Understanding Fall Risk in Pediatric Patients
Falls are a significant concern across all age groups, but they present unique challenges and considerations in pediatric care. A fall is defined by the World Health Organization (WHO) as an event where an individual unintentionally comes to rest on the ground, floor, or another lower level. In children, falls are a leading cause of non-fatal injuries, ranging from minor bruises to severe fractures and traumatic brain injuries. While older adults are often highlighted in fall prevention discussions, children, especially infants and toddlers, are also highly vulnerable due to their rapid development, curiosity, and limited understanding of danger.
According to the Centers for Disease Control and Prevention (CDC), falls are a leading cause of injury in children. For infants, falls from changing tables, beds, or stairs are common. As children become mobile, environmental hazards in homes and playgrounds contribute to fall risks. Unlike falls in older adults, which often result from chronic conditions or age-related decline, pediatric falls are frequently associated with developmental stages, environmental factors, and inadequate supervision. Understanding these unique aspects is crucial for developing effective nursing diagnoses and pediatric care plans to mitigate the risk of falling in this vulnerable population.
Nurses are at the forefront of pediatric fall prevention. Their role encompasses comprehensive assessment, parent and child education, creating safe environments, and implementing targeted interventions. By recognizing the specific risk factors and developmental stages of children, nurses can significantly reduce the incidence of falls and associated injuries, promoting safer and healthier childhoods.
Factors Contributing to Pediatric Falls
Identifying the risk factors for falls in children is the first step in developing effective prevention strategies. These factors are diverse and often age-dependent:
-
Infants and Toddlers (Under 2 Years): This age group is particularly vulnerable due to rapid motor development coupled with a lack of awareness of danger.
- Developmental Milestones: Learning to roll over, sit, crawl, and walk inherently increases the risk of falls.
- Inadequate Supervision: Leaving infants unattended on elevated surfaces like changing tables, beds, or sofas.
- Environmental Hazards at Home: Stairs without gates, unsecured windows, unstable furniture, and cluttered floors.
- Use of Walkers and Jumpers: These devices can lead to falls down stairs or tip over easily.
-
Preschool and School-Age Children (2-10 Years): As children become more independent and adventurous, new risk factors emerge.
- Increased Physical Activity: Running, climbing, and playing sports increase exposure to fall hazards.
- Playground Equipment: Falls from swings, slides, and climbing structures are common.
- Environmental Hazards Outdoors: Uneven surfaces, playground surfaces, traffic.
- Lack of Safety Education: Insufficient understanding of safe play practices and environmental dangers.
- Certain Medical Conditions: Conditions affecting balance, coordination, or muscle strength can increase fall risk.
-
Adolescents (10-18 Years): While older children and adolescents are generally less prone to falls than younger children, risks still exist.
- Sports and Recreational Activities: Skateboarding, cycling, and team sports can lead to falls and injuries.
- Risk-Taking Behaviors: Adolescents may engage in activities that increase fall risk, such as climbing or unsafe stunts.
- Fatigue and Dehydration: These can impair balance and coordination, especially during physical activity.
- Underlying Medical Conditions: Neurological or musculoskeletal conditions impacting mobility.
-
General Risk Factors Across Pediatric Age Groups:
- Environmental Hazards: Clutter, slippery floors, inadequate lighting, loose rugs, and unstable furniture are hazards for all ages.
- Footwear: Ill-fitting or inappropriate footwear can contribute to trips and falls.
- Medications: Although less common in children than adults, certain medications can cause drowsiness or dizziness, increasing fall risk.
- Cognitive Impairment or Developmental Delays: Children with cognitive or developmental delays may have an increased risk of falls due to impaired judgment or motor skills.
- Sensory Deficits: Vision or hearing impairments can limit a child’s ability to perceive and avoid hazards.
Nursing Diagnosis for Risk of Falling in Pediatric Care
Formulating a nursing diagnosis is a critical step in developing a pediatric care plan focused on fall prevention. For children at risk of falls, the primary nursing diagnosis is typically:
Risk for Falls as evidenced by [specific risk factors relevant to the child].
Defining Characteristics (adapted for pediatric context):
- History of previous falls (though less predictive in very young children, it can indicate underlying issues or environmental risks).
