A wound, defined as any disruption to the skin’s integrity and underlying tissues, represents a significant challenge in healthcare. From minor abrasions to complex surgical incisions, wounds can compromise the body’s protective barrier, increasing the risk of infection and hindering normal function. Effective wound care is paramount, not only for physical healing but also for a patient’s overall well-being. This necessitates a holistic approach, starting with accurate assessment and culminating in tailored interventions. Central to this process is the Nursing Diagnosis For Wound Care, which provides a structured framework for identifying patient needs, guiding care planning, and evaluating outcomes.
This article delves into the essential aspects of wound care through the lens of nursing diagnoses. We will explore the types of wounds, the intricate process of wound healing, and the crucial role of the nursing process in effective management. Furthermore, we will provide a detailed overview of key nursing diagnoses relevant to wound care, equipping healthcare professionals with the knowledge to deliver optimal, patient-centered care. Understanding and applying appropriate nursing diagnoses for wound care is fundamental to promoting healing, preventing complications, and enhancing the quality of life for individuals with wounds.
Understanding Wound Infection
Wound infection occurs when pathogenic microorganisms breach the body’s natural defenses, colonizing and multiplying within the wound bed. This invasion can overwhelm the immune system, leading to localized and potentially systemic complications. Compromised aseptic technique during wound management and direct contamination of the wound are primary culprits. Individuals with underlying conditions such as diabetes mellitus or HIV, which weaken the immune system or impede healing, are at a significantly elevated risk of developing wound infections.
Untreated wound infections can escalate into severe and life-threatening conditions, including:
- Cellulitis: A spreading bacterial infection of the skin and subcutaneous tissues, characterized by redness, warmth, swelling, and pain.
- Abscess: A localized collection of pus within the tissue, often requiring drainage.
- Osteomyelitis: Infection of the bone, a serious complication that can result from deep or chronic wounds.
- Sepsis: A systemic inflammatory response to infection, potentially leading to organ dysfunction and death.
Recognizing the signs of wound infection is crucial for prompt intervention. Key indicators include purulent discharge, skin discoloration, swelling, foul odor, and localized warmth and tenderness. Systemic symptoms such as fever, chills, and lymphadenopathy may indicate a more severe, spreading infection requiring immediate medical attention.
Alternative Text: A nurse carefully assesses a patient’s wound, demonstrating key steps in wound evaluation for effective nursing diagnosis and care planning.
The Process of Wound Healing
Wound healing, or tissue integrity restoration, is a complex biological process that commences immediately following skin injury. Any disruption or delay in this intricate process can significantly increase the susceptibility to infection and impede recovery. Understanding the phases of wound healing is fundamental for nurses to provide targeted and effective care.
Wound healing progresses through four distinct, yet overlapping phases:
- Hemostasis (Immediate): This initial phase is characterized by the body’s immediate response to injury. Blood vessels constrict to minimize blood loss, coagulation pathways are activated to form a blood clot, and platelets aggregate at the wound site to initiate sealing. The primary goal of hemostasis is to stop bleeding and create a temporary matrix for subsequent healing phases.
- Inflammation (0-4 Days): The inflammatory phase is essential for clearing debris and pathogens from the wound and setting the stage for tissue repair. The immune system mobilizes neutrophils and macrophages to the wound site to combat potential infection. This phase is clinically characterized by classic signs of inflammation: swelling, redness, heat, and pain. While essential, prolonged or excessive inflammation can hinder healing.
- Proliferation (2-24 Days): This phase marks the rebuilding of damaged tissue. Granulation tissue, a richly vascularized connective tissue, fills the wound bed, providing a foundation for new tissue growth. Epithelial cells migrate across the wound surface, eventually covering the granulation tissue and closing the wound. Collagen synthesis also occurs, adding strength and structure to the healing tissue.
- Maturation (24+ Days): The maturation phase, also known as remodeling, is the longest phase of wound healing and can continue for months or even years. During this phase, collagen fibers reorganize and cross-link, increasing the tensile strength of the wound. Scar tissue forms, and while it may never regain the full strength of the original tissue, it provides a durable closure.
Types of Wound Healing
Wound healing can occur through different mechanisms, primarily classified by how the wound edges are managed:
- Primary Intention: This type of healing occurs when wound edges are approximated, meaning they are brought together and closed. This is typically achieved using sutures, staples, surgical glue, or adhesive strips (Steri-Strips). Primary intention healing is common in surgical incisions, lacerations with clean edges, and well-approximated wounds. It results in minimal scarring and a relatively rapid healing process.
