Peptic ulcer disease, commonly referred to as stomach ulcers, presents a significant health challenge affecting individuals across various age groups. As a content creator for xentrydiagnosis.store and an automotive repair expert transitioning to health content, I aim to provide a detailed guide focusing on nursing diagnoses crucial for managing patients with stomach ulcers. This article delves into the essential nursing diagnoses, building upon the foundational knowledge of peptic ulcer disease to equip healthcare professionals with the necessary insights for optimal patient care.
Understanding Peptic Ulcer Disease
A peptic ulcer is a lesion in the mucosal lining of the upper gastrointestinal tract, occurring in areas exposed to gastric acid and pepsin. These ulcers can be classified based on their location, primarily as gastric, duodenal, or esophageal ulcers. Gastric ulcers are typically found in the stomach, often near the pylorus. Duodenal ulcers, more prevalent than gastric ulcers, occur in the duodenum, the first part of the small intestine. Esophageal ulcers result from the reflux of stomach acid into the esophagus.
Pathophysiology of Peptic Ulcers
Peptic ulcer disease arises from an imbalance between aggressive factors that damage the mucosa and defensive mechanisms that protect it. The primary aggressive factors include gastric acid and pepsin, while mucosal defense is maintained by mucus secretion, bicarbonate, blood flow, and prostaglandins. When these defensive mechanisms are disrupted, the mucosa becomes vulnerable to erosion and ulceration.
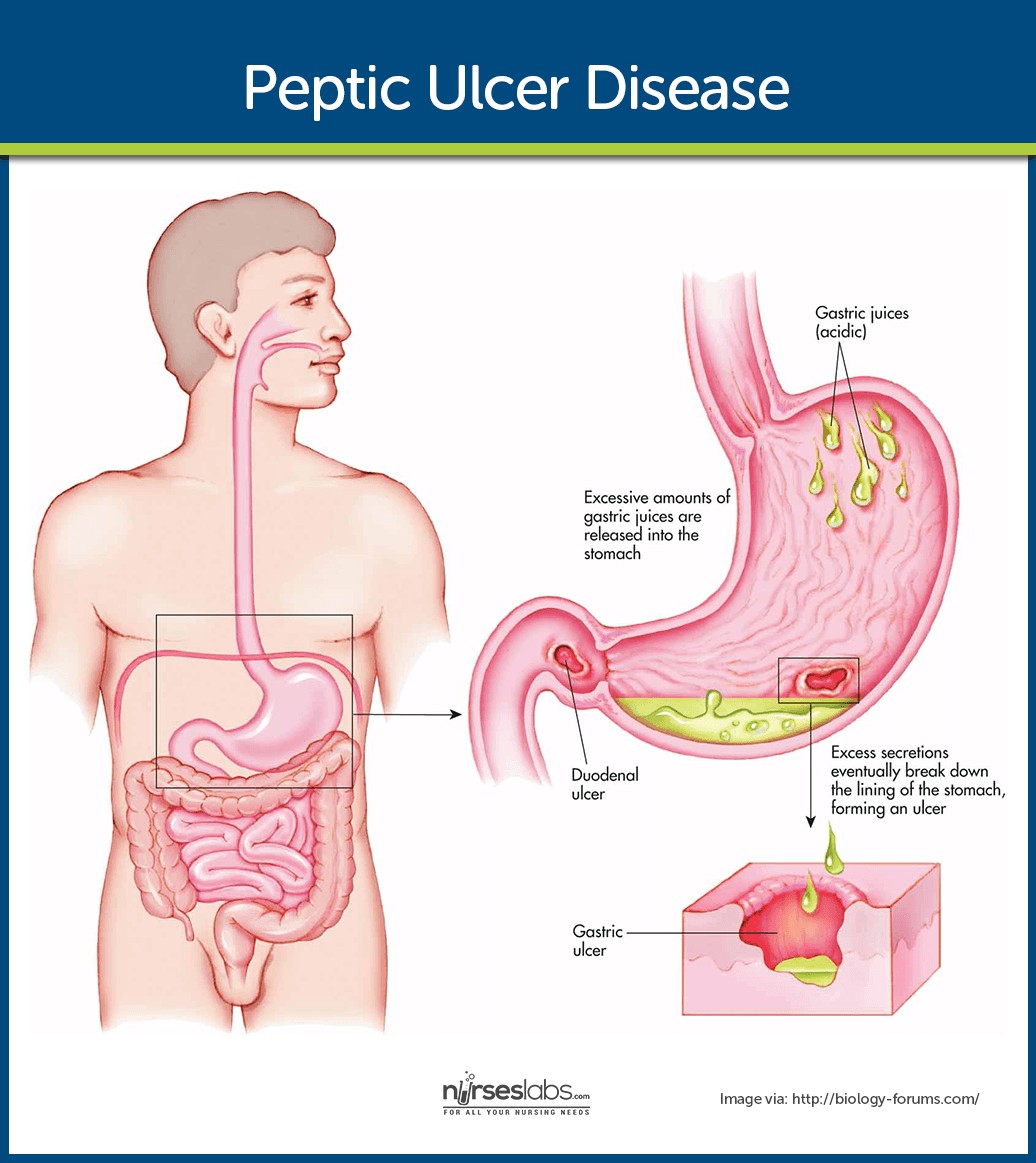 Peptic Ulcer Disease Visual Pathophysiology
Peptic Ulcer Disease Visual Pathophysiology
Visual representation of peptic ulcer disease pathophysiology, illustrating the erosive process on the gastroduodenal mucosa.
The erosion process begins with mucosal damage due to increased acid-pepsin activity or decreased mucosal resistance. A compromised mucosa is unable to secrete sufficient mucus, weakening the protective barrier against hydrochloric acid (HCl). Interestingly, acid secretion levels vary depending on the ulcer type; patients with duodenal ulcers often hypersecrete acid, while those with gastric ulcers may have normal or reduced acid secretion. A critical factor in peptic ulcer development is decreased mucosal resistance, which increases susceptibility to bacterial infection, particularly by Helicobacter pylori (H. pylori).