- Altered mobility, balance, or gait (related to developmental stage, injury, or medical condition).
- Sensory or perceptual alterations (vision, hearing, proprioception).
- Cognitive or emotional difficulties (impulsivity, inattention, developmental delay).
- Environmental hazards present in the home, school, or play areas.
- Lack of safety awareness or education (child and caregiver).
- Use of assistive devices (walkers, crutches) – if improperly used or fitted.
- Age less than two years (infants and toddlers are inherently at higher risk).
- Medical conditions or treatments that affect balance, coordination, or alertness.
- Inadequate supervision, especially for young children in environments with fall risks.
Related Factors (specific to pediatrics):
- Age and Developmental Stage: Infants, toddlers, and preschoolers are at higher risk due to rapid motor development and limited judgment.
- Environmental Design: Unsafe home or play environments, including stairs, windows, furniture, and playground equipment.
- Lack of Parental/Caregiver Knowledge: Insufficient understanding of child development and fall prevention strategies.
- Neuromuscular Impairment: Cerebral palsy, muscular dystrophy, spina bifida, or other conditions affecting motor control.
- Sensory Impairment: Visual or auditory deficits.
- Cognitive Impairment: Developmental delays, intellectual disability, attention-deficit/hyperactivity disorder (ADHD).
- Medication Side Effects: Though less common, certain medications can contribute to dizziness or drowsiness.
- Illness or Injury: Acute illnesses causing weakness or dizziness, or injuries affecting mobility.
- Fatigue or Sleep Deprivation: Can impair coordination and judgment.
- Obesity: May affect balance and mobility.
- Poverty or Socioeconomic Factors: Overcrowded living conditions or lack of resources for home safety modifications.
Goals and Expected Outcomes for Pediatric Fall Prevention
The overarching goal of a pediatric care plan for risk of falling is to prevent falls and minimize injuries. Specific goals and expected outcomes should be individualized to the child and family and should be measurable and realistic.
Goals:
- The child will remain free from falls during hospitalization/care setting.
- The child and caregivers will demonstrate understanding of fall risk factors specific to the child’s age and developmental stage.
- Caregivers will implement recommended safety measures in the home and other environments to reduce fall risks.
- The child will participate in age-appropriate activities safely, with minimized risk of falls.
- Caregivers will seek and utilize appropriate resources for fall prevention and home safety modifications.
Expected Outcomes (Measurable Indicators):
- Child experiences no falls during the defined period (e.g., hospital stay, next month).
- Caregivers accurately verbalize at least three fall risk factors relevant to their child.
- Caregivers demonstrate correct use of safety equipment (e.g., stair gates, window guards).
- Home safety assessment checklist is completed and appropriate modifications are implemented.
- Child and caregivers participate in education sessions on fall prevention.
- Caregivers identify and access at least one community resource for child safety.
Nursing Assessment for Pediatric Fall Risk
A thorough nursing assessment is essential to identify children at risk for falls and to tailor interventions effectively. The assessment should be comprehensive, age-appropriate, and consider both intrinsic and extrinsic risk factors.
Key Assessment Areas:
1. History of Falls:
- Inquire about any previous falls, including the circumstances, frequency, and severity of injuries.
- While past falls are less predictive in very young children due to rapid developmental changes, recurrent falls in any age group warrant further investigation.
2. Developmental Assessment:
- Evaluate the child’s current developmental stage and motor skills.
- Assess gross motor skills (walking, running, jumping, climbing) and fine motor skills (grasp, coordination).
- Identify any developmental delays that may impact balance or coordination.
- For infants, assess rolling, sitting, crawling, and pulling to stand abilities.
3. Physical Assessment:
- Neurological Assessment: Assess balance, gait, coordination, muscle strength, and reflexes.
- Sensory Assessment: Evaluate vision and hearing acuity.
- Musculoskeletal Assessment: Assess range of motion, joint stability, and any musculoskeletal abnormalities.
- Medication Review: Review current medications for potential side effects like drowsiness or dizziness.
- General Health Status: Note any acute or chronic illnesses that could contribute to weakness, fatigue, or dizziness.
4. Cognitive and Emotional Assessment:
- Assess cognitive abilities, attention span, and impulsivity, especially in older children.
- Consider emotional state, as stress or anxiety can sometimes contribute to accidents.