- Secondary Intention: Secondary intention healing is necessary when wound edges cannot be easily approximated, often due to tissue loss, infection, or delayed intervention. In these wounds, the body heals from the base upwards by producing granulation tissue to fill the wound cavity. Examples include pressure ulcers, large open wounds, and wounds with significant tissue loss. Secondary intention healing takes longer and results in more significant scarring compared to primary intention. There is also a higher risk of infection due to the prolonged open wound.
- Tertiary Intention (Delayed Primary Closure): Tertiary intention, also known as delayed primary closure, is a combination of primary and secondary intention. The wound is initially left open, typically to allow for drainage and to reduce infection risk. Once the wound is deemed clean and infection-free, it is surgically closed using sutures or staples. This method is often used for contaminated wounds, wounds with significant edema, or when there is a need to observe the wound bed before closure.
Factors Influencing Wound Healing
Numerous factors can significantly impact the body’s capacity to heal wounds effectively. Nurses must consider these factors during assessment and care planning to optimize patient outcomes. These factors can be broadly categorized as patient-related and wound-related:
Patient-Related Factors:
- Nutritional Status: Adequate nutrition, particularly protein, vitamins (especially Vitamin C and Zinc), and minerals, is crucial for tissue repair and regeneration. Malnutrition can severely impair wound healing.
- Stress: Psychological and physiological stress can negatively impact the immune system and delay wound healing.
- Comorbidities: Underlying health conditions such as diabetes mellitus, peripheral vascular disease, and autoimmune disorders can significantly impair circulation, immune function, and overall healing capacity.
- Age: The aging process is associated with physiological changes that can slow down wound healing, including decreased collagen synthesis, reduced immune response, and impaired circulation.
- Obesity: Obesity can increase the risk of wound complications and delay healing due to factors like poor circulation in adipose tissue and increased inflammatory mediators.
- Medications: Certain medications, such as corticosteroids, chemotherapy drugs, and immunosuppressants, can interfere with the inflammatory and proliferative phases of wound healing.
- Alcohol Use: Excessive alcohol consumption can impair immune function, nutritional status, and wound healing.
- Smoking: Smoking significantly impairs wound healing by constricting blood vessels, reducing oxygen delivery to tissues, and interfering with collagen synthesis.
- Friction and Shearing Forces: These mechanical forces can cause tissue damage and breakdown, particularly in individuals with limited mobility, increasing the risk of pressure ulcers.
- Poor Mobility: Immobility reduces circulation and increases pressure on specific body areas, predisposing individuals to pressure ulcers and hindering overall wound healing.
- Knowledge Deficits: Lack of understanding about proper wound care, nutrition, and preventative measures can negatively impact healing outcomes.
Wound-Related Factors:
- Wound Type and Location: The type of wound (e.g., surgical, traumatic, ulcer) and its location on the body can influence healing rates and potential complications.
- Wound Size and Depth: Larger and deeper wounds naturally require more time and resources to heal.
- Wound Bed Condition: The presence of necrotic tissue (eschar), slough, or infection within the wound bed can significantly impede healing.
- Wound Drainage: Excessive or inadequate wound drainage can disrupt the healing environment.
- Infection: Wound infection is a major impediment to healing, prolonging inflammation and damaging tissues.
- Foreign Bodies: The presence of foreign materials in the wound can trigger inflammation and infection, delaying healing.
The Nursing Process in Wound Care
The nursing process provides a systematic, patient-centered approach to wound care, ensuring comprehensive and individualized management. It encompasses assessment, diagnosis (nursing diagnosis), planning, implementation, and evaluation, forming a continuous cycle of care.
For wound care, the nursing process is crucial for:
- Identifying Patient Needs: Thorough assessment helps identify specific patient needs related to their wound, overall health status, and lifestyle factors.
- Developing Individualized Care Plans: Nursing diagnoses guide the development of tailored care plans that address identified needs and promote optimal wound healing.
- Implementing Effective Interventions: Care plans outline specific nursing interventions, such as wound cleansing, dressing changes, pain management, and infection control measures.
- Evaluating Outcomes: Regular evaluation of wound healing progress and patient response to interventions allows for adjustments to the care plan, ensuring effectiveness and optimal outcomes.
A consultation with a wound care specialist or certified wound care nurse is highly recommended for managing complex, chronic, or non-healing wounds. These specialists possess advanced knowledge and skills in wound management, ensuring patients receive the most appropriate and evidence-based care.
Nursing Assessment: Gathering Subjective and Objective Data
The initial step in the nursing process is a comprehensive nursing assessment. This involves gathering both subjective data (what the patient reports) and objective data (what the nurse observes and measures) to gain a holistic understanding of the patient’s condition and wound characteristics.