Epidemiology and Risk Factors
Peptic ulcer disease affects both genders and all age groups, although it is most common between 40 and 60 years of age. Before menopause, women are less frequently affected; however, post-menopause, the incidence rate nearly equals that of men. Several factors contribute to the development of peptic ulcers. Infection with H. pylori is a leading cause, alongside chronic use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and conditions causing hypersecretion of gastric acid, such as Zollinger-Ellison syndrome.
H. pylori infection, often acquired through contaminated food and water, damages the protective mucous layer of the stomach and duodenum. NSAIDs, including salicylates, inhibit prostaglandin secretion, which is crucial for mucosal protection. Other illnesses like pancreatitis, hepatic disease, Crohn’s disease, and gastritis also increase ulcer risk. Lifestyle factors, including excessive alcohol, caffeine, and smoking, can exacerbate acid secretion and delay ulcer healing. Blood type may also play a role; gastric ulcers are more common in individuals with type A blood, while duodenal ulcers are more frequently seen in those with type O blood.
Clinical Presentation and Complications
The symptoms of peptic ulcers can be cyclical, lasting weeks or months, with periods of remission and exacerbation. Common clinical manifestations include abdominal pain, often described as burning or gnawing, typically located in the epigastric region. Pain may be relieved or worsened by eating, depending on the ulcer location (food may buffer acid in gastric ulcers but exacerbate pain in duodenal ulcers when the stomach empties and acid irritates the duodenum). Other symptoms include bloating, nausea, vomiting, and loss of appetite.
Untreated peptic ulcers can lead to severe complications. Hemorrhage is the most frequent complication, manifesting as hematemesis (vomiting blood) or melena (dark, tarry stools). Perforation, a life-threatening complication, occurs when the ulcer erodes through the stomach or duodenal wall into the peritoneal cavity, causing peritonitis. Penetration involves ulcer erosion into adjacent organs like the pancreas. Pyloric obstruction can develop due to scarring and edema near the pyloric sphincter, leading to gastric outlet obstruction with symptoms of vomiting and abdominal distention.
