Peripheral arterial disease (PAD), often referred to as peripheral vascular disease (PVD), is a common circulatory problem in which narrowed arteries reduce blood flow to the limbs. This condition is typically a manifestation of atherosclerosis, where plaque buildup narrows the arteries, most commonly affecting the legs and feet. Untreated PAD can lead to serious complications, including gangrene, amputation, and increased risk of cardiovascular events like heart attack and stroke.
For nurses, understanding and managing PAD is crucial. This article provides an in-depth guide to nursing diagnoses related to peripheral arterial disease, enhancing the original content with a focus on comprehensive care and SEO optimization for healthcare professionals and nursing students.
Nursing Process in Peripheral Arterial Disease Management
The cornerstone of managing PAD lies in a holistic nursing approach. The primary goal is to mitigate cardiovascular risks and address the chronic condition affecting blood vessels. Nurses play a pivotal role in patient education, promoting lifestyle modifications, and ensuring adherence to prescribed therapies.
When conservative measures are insufficient, revascularization procedures such as angioplasty or bypass grafting may be necessary. Nursing care extends to pre- and post-operative management, aiming to prevent complications and facilitate optimal recovery.
Comprehensive Nursing Assessment for PAD
The initial step in nursing care is a thorough assessment, encompassing physical, psychosocial, emotional, and diagnostic data. This section elaborates on subjective and objective data collection relevant to PAD.
Review of Health History: Subjective Data
1. Elicit General and Specific Symptoms:
Patients with PAD may present with a variety of symptoms. Key symptoms to inquire about include:
- General Symptoms:
- Pain aggravated by activity: Characteristically, PAD pain worsens with exertion and improves with rest.
- Cardiovascular Symptoms:
- Weak or absent peripheral pulses: Patients may report noticing changes in their pulse strength in the extremities.
- Integumentary Symptoms:
- Skin color changes: Inquire about pallor (paleness), cyanosis (bluish discoloration), or erythema (redness) in the extremities.
- Temperature changes: Patients may perceive decreased skin temperature in affected limbs.
- Skin texture changes: Ask about thin, taut, or shiny skin, particularly on the lower legs and feet.
- Non-healing wounds or ulcers: A critical symptom indicative of poor circulation.
- Hair loss on legs: Patients may notice thinning or absence of hair on their legs.
- Nail changes: Thickened or opaque toenails can be a sign.
- Musculoskeletal Symptoms:
- Reduced mobility and weakness: PAD can limit physical activity due to pain and discomfort.
- Muscle heaviness or fatigue: Leg muscles may feel heavy or easily fatigued.
- Paresthesia: Numbness or tingling sensations in the legs or feet.
- Intermittent Claudication: Muscle pain during activity that is relieved by rest, a hallmark symptom of PAD.
- Reproductive Symptoms:
- Impotence (in men): PAD can affect blood flow and contribute to erectile dysfunction.
2. Detailed Medical History Review:
Atherosclerosis is the primary underlying cause of PAD. Explore the patient’s medical history for conditions that contribute to plaque formation:
- Hypertension: High blood pressure damages blood vessels.
- Hyperlipidemia: High cholesterol levels contribute to plaque buildup.
- Diabetes Mellitus: Diabetes significantly accelerates atherosclerosis.
- Coronary Artery Disease (CAD): PAD often coexists with CAD as both are manifestations of systemic atherosclerosis.
- Cerebrovascular Disease: History of stroke or transient ischemic attack (TIA) is relevant.
- Renal Insufficiency: Kidney disease is linked to vascular disease.
3. Family History Assessment:
Genetic predisposition plays a role in PAD. Inquire about:
- Family history of PAD, especially in first-degree relatives diagnosed before age 65.
- History of heart disease or stroke in the family.
4. Risk Factor Identification:
Identify modifiable and non-modifiable risk factors for PAD:
- Smoking: A major and modifiable risk factor.
- Sedentary Lifestyle: Lack of physical activity contributes to PAD.
- Age: Risk increases with older age.
- Gender: Men are generally at higher risk, although risk increases in women post-menopause.
- Obesity: Excess weight contributes to several PAD risk factors.
- Ethnicity: African Americans have a higher prevalence of PAD.
5. Dietary History:
Diet significantly impacts atherosclerosis. Assess for consumption of:
- Saturated Fats: Found in fatty meats and dairy products.
- Simple Carbohydrates: High sugar intake can contribute to diabetes and dyslipidemia.
- High Sodium Foods: Excess sodium can elevate blood pressure.
