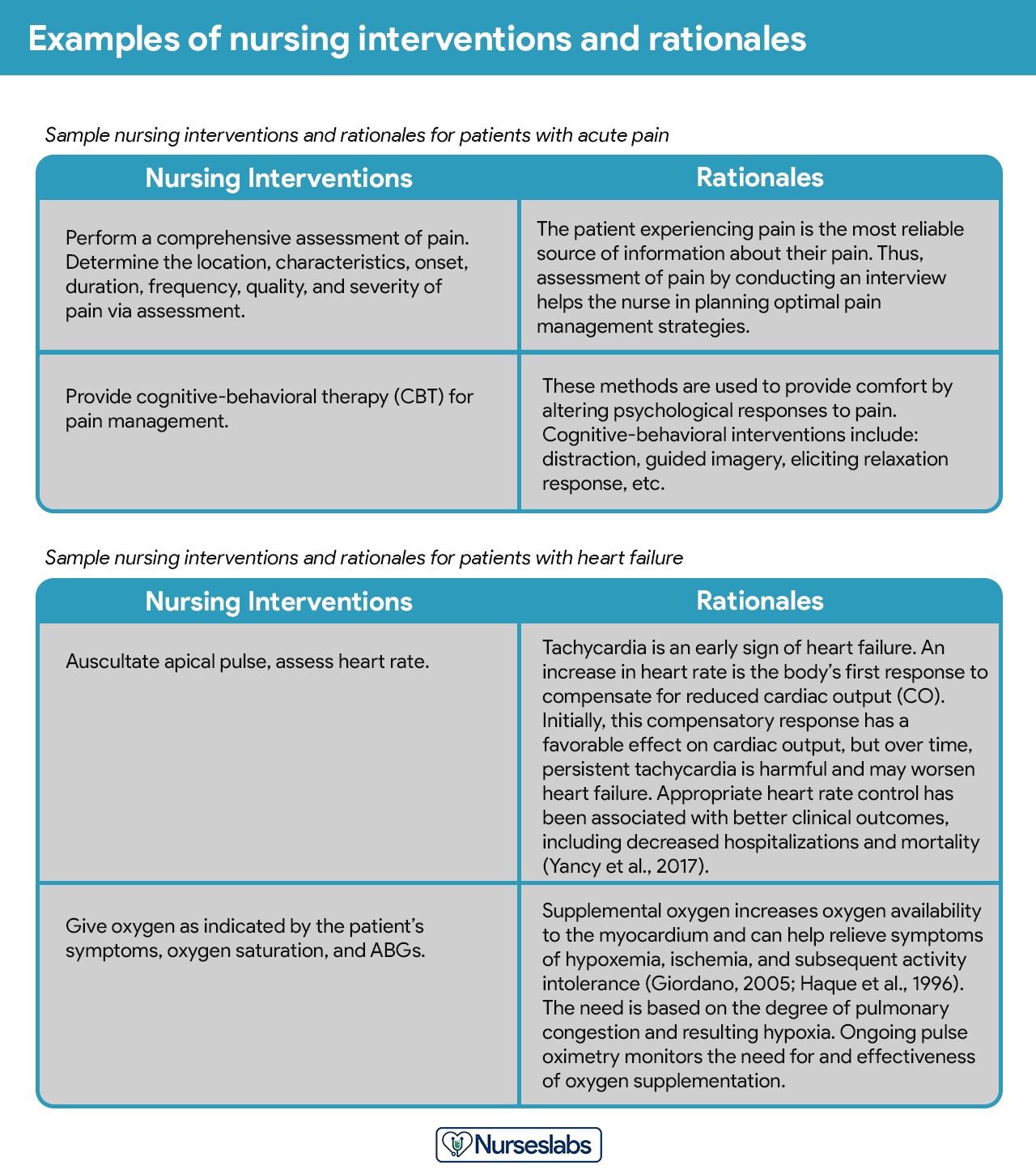{width=1280 height=1450}
*Image alt text: Example of nursing interventions with corresponding rationales in a care plan, demonstrating the link between nursing actions and their scientific basis.*Step 8: Evaluation:
Evaluation is an ongoing, systematic process of assessing the patient’s progress toward achieving goals and the effectiveness of the care plan. It involves:
- Collecting Data: Gathering information about the patient’s current status in relation to the desired outcomes.
- Comparing Data to Outcomes: Analyzing whether the patient is meeting, partially meeting, or not meeting the established outcomes.
- Drawing Conclusions: Determining the effectiveness of the care plan and identifying areas for improvement.
- Modifying the Care Plan: Adjusting diagnoses, outcomes, or interventions based on the evaluation findings.
Evaluation is a critical step in the nursing process, ensuring that care plans are dynamic and responsive to the patient’s evolving needs.