- For children with known cognitive impairments or developmental delays, assess their understanding of safety and ability to follow instructions.
5. Environmental Assessment:
- Home Environment: Assess for hazards such as stairs without gates, unsecured windows, unstable furniture, clutter, slippery floors, and inadequate lighting. A home safety checklist can be a useful tool.
- School/Daycare/Playground Environment: Evaluate the safety of these settings, noting potential hazards.
- Observe the environment for age-appropriateness and potential risks for the specific child.
6. Supervision and Caregiver Factors:
- Assess the level of supervision provided, especially for young children.
- Evaluate caregiver knowledge of child development and fall prevention strategies.
- Identify any caregiver limitations that may impact their ability to supervise or create a safe environment (e.g., physical limitations, cognitive impairments, lack of resources).
7. Age-Appropriate Risk Assessment Tools:
- While standardized fall risk assessment tools are more common in adult care, some pediatric-specific tools or adaptations exist.
- Examples include the Pediatric Fall Assessment Tool (PFAT) or modifications of adult tools to suit the pediatric population.
- These tools typically incorporate age, developmental stage, mobility, medications, and environmental factors.
- For infants, consider tools focusing on infant-specific risks like falls from furniture.
Example of Age-Specific Assessment Considerations:
- Infants: Focus on risks at home, especially falls from changing tables, beds, and stairs. Assess parental knowledge of infant safety.
- Toddlers: Assess mobility and exploration behaviors. Evaluate home safety for newly mobile children. Observe playground safety.
- Preschoolers: Assess playground safety, outdoor play habits, and understanding of basic safety rules.
- School-Age Children: Consider sports and recreational activities, playground and school safety, and understanding of safety rules for older children.
Nursing Interventions and Rationales for Pediatric Fall Prevention
Nursing interventions for pediatric fall risk should be tailored to the individual child, their age, developmental stage, risk factors, and environment. Interventions are most effective when they are multifaceted and involve the child, family, and healthcare team.
Categories of Nursing Interventions:
1. Environmental Modifications:
-
Home Safety Assessment and Modifications:
- Conduct a thorough home safety assessment using a checklist or guide.
- Recommend and assist with modifications such as:
- Installing gates at the top and bottom of stairs.
- Securing windows with guards or stops, especially above ground level.
- Removing or securing unstable furniture (bookcases, shelves).
- Padding sharp corners of furniture.
- Using non-slip mats under rugs and in bathrooms.
- Ensuring adequate lighting, especially in hallways and stairs.
- Keeping floors clear of clutter and spills.
- Rationale: Creating a safe home environment minimizes hazards that contribute to falls.
-
Playground and School Safety:
- Advocate for safe playground surfaces (impact-absorbing materials).
- Ensure playground equipment is age-appropriate and well-maintained.
- Promote safe school environments, addressing hazards like slippery floors or cluttered hallways.
- Rationale: Children spend significant time in these settings, and safety measures are crucial.
2. Child and Family Education:
-
Age-Appropriate Safety Education for Children:
- Teach children about fall risks in an age-appropriate manner, using games, stories, or demonstrations.
- Educate on safe play practices, such as not climbing on furniture, using playground equipment safely, and being aware of surroundings.
- For older children and adolescents, discuss risks associated with sports and recreational activities and the importance of safety equipment.
- Rationale: Empowering children with safety knowledge promotes safe behaviors.
-
Parent/Caregiver Education:
- Provide comprehensive education on child development, age-specific fall risks, and prevention strategies.
- Teach parents how to conduct home safety assessments and make necessary modifications.
- Educate on proper supervision techniques, especially for infants and toddlers.
- Discuss the dangers of walkers and jumpers and recommend safer alternatives.
- Provide resources for safety equipment (stair gates, window guards) and home safety assistance programs.
- Rationale: Caregivers are the primary agents in creating and maintaining a safe environment for children.
3. Assistive Devices and Adaptive Equipment (When Appropriate):
-
Proper Use of Assistive Devices:
- If a child requires assistive devices like crutches or walkers due to a medical condition or injury, ensure proper fitting and training in their use.
- Educate both the child and caregivers on safe ambulation techniques with assistive devices.
- Rationale: Improperly used assistive devices can increase fall risk.