Physical Assessment: Objective Data
1. Assess the 5 P’s of Acute Arterial Occlusion:
These classic signs indicate acute limb ischemia and require immediate attention:
- Pulselessness: Absence of palpable pulses distal to the blockage.
- Pallor: Pale appearance of the limb.
- Pain: Severe, sudden onset of pain.
- Paresthesia: Numbness and tingling.
- Paralysis: Loss of motor function.
Note: Paresthesia and paralysis are late signs indicating severe ischemia and potential limb loss, necessitating urgent intervention.
2. Cardiovascular Status Examination:
- Auscultate Heart Sounds: Listen for murmurs or irregularities.
- Peripheral Pulse Palpation: Assess pulse quality (strength, rhythm) in all peripheral arteries (e.g., femoral, popliteal, dorsalis pedis, posterior tibial, radial, ulnar). Document pulse strength using a scale (e.g., 0-4+).
- Auscultate for Bruits: Listen for abnormal swishing sounds (bruits) over major arteries (femoral, carotid, abdominal aorta), indicating turbulent blood flow due to narrowing.
3. Allen Test:
- Perform the Allen test to evaluate collateral circulation to the hands, especially important before radial artery procedures. A negative Allen test (delayed color return) suggests insufficient collateral flow.
4. Skin Assessment:
Observe for skin changes indicative of PAD:
- Alopecia: Hair loss on the lower extremities.
- Skin Texture: Dry, scaly, or erythematous (reddened) skin.
- Pigmentation Changes: Persistent discoloration.
- Nail Changes: Brittle or thickened nails.
5. Advanced PAD Signs:
Recognize signs of critical limb ischemia, indicating advanced disease:
- Rest Pain: Pain in the foot or lower leg at rest, often worsening at night.
- Non-healing Ulcers or Gangrene: Tissue necrosis due to severe ischemia.
- Cyanosis or Mottling (Livedo Reticularis): Bluish discoloration or a “fishnet” pattern on the skin.
- Cold Extremities: Palpable coolness compared to proximal areas.
- Pulselessness: Often absent pulses.
6. Pain Assessment:
- Characterize pain: Differentiate between intermittent claudication (activity-related pain relieved by rest) and rest pain (pain at rest, indicating severe ischemia).
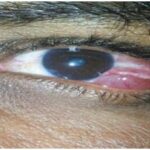
Image: Visual representation of common Peripheral Artery Disease (PAD) symptoms, emphasizing leg and foot issues.
Diagnostic Procedures for PAD
1. Blood Tests:
Routine blood tests help assess overall health and risk factors:
- Complete Blood Count (CBC): Evaluates general health and can identify anemia, which can worsen PAD symptoms.
- Blood Urea Nitrogen (BUN) and Creatinine: Assess kidney function, as renal insufficiency is associated with vascular disease.
- Electrolyte Levels: To evaluate for imbalances.
- Coagulation Tests (PT/INR, aPTT): Baseline before anticoagulation therapy.
- Lipid Profile (Cholesterol, Triglycerides, LDL, HDL): Assess for hyperlipidemia, a major risk factor.
2. Inflammatory Markers:
Elevated inflammatory markers may be associated with exercise intolerance in PAD:
- D-dimer: Can be elevated but is not specific to PAD.
- C-reactive Protein (CRP): General marker of inflammation.
- Interleukin-6 (IL-6): Pro-inflammatory cytokine.
- Homocysteine: Elevated levels are linked to vascular disease.
3. Ankle-Brachial Index (ABI):
- A key non-invasive test comparing blood pressure in the ankles to the arms. A normal ABI is 1.0-1.4. An ABI of 0.9 or less is diagnostic of PAD. Severe PAD is indicated by ABI <0.5.
4. Doppler Ultrasound:
- Non-invasive assessment of blood flow. Absent or diminished Doppler signals indicate blockage or reduced flow. Duplex ultrasound combines Doppler with B-mode imaging to visualize arteries and blood flow.
5. Transcutaneous Oximetry (TcPO2):
- Measures oxygen tension in the skin, useful in assessing tissue perfusion, particularly in diabetic patients and wound care. Low TcPO2 levels indicate poor perfusion.
6. Imaging Scans:
Advanced imaging techniques provide detailed visualization of blood vessels:
- Magnetic Resonance Imaging (MRI): High detail for plaque visualization but can be costly and time-consuming.
- Computed Tomography (CT) with Contrast: Effective for visualizing arterial stenosis and occlusions.
- CT Angiography (CTA): Rapid, non-invasive, and provides excellent anatomical detail of arteries.