Review of Health History (Subjective Data)
Obtaining a detailed health history is crucial for identifying potential risk factors, understanding the etiology of the wound, and recognizing signs of infection.
1. Determine General Symptoms: Inquire about symptoms indicative of wound infection:
- Purulent discharge from the wound
- Skin discoloration (increased redness, unusual pallor)
- Swelling (localized or spreading)
- Foul-smelling odor
- Warmth, tenderness, pain, or inflammation at the wound site
Also, assess for systemic symptoms that may signal severe infection:
- Fever
- Chills
- Lymphadenopathy (swollen lymph nodes) near the wound
2. Assess the Underlying Cause of the Wound: Explore the circumstances surrounding wound development:
- Accidents and trauma
- Immobility and pressure
- Surgical procedures
- Underlying medical conditions
Understand how the wound occurred to identify potential contamination risks and guide preventative measures.
3. Identify Medical Risk Factors: Elucidate pre-existing conditions that increase wound risk or impair healing:
- Diabetes mellitus
- Immunosuppression (HIV, autoimmune diseases)
- Renal failure
- Obesity
- Advancing age
- Neuropathy (peripheral or autonomic)
- Peripheral vascular disease
- Treatments or medications (chemotherapy, radiation therapy, immunosuppressants)
4. Review Surgical Record (If Applicable): For surgical wounds, consider factors that may increase infection risk:
- Poor surgical technique
- Prolonged hospital stay pre- or post-surgery
- Intraoperative contamination
- Hypothermia during surgery
5. Review Medication List: Identify medications that can delay wound healing:
- Hydroxyurea
- Chemotherapeutic drugs
- Steroids (corticosteroids)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Disease-modifying antirheumatic drugs (DMARDs)
6. Inquire About Nutritional Status: Assess dietary intake to identify potential nutritional deficiencies:
- Protein intake
- Vitamin and mineral intake
- Fluid intake (hydration status)
Protein, vitamins, minerals, and adequate hydration are essential for optimal wound healing.
Alternative Text: Illustration depicting the four distinct stages of wound healing: hemostasis, inflammation, proliferation, and maturation, emphasizing the dynamic and sequential nature of tissue repair.
Physical Assessment (Objective Data)
Physical assessment provides crucial objective data about the wound itself and the surrounding tissue.
1. Determine Wound Type: Identify the specific type of wound, as this will guide care:
- Skin tears
- Diabetic foot ulcers
- Arterial ulcers
- Venous stasis ulcers
- Pressure ulcers (stages I-IV, unstageable, deep tissue injury)
- Surgical wounds (incision, excision)
- Traumatic wounds (abrasions, lacerations, punctures, avulsions)
2. Assess and Document Wound Findings: Document detailed wound characteristics at each dressing change or as per facility protocol:
- Location: Anatomical site of the wound.
- Size: Length, width, and depth in centimeters.
- Drainage: Type, color, amount, and odor of exudate (serous, sanguinous, serosanguinous, purulent).
- Wound Bed: Description of tissue types present (granulation tissue, slough, eschar, exposed muscle/bone).
- Wound Edges and Periwound Skin: Condition of wound edges (approximated, unapproximated, rolled) and surrounding skin (erythema, edema, maceration, induration).
- Tunneling or Undermining: Presence and extent of tissue tracts extending from the wound edge.
- Signs of Infection: Redness, warmth, swelling, pain, purulent drainage, foul odor.
3. Utilize the T.I.M.E. Acronym for Wound Bed Assessment: This structured approach aids in comprehensive wound evaluation:
- T – Tissue: Assess tissue type in the wound bed:
- Epithelial tissue (pink): Indicates advancing wound closure.
- Granulation tissue (red, beefy): Healthy, new connective tissue indicating healing.
- Slough (yellow/gray, stringy): Nonviable, moist tissue that needs to be removed.
- Necrotic tissue/Eschar (black, dry, leathery): Dead tissue that impedes healing and must be debrided.
- I – Infection/Inflammation: Differentiate between normal inflammation (expected in healing) and infection (abnormal and detrimental):
- Inflammation: Localized redness, warmth, mild swelling, and pain are normal in the initial healing phases.
- Infection: Spreading redness, significant warmth and swelling, purulent drainage, foul odor, increased pain, fever, and elevated white blood cell count are indicative of infection.
- M – Moisture Balance: Assess wound moisture levels:
- Moist wound bed: Optimal for healing, promoting cell migration and nutrient delivery.
- Excessive moisture (maceration): Skin softening and breakdown due to prolonged exposure to exudate.