-
Adaptive Equipment:
- For children with mobility impairments, recommend and facilitate access to adaptive equipment that enhances safety and mobility (e.g., wheelchairs, adapted strollers, supportive seating).
- Rationale: Adaptive equipment can improve safety and independence for children with special needs.
4. Therapeutic Interventions:
-
Physical Therapy and Occupational Therapy:
- Refer children with balance or motor skill deficits to physical therapy for gait and balance training, strengthening exercises, and gross motor skill development.
- Occupational therapy can address fine motor skills, coordination, and adaptive strategies for daily activities.
- Rationale: Therapy can improve underlying physical abilities that reduce fall risk.
-
Medication Review and Management:
- Collaborate with physicians and pharmacists to review the child’s medications and identify any that may contribute to fall risk.
- Explore alternative medications or dosage adjustments if necessary.
- Rationale: Minimizing medication-related side effects reduces fall risk.
5. Supervision Strategies:
-
Promote Adequate Supervision:
- Emphasize the importance of close supervision, especially for infants, toddlers, and preschoolers, and in hazardous environments.
- Educate caregivers on effective supervision techniques, such as keeping young children within arm’s reach, especially near stairs or elevated surfaces.
- Rationale: Supervision is paramount in preventing falls, especially for young children who are unaware of danger.
-
Safe Play Environments:
- Encourage caregivers to create designated safe play areas indoors and outdoors.
- Advise on choosing age-appropriate and safe toys and play equipment.
- Rationale: Structured safe play areas minimize exposure to hazards.
6. Age-Specific Interventions:
- Infants: Focus on preventing falls from furniture (changing tables, beds), stairs, and walkers. Emphasize constant supervision.
- Toddlers: Address environmental hazards in the home, stair safety, playground safety, and teach basic safety rules.
- Preschoolers: Reinforce playground safety, outdoor play safety, street safety, and promote safe risk-taking within limits.
- School-Age Children: Focus on sports and recreational safety, bicycle safety, playground safety, and reinforce safety rules for older children.
Example Nursing Intervention: Home Safety Education for Parents of a Toddler