- Magnetic Resonance Angiography (MRA): Highly accurate without radiation, but also costly and may not be readily available.
Nursing Interventions for Peripheral Arterial Disease
Nursing interventions are aimed at slowing disease progression, managing symptoms, and preventing complications.
1. Lifestyle Modification and Risk Factor Management:
- Smoking Cessation: Essential for preventing disease progression. Provide resources and support for quitting.
- Exercise Therapy: Supervised exercise programs, particularly walking, are highly effective for improving claudication symptoms.
- Weight Management: Achieving and maintaining a healthy weight reduces cardiovascular risk.
- Heart-Healthy Diet: Low in saturated fat, cholesterol, and sodium; rich in fruits, vegetables, and whole grains.
2. Pharmacological Management:
Administer medications as prescribed, which may include:
- Statins: To lower LDL cholesterol and reduce plaque buildup.
- Antihypertensives: To manage blood pressure, typically aiming for <130/80 mmHg for patients with diabetes and <120/80 mmHg for non-diabetics.
- Antidiabetic Agents: To maintain optimal blood glucose control (HbA1c <7% in diabetics).
- Antiplatelet Medications (e.g., Aspirin, Clopidogrel): To reduce the risk of blood clot formation.
- Anticoagulants (e.g., Warfarin, Heparin): For specific indications, such as acute thrombotic events.
- Cilostazol: A phosphodiesterase inhibitor that acts as a vasodilator and antiplatelet agent, specifically indicated to improve walking distance in claudication.
3. Revascularization Procedures:
Prepare patients for procedures when indicated:
- Angioplasty and Stenting: Minimally invasive procedures to open blocked arteries.
- Bypass Grafting: Surgical procedure to reroute blood flow around blocked arteries.
- Atherectomy: Procedure to remove plaque from arteries.
4. Management of Acute Thrombosis/Embolism:
- If acute limb ischemia due to thrombus or embolus occurs, immediate anticoagulation with heparin infusion is necessary.
5. Patient Education:
- Emphasize the importance of lifestyle modifications, medication adherence, and foot care.
- Advise patients to avoid decongestants containing pseudoephedrine, as they can worsen PAD symptoms by constricting blood vessels.
- Refer patients to a nutritionist for dietary guidance and to physical therapy for exercise programs.
6. Foot Care Education:
- Crucial for preventing ulcers and infections, especially in diabetic patients.
- Instruct on daily foot inspection, proper footwear, avoiding injury, and prompt care for any foot lesions.
Nursing Care Plans and Diagnoses for Peripheral Arterial Disease
Based on assessment findings, several nursing diagnoses are pertinent to PAD. Here are examples of common nursing diagnoses, related factors, and expected outcomes:
1. Acute Pain
Nursing Diagnosis: Acute Pain related to vascular system blockage secondary to peripheral vascular disease.
As evidenced by:
- Verbal reports of pain, cramping, or aching in extremities during walking.
- Reports of burning pain in feet (severe cases).
- Muscle fatigue.
- Reluctance to engage in physical activity.
Expected Outcomes:
- Patient will report reduced pain levels during activity.
- Patient will increase participation in physical activity without significant pain.
Nursing Interventions:
- Pain Assessment: Thoroughly assess pain characteristics (location, intensity, quality, aggravating/relieving factors).
- Medication Administration: Administer prescribed analgesics and vasodilators (e.g., cilostazol) as ordered.
- Exercise Promotion: Encourage a structured walking program (walk-rest-walk) to improve collateral circulation.
- Lifestyle Education: Reinforce the importance of weight management, smoking cessation, and managing comorbidities.
- Avoid Massage of Affected Extremities: Contraindicated if there’s a risk of dislodging emboli; consult physician.
2. Chronic Pain
Nursing Diagnosis: Chronic Pain related to limb ischemia secondary to plaque buildup in blood vessels (atherosclerosis).
As evidenced by:
- Reports of burning pain, paresthesias, intermittent claudication.
- Altered mobility due to pain.
Expected Outcomes:
- Patient will report decreased burning, tingling, and numbness.
- Patient will utilize non-pharmacological pain management techniques.
Nursing Interventions:
- Pain Assessment: Assess pain characteristics, including presence of rest pain and signs of critical limb ischemia (rest pain, non-healing ulcers, ABI <0.4).
- Exercise Therapy: Collaborate with physical therapy to develop a tailored exercise program.
- Non-pharmacological Pain Management: Explore techniques like biofeedback, mirror therapy, imagery, and meditation.