- Insufficient moisture (dry wound bed): Can impede cell migration and lead to cell death.
- Exudate assessment: Note type (serous, sanguinous, serosanguinous, purulent), amount (scant, moderate, copious), color, and odor.
- E – Edge Advancement: Monitor wound edges for progress in closure:
- Well-defined, advancing edges: Indicate healing.
- Rolled or epibolic edges: Edges that have rolled under, hindering epithelial migration and wound closure.
- Undermining or tunneling: Indicate tissue destruction extending beneath intact skin at the wound edge.
- Periwound skin assessment: Evaluate for erythema, edema, maceration, or induration, which may indicate complications or delayed healing.
4. Pain Assessment: Quantify and characterize wound-related pain:
- Utilize a validated pain scale (numerical rating scale, visual analog scale) to assess pain intensity.
- Determine pain characteristics (sharp, dull, burning, aching, throbbing).
- Assess factors that exacerbate or alleviate pain.
Diagnostic Procedures
Diagnostic procedures provide objective data to confirm infection, identify causative pathogens, and assess factors affecting wound healing.
1. Wound Culture: Obtain a wound swab for culture and sensitivity testing:
- Swab culture: A non-invasive and cost-effective method to identify bacterial pathogens in superficial wounds.
- Culture and sensitivity testing determines the specific microorganisms present and their susceptibility to antibiotics, guiding targeted antimicrobial therapy.
2. Biopsy or Aspiration: Prepare for more invasive sample collection if indicated:
- Tissue biopsy: The most accurate method for identifying pathogens, particularly in deep or chronic wounds. Involves surgically removing a small tissue sample for analysis.
- Aspiration of fluid: Used to assess for infection in deeper tissues or abscesses. Fluid is aspirated using a needle and syringe for culture and analysis.
3. Laboratory Values: Send blood samples for laboratory analysis to assess for systemic infection and overall health status:
- White blood cell (WBC) count: Elevated WBC count is a common indicator of infection.
- C-reactive protein (CRP): An acute-phase reactant protein that increases in response to inflammation and infection.
- Procalcitonin (PCT): A more specific marker for bacterial infection than CRP.
- Presepsin: Another biomarker that rises early in sepsis and bacterial infections.
- Microbial DNA testing: Detects the presence of microbial DNA in the wound, aiding in pathogen identification.
- Bacterial protease activity (BPA): Measures the activity of bacterial enzymes in the wound, indicating bacterial burden.
4. Imaging Studies: Prepare the patient for imaging as ordered to evaluate deeper tissue involvement or complications:
- Plain X-rays: Detect radiopaque foreign bodies and assess for osteomyelitis (bone infection).
- Computed tomography (CT scan): Provides detailed images of soft tissues and can identify deep tissue infections or intra-abdominal abscesses.
- Magnetic resonance imaging (MRI): Offers excellent soft tissue detail and is useful for assessing the extent of infection in tissues and bone.
- Ultrasound: Can visualize skin and soft tissue infections, abscesses, and fluid collections.
5. Peripheral Perfusion Assessment: Determine adequacy of blood flow to the extremities:
- Ankle-brachial index (ABI) and toe-brachial index (TBI): Non-invasive tests to assess for peripheral artery disease by comparing blood pressure in the ankles/toes to the brachial artery.
- Monofilament testing: Evaluates protective sensation in the feet, particularly important for patients with diabetes or peripheral neuropathy, to identify risk for foot ulcers.
Nursing Interventions: Implementing Evidence-Based Wound Care
Nursing interventions are crucial for promoting wound healing, preventing infection, managing pain, and supporting the patient’s overall well-being.
Providing Appropriate Wound Care
1. Debridement of Nonviable Tissue: Remove necrotic tissue to promote healing:
- Autolytic debridement: Using the body’s own enzymes to break down necrotic tissue through moisture-retentive dressings (hydrogels, hydrocolloids).
- Enzymatic debridement: Applying prescribed topical enzymes to digest necrotic tissue (collagenase).
- Sharp debridement: Surgical removal of necrotic tissue using sharp instruments (scalpel, scissors), performed by trained professionals.
2. Moisture Balance: Maintain optimal wound moisture:
- Utilize dressings that manage exudate effectively. Hydrofiber or alginate dressings are highly absorbent for wounds with heavy drainage.
- Consider hydrogels for dry wounds to provide moisture and promote autolytic debridement.
- Change dressings frequently as needed to prevent maceration or wound dryness.
3. Wound Packing for Tunneling: Fill dead space in wounds with tunneling or undermining:
- Pack loosely with moistened sterile gauze or hydrogel-impregnated dressings to maintain a moist wound bed and prevent premature wound closure from the surface.