- Action: The nurse provides a home safety checklist to the parents of a 15-month-old toddler. The nurse reviews each item with the parents, focusing on stair safety, window safety, furniture stability, and floor hazards. The nurse demonstrates how to install a stair gate and provides resources for obtaining window guards. The nurse also educates the parents on the dangers of baby walkers and recommends alternative activities to promote mobility.
- Rationale: Toddlers are highly mobile and curious, but lack judgment. A home safety assessment and specific education on common toddler fall hazards empower parents to create a safer environment and reduce the risk of falls.
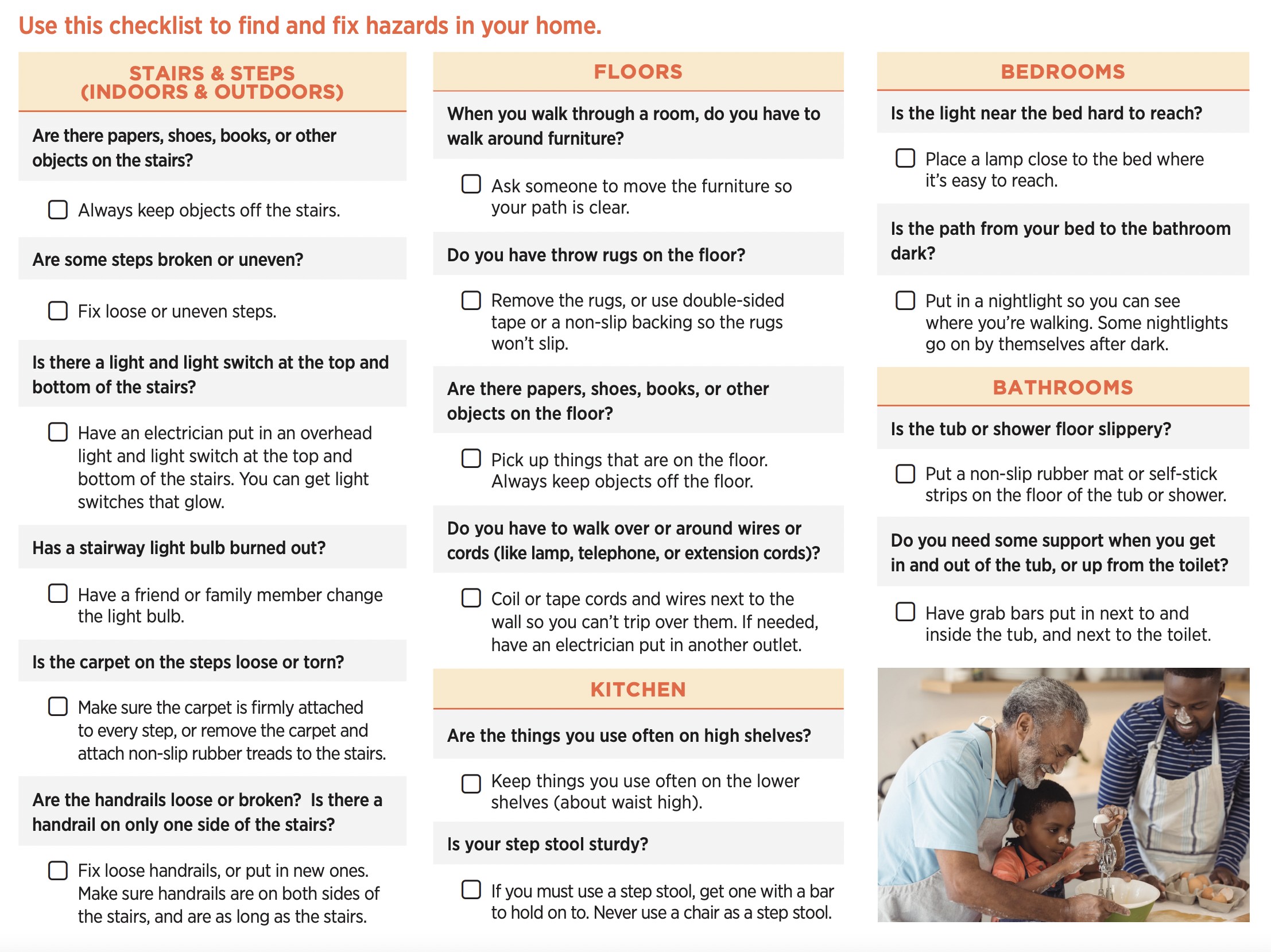 CDC checklist on how to find and fix hazards in homes. Click to enlarge.
CDC checklist on how to find and fix hazards in homes. Click to enlarge.
Conclusion
Preventing falls in children requires a comprehensive and age-appropriate approach. By utilizing a nursing diagnosis of Risk for Falls, nurses can systematically assess risk factors, develop individualized pediatric care plans, and implement evidence-based interventions. These interventions encompass environmental modifications, child and family education, therapeutic approaches, and supervision strategies. Nurses play a vital role in empowering families and communities to create safer environments for children, ultimately reducing the incidence of falls and promoting healthy development. Focusing on the unique needs of each age group, from infants to adolescents, ensures that fall prevention efforts are targeted and effective, contributing to a safer and brighter future for all children.
Recommended Resources
- CDC Childhood Injury Prevention: https://www.cdc.gov/injury/prevention/child/index.html
- American Academy of Pediatrics (AAP) Injury Prevention: https://www.healthychildren.org/English/safety-prevention/Pages/default.aspx
- National Safety Council: https://www.nsc.org/
- Safe Kids Worldwide: https://www.safekids.org/
References and Sources
- Annweiler, C., Montero-Odasso, M., & Beauchet, O. (2010). Vitamin D and falls: systematic review and meta-analysis. Journal of Steroid Biochemistry and Molecular Biology, 121(1-2), 297–301.
- Booth, J.,thorpe, S. K., & Brauer, S. G. (2004). Water-based exercise for improving balance and gait in older adults: systematic review and meta-analysis. Age and Ageing, 33(5), 423–429.
- Centers for Disease Control and Prevention (CDC). (2021). Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2020–2021.
- Chari, S., Haines, T., & Mitchell, D. (2009). Effect of footwear on slip resistance during mobilization, incline and descent in patients with lower limb amputations. Prosthetics and Orthotics International, 33(3), 249–257.