Diagnosis and Management
Diagnosing peptic ulcer disease involves a combination of clinical assessment and diagnostic procedures. Esophagogastroduodenoscopy (EGD) is the gold standard, allowing direct visualization of the mucosa, ulcer confirmation, and tissue biopsy to rule out H. pylori infection or malignancy. Physical examination may reveal epigastric tenderness and signs of complications. Barium studies of the upper GI tract can identify ulcers, although endoscopy is preferred for its accuracy and therapeutic capabilities. Stool tests for occult blood and urea breath tests for H. pylori activity are also valuable diagnostic tools.
Medical management aims to eradicate H. pylori infection, reduce gastric acidity, and protect the mucosa. Proton pump inhibitors (PPIs) and H2 receptor antagonists are commonly used to decrease acid production. Antibiotic therapy, typically a combination of medications, is prescribed to eradicate H. pylori. Mucosal protectants like sucralfate and bismuth subsalicylate can promote ulcer healing. Lifestyle modifications, including smoking cessation, avoiding NSAIDs and trigger foods, and stress reduction, are crucial. Surgical interventions, such as pyloroplasty and antrectomy, are now less common due to effective medical treatments but may be necessary in cases of complications or treatment failure.
Nursing Diagnoses for Peptic Ulcer
Nursing care for patients with peptic ulcer disease is crucial for symptom management, preventing complications, and promoting healing. Accurate nursing diagnoses guide the development of effective care plans. Based on the assessment data of a patient with a stomach ulcer, several nursing diagnoses may be applicable:
-
Acute Pain related to gastric mucosal irritation secondary to peptic ulcer disease, as evidenced by patient reports of epigastric pain, guarding behavior, and changes in vital signs.
This diagnosis addresses the primary symptom of peptic ulcers: pain. The pain arises from the ulcer’s erosion into the sensitive mucosal lining, exposing nerve endings to gastric acid and digestive enzymes.
-
Risk for Bleeding related to peptic ulcer erosion into blood vessels.
Peptic ulcers can erode through the mucosal and submucosal layers and into blood vessels, leading to hemorrhage. This risk diagnosis highlights the potential for a severe complication requiring vigilant monitoring.
-
Imbalanced Nutrition: Less than Body Requirements related to anorexia, nausea, and pain associated with peptic ulcer disease, as evidenced by reported decreased food intake, weight loss, and aversion to eating.
Pain and gastrointestinal symptoms can significantly reduce a patient’s appetite and ability to eat, leading to nutritional deficits that impede healing and overall recovery.
-
Deficient Knowledge regarding peptic ulcer disease, treatment regimen, lifestyle modifications, and prevention of recurrence, as evidenced by patient questions and statements of misinformation.
Effective management and prevention of ulcer recurrence rely heavily on patient understanding and adherence to the treatment plan and lifestyle changes. Knowledge deficit is a key barrier to successful self-management.
-
Anxiety related to the diagnosis of peptic ulcer disease, pain, potential complications, and lifestyle changes, as evidenced by patient expressions of worry, restlessness, and increased heart rate.
The discomfort, chronicity, and potential complications of peptic ulcer disease can induce significant anxiety in patients. Addressing this emotional distress is an integral part of holistic nursing care.
-
Risk for Deficient Fluid Volume related to vomiting secondary to peptic ulcer disease.
Persistent vomiting, a symptom in some peptic ulcer cases, can lead to dehydration and electrolyte imbalances. This risk diagnosis emphasizes the need to monitor fluid status and prevent dehydration.
-
Ineffective Health Management related to complexity of treatment regimen and required lifestyle modifications for peptic ulcer disease.
Managing peptic ulcer disease involves multiple medications, dietary changes, and lifestyle adjustments. Ineffective health management can occur if the patient struggles to integrate these recommendations into their daily life.
Nursing Interventions and Care Planning
Nursing interventions are tailored to address the identified nursing diagnoses and patient-specific needs.
