Cushing’s syndrome, also known as hypercortisolism or adrenal hyperfunction, is an endocrine disorder characterized by an excess of adrenocortical hormones, particularly cortisol. This excess can also involve related corticosteroids, and to a lesser extent, androgens and aldosterone. This condition leads to a constellation of clinical abnormalities affecting various body systems.
Understanding Cushing’s Syndrome
Cushing’s syndrome disrupts the body’s hormonal balance, leading to a range of symptoms. It’s crucial to understand the underlying causes and manifestations of this condition to provide effective nursing care.
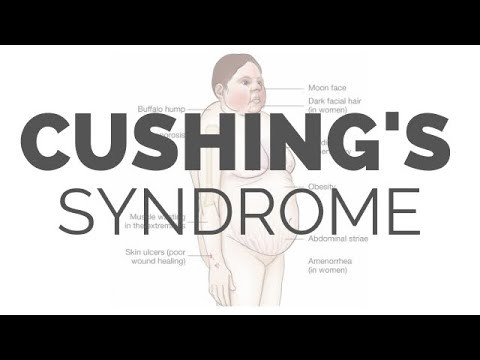 YouTube video about Cushing's syndrome
YouTube video about Cushing's syndrome
Prevalence of Cushing’s Syndrome
Cushing’s syndrome is a relatively common endocrine disorder worldwide, affecting approximately 13 out of every 1 million people. It is notably more prevalent in women than in men, with primary occurrence observed between the ages of 25 and 40.
Root Causes of Cushing’s Syndrome
The etiology of Cushing’s syndrome is diverse, stemming from several potential factors:
- Excessive Corticotropin Production: In about 70% of cases, Cushing’s syndrome is triggered by the overproduction of corticotropin. This hormone imbalance leads to adrenal cortex hyperplasia, subsequently causing excessive cortisol secretion.
- Adrenal Tumors: The remaining 30% of cases are often associated with cortisol-secreting adrenal tumors. These tumors are typically benign but are responsible for autonomous cortisol production, disrupting the normal feedback mechanisms of the endocrine system.
Clinical Signs and Symptoms of Cushing’s Syndrome
Cushing’s syndrome manifests through a variety of clinical signs and symptoms, impacting multiple organ systems due to hormonal dysregulation.
- Muscle Weakness: Patients frequently experience muscle weakness, which can arise from hypokalemia or muscle mass loss due to increased protein catabolism. This weakness can significantly impact mobility and daily activities.
- Buffalo Hump: A characteristic sign is the development of fat pads over the upper back and neck, known as a buffalo hump. This is due to the altered fat distribution associated with Cushing’s syndrome.
- Moon Face: Another hallmark symptom is a rounded, full face, often referred to as moon face. This is caused by the deposition of excess fat in the facial area.
- Truncal Obesity: Central or truncal obesity, characterized by fat accumulation around the abdomen and trunk, while limbs remain relatively slender, is a common feature.
- Peptic Ulcer Disease: The risk of peptic ulcers increases due to elevated gastric acid production, increased pepsin secretion, and a reduction in protective gastric mucus.
- Psychological Disturbances: Emotional and psychological changes are common, ranging from irritability and emotional lability to euphoria, depression, and even psychosis.
- Hypertension: Elevated blood pressure is frequently observed in Cushing’s syndrome patients due to sodium and water retention, driven by hormonal imbalances.
- Compromised Immunity: The immune system can be significantly weakened, increasing susceptibility to infections. This is due to decreased lymphocyte production and suppressed antibody formation.
Potential Complications of Cushing’s Syndrome
Untreated or poorly managed Cushing’s syndrome can lead to several serious complications, further impacting patient health and quality of life.
Diagnostic Evaluation for Cushing’s Syndrome
Diagnosing Cushing’s syndrome involves a comprehensive evaluation, utilizing various assessments and diagnostic findings to confirm the condition and identify its cause.