Step 9: Documentation:
The final step is to document the complete nursing care plan according to institutional policy. This documentation becomes part of the patient’s permanent medical record, ensuring continuity of care and providing a legal record of the care provided.
Leveraging Nursing Diagnosis Books for Enhanced Care Plans
Nursing diagnosis books are invaluable resources that significantly enhance the quality and effectiveness of nursing care plans. They offer a wealth of information to guide nurses through the crucial step of diagnosis selection and care planning.
Why are Nursing Diagnosis Books Essential?
- Comprehensive Lists of Diagnoses: These books provide exhaustive lists of NANDA-I (North American Nursing Diagnosis Association International) approved nursing diagnoses, ensuring nurses have access to the most current and standardized terminology.
- Defining Characteristics and Related Factors: For each diagnosis, these books detail the specific signs and symptoms (defining characteristics) and contributing factors (related factors) that help nurses accurately identify the most appropriate diagnosis for their patient.
- Guidance on Diagnosis Selection: They offer clear explanations and examples to help nurses differentiate between similar diagnoses and select the one that best reflects the patient’s specific situation.
- Support for Evidence-Based Care: Many books emphasize evidence-based interventions and rationales, promoting best practices in care planning.
- Time-Saving Resources: By providing readily accessible information, these books streamline the diagnosis and care planning process, saving nurses valuable time.
- Improved Accuracy and Confidence: Using these resources increases the accuracy of nursing diagnoses and boosts nurses’ confidence in their care planning abilities.
- Educational Value: For nursing students, these books are essential learning tools, helping them develop diagnostic reasoning and care planning skills.
Key Features to Look for in a Nursing Diagnosis Book:
- NANDA-I Alignment: Ensure the book is aligned with the latest NANDA-I diagnoses.
- Evidence-Based Content: Look for books that emphasize evidence-based interventions and rationales.
- Clear and Concise Language: The book should be easy to understand and navigate, with clear explanations and examples.
- Comprehensive Coverage: It should cover a wide range of diagnoses relevant to various clinical settings.
- Practical Application: Seek books that offer practical guidance on applying diagnoses to real-patient scenarios.
- User-Friendly Format: A well-organized format with indices, tables, and quick-reference tools enhances usability.
Recommended Nursing Diagnosis Books for Care Plan Excellence
Choosing the right nursing diagnosis book can significantly impact your ability to create effective care plans. Here are some highly recommended resources:
-
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: This handbook is lauded for its evidence-based approach and user-friendly three-step system. It guides you through assessment, diagnosis, and care planning with clear instructions and emphasizes diagnostic reasoning and critical thinking skills. Its strength lies in connecting evidence to practical interventions.
Image alt text: Cover image of “Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care,” highlighting its evidence-based approach. -
Nursing Care Plans – Nursing Diagnosis & Intervention: This comprehensive resource offers over 200 care plans reflecting the latest evidence-based guidelines. The newest edition includes ICNP diagnoses and expanded coverage of LGBTQ health and electrolyte/acid-base balance, making it exceptionally current and relevant.
Image alt text: Cover image of “Nursing Care Plans – Nursing Diagnosis & Intervention,” emphasizing its extensive care plans and up-to-date guidelines. -
Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: This quick-reference tool is ideal for on-the-go use. It provides essential information for identifying diagnoses and planning care efficiently. The latest edition features updated diagnoses and interventions, covering over 400 disorders in an alphabetized format for rapid access.
Image alt text: Cover image of “Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales,” showcasing its quick-reference format and comprehensive coverage. -
Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: This manual is distinguished by its detailed guidance on planning, individualizing, and documenting care for over 800 conditions. It uniquely offers subjective and objective data examples, clinical applications, prioritized interventions with rationales, and documentation sections for each diagnosis, making it an exceptionally thorough resource.
Image alt text: Cover image of “Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care,” emphasizing its focus on planning, individualization, and documentation. -
All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health: For a holistic approach, this e-book provides over 100 care plans spanning medical-surgical, maternity, pediatrics, and psychiatric-mental health nursing. Its “patient problems” focus promotes interprofessional communication and patient-centered language.
Image alt text: Cover image of “All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health,” highlighting its comprehensive coverage across nursing specialties.
Conclusion: Empowering Care Plans with the Right Resources
Mastering nursing care planning is a journey, and nursing diagnosis books are invaluable companions on this path. They provide the knowledge, structure, and confidence needed to create patient-centered, effective care plans. By utilizing these resources, nurses can enhance their diagnostic accuracy, select appropriate interventions, and ultimately, deliver superior patient care. Investing in a quality nursing diagnosis book is an investment in your nursing expertise and your patients’ well-being. Embrace these resources and elevate your care planning skills to new heights.