For Acute Pain:
- Administer prescribed analgesics and antacids as ordered and evaluate their effectiveness.
- Encourage the patient to identify and avoid foods and beverages that exacerbate pain, such as spicy foods, caffeine, and alcohol.
- Promote relaxation techniques such as deep breathing exercises and meditation to manage pain perception.
- Ensure regular meal schedules in a relaxed environment to minimize gastric irritation.
For Risk for Bleeding:
- Monitor vital signs closely for signs of hypovolemia, such as tachycardia, hypotension, and pallor.
- Assess for signs of gastrointestinal bleeding, including hematemesis and melena.
- Administer prescribed medications, such as proton pump inhibitors, to reduce gastric acid and promote ulcer healing.
- Prepare for potential interventions such as blood transfusions and endoscopic procedures if bleeding occurs.
For Imbalanced Nutrition: Less than Body Requirements:
- Assess nutritional status, including weight, dietary intake, and laboratory values.
- Provide small, frequent, and easily digestible meals to improve nutritional intake and reduce gastric discomfort.
- Consult with a dietitian to develop an individualized meal plan that meets the patient’s nutritional needs and preferences.
- Administer antiemetics as prescribed to manage nausea and improve appetite.
For Deficient Knowledge:
- Provide comprehensive patient education about peptic ulcer disease, its causes, symptoms, treatment, and prevention.
- Explain the importance of medication adherence, lifestyle modifications, and follow-up care.
- Utilize various teaching methods, including verbal instructions, written materials, and visual aids, to enhance understanding.
- Encourage the patient to ask questions and address any misconceptions.
For Anxiety:
- Assess the patient’s level of anxiety and coping mechanisms.
- Provide a calm and supportive environment to encourage open expression of feelings and concerns.
- Offer reassurance and accurate information to alleviate anxiety related to the disease and treatment.
- Teach stress-reduction techniques and coping strategies.
For Risk for Deficient Fluid Volume:
- Monitor fluid intake and output, and assess for signs of dehydration.
- Encourage oral fluid intake as tolerated.
- Administer intravenous fluids and electrolytes as prescribed to correct fluid imbalances if vomiting is persistent.
For Ineffective Health Management:
- Assess the patient’s understanding of the treatment plan and their ability to adhere to recommendations.
- Simplify the treatment regimen and provide clear, concise instructions.
- Collaborate with the patient to develop realistic and achievable goals for self-management.
- Provide resources and support systems to assist with lifestyle modifications and medication management.
Evaluation and Expected Outcomes
Expected patient outcomes following nursing interventions include:
- Relief of pain as reported by the patient and demonstrated by improved comfort levels.
- Absence of bleeding or prompt management of bleeding episodes.
- Attainment of adequate nutritional intake to meet metabolic needs.
- Demonstrated understanding of peptic ulcer disease, treatment, and self-management strategies.
- Reduction in anxiety and improved coping mechanisms.
- Maintenance of fluid balance.
- Effective self-management of the peptic ulcer condition and prevention of recurrence.
Discharge Planning and Home Care
Prior to discharge, comprehensive self-care education is essential. Patients should receive detailed instructions regarding medications, dietary guidelines, lifestyle modifications, and signs and symptoms of complications that warrant immediate medical attention. Emphasize the importance of adhering to the prescribed treatment regimen and attending follow-up appointments to ensure optimal long-term management and prevent ulcer recurrence. Reinforce the need to avoid NSAIDs, smoking, and excessive alcohol and caffeine intake. Encourage a relaxed eating environment and stress management techniques as part of their daily routine.
Conclusion
Effective nursing care for patients with peptic ulcer disease hinges on accurate nursing diagnoses and well-planned interventions. By addressing key issues such as pain management, risk of bleeding, nutritional support, knowledge deficits, and anxiety, nurses play a pivotal role in improving patient outcomes and quality of life. This comprehensive guide aims to enhance the understanding of nursing diagnoses relevant to stomach ulcers, empowering healthcare professionals to deliver patient-centered care that promotes healing and prevents complications.