- Spinal Cord Stimulation: Consider for severe ischemic pain unresponsive to other analgesics (requires physician referral).
- Psychological Support: Address the emotional impact of chronic pain; refer to mental health services if needed.
- Prepare for Revascularization: If indicated, prepare patient for surgical or endovascular interventions.
3. Ineffective Peripheral Tissue Perfusion
Nursing Diagnosis: Ineffective Peripheral Tissue Perfusion related to atherosclerotic plaque buildup and reduced blood flow.
As evidenced by:
- Absent or weak peripheral pulses.
- Cool, cyanotic skin; shiny, hairless legs.
- Decreased blood pressure in affected extremities.
- Delayed wound healing.
- Extremity pain, intermittent claudication, paresthesia.
- Pallor with limb elevation.
Expected Outcomes:
- Patient will demonstrate adequate peripheral tissue perfusion, evidenced by palpable peripheral pulses (3+).
- Patient will verbalize understanding of medication regimen and lifestyle modifications to improve perfusion.
Nursing Interventions:
- Peripheral Pulse Assessment: Regularly assess and document peripheral pulses.
- Ankle-Brachial Index (ABI) Monitoring: Monitor ABI as an indicator of perfusion status.
- Chronic Condition Management: Ensure optimal management of diabetes, hypertension, and hyperlipidemia.
- Promote Ambulation: Encourage regular walking and advise against prolonged sitting.
- Statin Therapy: Advocate for statin use as per physician orders to manage atherosclerosis.
- Prepare for Surgical Intervention: If indicated, prepare patient for revascularization procedures.
4. Risk for Injury
Nursing Diagnosis: Risk for Injury related to tissue hypoxia, altered peripheral sensation, and decreased lower extremity strength secondary to PAD.
As evidenced by: (Risk diagnosis – evidenced by risk factors, not symptoms)
- Presence of PAD.
- Altered sensation in extremities.
- Potential for falls due to weakness and impaired balance.
Expected Outcomes:
- Patient will remain free from injury.
- Patient will demonstrate strategies to prevent falls and foot injuries.
Nursing Interventions:
- Environmental and Self-Care Assessment: Assess home environment for safety hazards, evaluate self-care abilities and need for support.
- Mobility Assessment: Assess gait, balance, and lower extremity strength to identify fall risks.
- Fall Prevention: Provide assistive devices (cane, walker), educate on safe ambulation techniques.
- Foot Care Education: Emphasize proper footwear, daily foot inspection, and preventative foot care measures.
- Smoking Cessation Support: Reinforce smoking cessation to reduce amputation risk.
- Physical/Occupational Therapy Referral: Refer for comprehensive mobility and safety assessment and interventions.
5. Risk for Peripheral Neurovascular Dysfunction
Nursing Diagnosis: Risk for Peripheral Neurovascular Dysfunction related to plaque buildup and reduced blood flow to extremities.
As evidenced by: (Risk diagnosis – evidenced by risk factors, not symptoms)
- Presence of PAD.
- Sedentary lifestyle.
- Atherosclerosis.
Expected Outcomes:
- Patient will maintain adequate peripheral neurovascular function, evidenced by palpable peripheral pulses and absence of pallor.
- Patient will not report paresthesia or numbness.
Nursing Interventions:
- Neurovascular Assessment: Regularly assess peripheral pulses, skin color and temperature, capillary refill, sensation, and motor function, comparing bilaterally.
- Balance and Gait Assessment: Evaluate balance and gait stability.
- Monitor for 5 P’s: Vigilantly monitor for signs of acute limb ischemia (pain, pallor, pulselessness, paresthesia, paralysis).
- Positioning Education: Advise against leg crossing; recommend leg elevation (but not above heart level).
- Medication Adherence: Ensure patient understanding and adherence to prescribed medications (antihypertensives, statins, antiplatelets).
- Supervised Exercise Program: Encourage participation in a structured exercise program to improve circulation.
- Patient Education on Neurovascular Dysfunction Signs: Educate on signs and symptoms requiring immediate medical attention (burning pain, numbness, diminished pulses, color changes, cold skin, prolonged capillary refill, decreased sensation/motor function).
- Clinical Photography (with consent): Consider documenting skin changes, hair loss, nail abnormalities with clinical images to monitor disease progression.
Image: Infographic outlining key risk factors associated with Peripheral Artery Disease (PAD), including smoking, diabetes, and hypertension.
References
(Implicitly referencing the information from the original article and general nursing knowledge related to Peripheral Arterial Disease.)