Medical Interventions for Cushing’s Syndrome
The primary goal of medical management is to restore hormonal balance and alleviate the symptoms of Cushing’s syndrome. Treatment strategies may include radiation therapy, drug therapy, or surgical intervention, depending on the etiology and severity of the condition.
Pharmacological Approaches
Pharmacologic therapy plays a crucial role in managing Cushing’s syndrome, particularly in cases where surgery is not immediately feasible or as an adjunct to other treatments.
Surgical Options for Cushing’s Syndrome
Surgical intervention often provides the most effective and definitive treatment for Cushing’s syndrome, especially when caused by tumors.
- Transsphenoidal Hypophysectomy: For Cushing’s syndrome resulting from pituitary tumors, transsphenoidal hypophysectomy is the preferred surgical approach. This procedure involves the selective removal of the pituitary tumor and boasts an 80% success rate in resolving the condition.
- Adrenalectomy: In cases of primary adrenal hypertrophy or adrenal tumors, adrenalectomy, the surgical removal of one or both adrenal glands, is often the treatment of choice.
Nursing Management and Care for Cushing’s Syndrome
Nursing care is paramount in managing patients with Cushing’s syndrome. Nurses play a vital role in monitoring patients, preventing complications, and providing supportive care throughout the treatment process.
Comprehensive Nursing Assessment
A thorough nursing assessment is essential to understand the patient’s condition and tailor care effectively.
- Detailed Health History: Gathering a comprehensive health history includes assessing the patient’s activity level and their capacity to perform routine daily and self-care activities.
- Thorough Physical Examination: Physical examination focuses on skin assessment for trauma, infection, breakdown, bruising, and edema. Monitoring these skin changes is crucial due to the skin fragility associated with Cushing’s syndrome.
- Mental Status Evaluation: Assessing mental function is critical, evaluating mood, responses to questions, environmental awareness, and signs of depression or other psychological disturbances.
Key Nursing Diagnoses for Cushing’s Syndrome
Based on thorough assessment data, several nursing diagnoses are pertinent for patients with Cushing’s syndrome. These diagnoses guide the development of individualized care plans to address the specific needs of each patient. Identifying the correct nursing diagnosis is crucial for effective care planning. Common nursing diagnoses include:
- Risk for Injury: Related to muscle weakness, osteoporosis, and altered balance.
- Risk for Infection: Related to immunosuppression secondary to excess cortisol.
- Self-Care Deficit: Related to fatigue, muscle weakness, and altered body image.
- Impaired Skin Integrity: Related to fragile skin, edema, and poor wound healing.
- Disturbed Body Image: Related to physical changes such as moon face, buffalo hump, and truncal obesity.
- Disturbed Thought Processes: Related to hormonal imbalances affecting mental and emotional stability.
Nursing Care Planning and Goals
The overarching nursing goals for patients with Cushing’s syndrome are centered on mitigating risks and improving patient well-being. These goals include:
- Minimizing the risk of injury through preventive measures and a safe environment.
- Reducing the risk of infection by implementing infection control practices and early detection.
- Enhancing the patient’s ability to perform self-care activities by providing support and adaptive strategies.
- Promoting skin integrity through meticulous skin care and preventive measures.
- Improving body image by addressing psychological and emotional aspects and fostering positive self-perception.
- Optimizing mental function by providing emotional support and managing psychological symptoms.
Essential Nursing Interventions
Nursing interventions for Cushing’s syndrome are multifaceted, aiming to address the specific nursing diagnoses and achieve the established patient goals.
Reducing Risk of Injury
- Implement a safe environment to prevent falls, fractures, and soft tissue injuries.
- Provide assistance with ambulation for weak patients to prevent falls and collisions.
- Recommend a diet rich in protein, calcium, and vitamin D to combat muscle wasting and osteoporosis. Dietary consultation with a dietitian is beneficial.
Minimizing Risk of Infection
- Limit exposure to individuals with infections to protect the immunocompromised patient.