- Cruz, F. D. A. M., de Melo, D. M. M., & de Andrade, D. C. (2020). Falls and functional capacity in frail elderly individuals using and not using assistive devices. Revista Brasileira de Enfermagem, 73(Suppl 3), e20190141.
- Greely, R., Hamilton, S., Sandhu, J., & Wahab, M. (2020). Effectiveness of sitters in reducing falls in hospitalized adults: a systematic review and meta-analysis. JBI Evidence Synthesis, 18(11), 2256–2298.
- Grivnan, J., Baker, D. J., & Vella, M. A. (2017). Childhood falls from windows: A systematic review. Injury, 48(12), 2653–2661.
- Huang, H. T. (2004). Risk factors for falls in community-dwelling elderly persons: a systematic review. Journal of Nursing Research, 12(4), 223–232.
- Lapumnuaypol, K., Thongprayoon, C., Cheungpasitporn, W., & Wijarnpreecha, K. (2019). Proton pump inhibitors and fracture risk: a systematic review and meta-analysis of observational studies. Osteoporosis International, 30(7), 1337–1346.
- Leveille, S. G., Bean, J., Bandeen-Roche, K., Roy, M. A., & Leveille, D. E. (2002). Musculoskeletal pain and risk for falls in older disabled women. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 57(1), M19–M25.
- Lord, S. R., Sherrington, C., Menz, H. B., & Close, J. C. T. (2006). Falls in Older People : Risk Factors and Strategies for Prevention. Journal of Gerontology Series A: Biological Sciences and Medical Sciences, 61(3), 241–268.
- Luo, L., Bell, C. M., & Herrmann, N. (2011). Association between trunk restraint use and falls and fractures in older adults with dementia: a systematic review and meta-analysis. Journal of the American Geriatrics Society, 59(9), 1729–1736.
- Prabhakaran, L., Sharma, H., & Gandhi, A. (2020). Risk factors for fall-related readmissions in older adults: A systematic review and meta-analysis. Geriatrics & Gerontology International, 20(12), 1133–1141.
- Quigley, P. A., Neily, J., & Watson, D. (2015). Reducing falls in hospitals. Joint Commission Journal on Quality and Patient Safety, 41(1), 29–37.
- Ramulu, P. Y., Chan, E. S., Friedman, D. S., & Lam, B. L. (2021). Home lighting and falls in older adults with impaired vision: a systematic review and meta-analysis. JAMA Ophthalmology, 139(5), 559–566.
- Rhalimi, M., & Jaecker, P. (2009). Drug use and falls in hospitalized elderly people: a systematic review. European Journal of Clinical Pharmacology, 65(4), 323–330.
- Rogers, W. A., Meyer, B. J., & Fisk, J. D. (2004). Designing safer homes for older adults: the role of safety experts, design engineers, and older people. Ergonomics, 47(15), 1637–1656.
- Salamon, J., Shaughnessy, M., & Sands, L. (2012). Falls in stroke patients during acute rehabilitation: incidence and predictors. Archives of Physical Medicine and Rehabilitation, 93(1), 15–21.
- Samardzic, M., Mijatovic, M., & Popovic, N. (2020). Group exercise programmes for older adults: a systematic review. Journal of Physical Therapy Science, 32(1), 1–9.
- Sevdalis, N., Mannion, R., & Davies, H. T. O. (2009). Patient identification in hospitals: a systematic review of the literature. BMJ Quality & Safety, 18(3), 173–180.
- Stanmore, E. K., Oldham, J., & Skilbeck, C. J. (2013). Falls in people with rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care & Research, 65(1), 91–101.
- Tencer, A. F., Koepsell, T. D., & Wolf, M. E. (2004). Biomechanical and epidemiological studies of footwear as a risk factor for falls in older adults. Journal of the American Geriatrics Society, 52(11), 1840–1846.
- Tzeng, H. M., & Yin, C. Y. (2010). Nurses’ responsiveness to patients’ call lights: a compensatory mechanism in responding to patient falls? Journal of Nursing Scholarship, 42(1), 73–81.
- Wood, J. M., Lacherez, P., & Black, A. A. (2011). Visual impairment and falls in older adults with age-related macular degeneration. Investigative Ophthalmology & Visual Science, 52(1), 1–18.