- Conduct frequent assessments for subtle signs of infection, as corticosteroids can mask typical inflammatory responses and infection indicators.
Preoperative Nursing Care
Promoting Rest and Activity
Maintaining Skin Integrity
- Employ meticulous skin care techniques to prevent trauma to fragile skin.
- Avoid adhesive tape, which can cause skin tears and irritation.
- Regularly assess skin and bony prominences for signs of breakdown.
- Encourage frequent position changes to relieve pressure and promote circulation.
Enhancing Body Image
- Facilitate discussions about the impact of physical changes on self-concept and interpersonal relationships. Reassure patients that physical changes are often reversible with successful treatment.
- Recommend dietary modifications, such as a low-carbohydrate, low-sodium, and high-protein diet, to manage weight gain and edema and alleviate bothersome symptoms.
Improving Thought Processes
- Educate the patient and family about the emotional instability associated with Cushing’s syndrome. Provide coping strategies for mood swings, irritability, and depression.
- Report any instances of psychotic behavior for prompt intervention.
- Encourage verbalization of feelings and concerns from both the patient and family members to foster emotional support and coping.
Monitoring and Managing Complications
- Adrenal Hypofunction and Addisonian Crisis: Vigilantly monitor for signs of adrenal hypofunction and Addisonian crisis, including hypotension, rapid weak pulse, rapid respiratory rate, pallor, and extreme weakness. Identify potential precipitating factors like stress, trauma, or surgery.
- Administer IV fluids, electrolytes, and corticosteroids as prescribed, especially before, during, and after surgery or treatments, to support adrenal function.
- Monitor for and promptly treat circulatory collapse and shock, which can occur during Addisonian crisis.
- Assess fluid and electrolyte balance through laboratory values and daily weight monitoring.
- Monitor blood glucose levels and report any elevations to the physician, as hyperglycemia is a potential complication.
Patient Education for Self-Care
- Provide comprehensive information about Cushing’s syndrome both verbally and in written format for the patient and family.
- Emphasize the critical importance of not abruptly stopping corticosteroid use without medical supervision, as this can lead to adrenal insufficiency and symptom recurrence.
- Stress the need to maintain an adequate supply of prescribed corticosteroids to prevent missed doses and potential Addisonian crisis.
- Educate on necessary dietary modifications to ensure adequate calcium intake while managing risks of hypertension, hyperglycemia, and weight gain.
- Instruct the patient and family on how to monitor blood pressure, blood glucose levels, and weight at home.
- Recommend wearing a medical alert bracelet and informing all healthcare professionals about the Cushing’s syndrome diagnosis.
- Arrange for home care services as needed to ensure a safe, low-stress environment and minimize fall risks and other side effects.
- Emphasize the importance of regular medical follow-up appointments and ensure the patient understands potential medication side effects and toxicities.
Evaluation of Nursing Care
Expected patient outcomes indicating effective nursing care include:
- Reduced incidence of injuries.
- Decreased occurrence of infections.
- Improved ability to perform self-care activities.
- Enhanced skin integrity.
- Improved body image and self-perception.
- Stabilized mental function.
Discharge Planning and Home Care Guidelines
Prior to discharge, it is crucial to educate the patient and family about the importance of adhering to discharge orders to prevent adrenal insufficiency and symptom recurrence.
Documentation in Nursing Care
Accurate and thorough documentation is essential and should include:
- The patient’s and caregiver’s understanding of individual risks and safety precautions.
- Available and utilized resources and support systems.
- Recent or ongoing antibiotic therapy.
- Signs and symptoms of any infectious processes.
- Functional level and specific limitations.
- Needed resources and adaptive equipment.
- The plan of care and individuals involved in planning.
- Patient education plan and content.
- Individual responses to nursing interventions, teaching, and actions taken.
- Specific actions and any changes made to the care plan.
- Progress towards achieving desired patient outcomes.
- Modifications to the plan of care as needed.
Further Reading
Related resources for additional information on Cushing’s syndrome.