- Avoid overpacking, which can increase pressure and impede healing.
4. Periwound Skin Protection: Protect the skin surrounding the wound:
- Apply barrier creams, powders, protective wipes, or barrier wafers to the periwound skin to prevent maceration and irritation from wound exudate or adhesive dressings.
5. Wound Vac Therapy: Consider vacuum-assisted closure (VAC) for specific wound types:
- Wound VACs are effective for open wounds, skin grafts, flaps, and pressure ulcers.
- They utilize negative pressure to remove excess fluid, reduce edema, promote granulation tissue formation, and enhance wound closure.
6. Pain Management: Address wound-related pain:
- Premedicate with prescribed analgesics (oral or intravenous) prior to dressing changes or debridement procedures to minimize pain and anxiety.
- Utilize non-pharmacological pain management strategies such as positioning, distraction, and relaxation techniques.
Preventing and Managing Infection
1. Aseptic or Clean Technique: Adhere to appropriate infection control practices:
- Aseptic technique (sterile technique): Use sterile gloves and sterile equipment for high-risk wounds, such as burns, surgical wounds, and immunocompromised patients, to prevent introducing pathogens.
- Clean technique (non-sterile technique): Use clean gloves and clean equipment for chronic wounds like pressure ulcers and simple wounds like skin tears when aseptic technique is not mandated.
2. Antibiotic Administration: Administer antibiotics as prescribed:
- Topical antibiotics or silver dressings may be used for localized wound infections.
- Oral or intravenous antibiotics are necessary for systemic infections or wounds with signs of spreading infection (cellulitis, sepsis).
- Targeted antimicrobial therapy should be based on wound culture and sensitivity results.
3. Immediate Wound Cleaning: Emphasize the importance of prompt wound cleaning:
- Clean wounds immediately with mild soap and water to remove debris and reduce bacterial contamination, especially for “dirty” wounds (animal bites, contaminated objects).
- Encourage patients to seek medical attention if they are unable to clean the wound adequately themselves or if there is concern for infection.
4. Avoid Harsh Cleansing Agents: Educate patients to avoid using hydrogen peroxide or rubbing alcohol:
- These agents are cytotoxic and can damage healthy tissue, delaying wound healing.
- Recommend gentle wound cleansing with mild soap and water or sterile saline.
5. Hand Hygiene: Reinforce the importance of hand hygiene:
- Meticulous handwashing with soap and water or using alcohol-based hand sanitizer before and after wound care is essential to prevent infection transmission.
6. Wound Coverage: Educate patients about the benefits of wound dressings:
- Counter the myth that wounds need to “breathe.” Explain that dressings maintain a moist wound environment, promote healing, and protect against bacterial contamination.
- Ensure appropriate dressing selection based on wound type, exudate level, and healing phase.
Promoting Wound Healing
1. Nutritional and Hydration Support: Optimize nutritional intake:
- Recommend a high-protein diet to support tissue repair and regeneration.
- Suggest protein-enriched drinks as supplements if dietary protein intake is insufficient.
- Encourage adequate intake of Vitamin C, zinc, and other essential nutrients for wound healing.
- Promote adequate fluid intake to maintain hydration, support blood circulation, and deliver nutrients to the wound bed.
2. Education on Skin Breakdown Prevention: Educate patients and families on preventative strategies:
- Minimize pressure by frequent turning and repositioning (every 2 hours for bedridden patients).
- Use pressure-redistributing support surfaces (specialty mattresses, cushions).
- Encourage regular mobility and ambulation as tolerated.
- Advise patients to wear appropriate footwear (shoes or socks) to protect feet from injury.
- Promote edema control in lower extremities with compression stockings (for venous insufficiency).
- Maintain skin hygiene: keep skin clean and dry, especially in areas prone to moisture (incontinence).
3. Wound Documentation: Maintain thorough and accurate wound documentation:
- Document wound characteristics (size, location, drainage, wound bed, periwound skin) at each dressing change.
- Record wound care interventions (cleansing solutions, dressings applied).
- Document any changes in wound status or healing progress.
- Utilize wound photography as per facility protocol to visually track wound healing over time.
4. Wound Care Clinic Referral: Consider referral to a wound care specialist for complex or chronic wounds:
- Refer patients with chronic, non-healing wounds, or wounds requiring specialized treatments (wound VAC, hyperbaric oxygen therapy) to a wound care clinic for expert assessment and management.
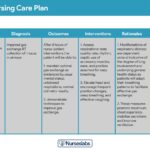
Nursing Care Plans: Addressing Key Nursing Diagnoses for Wound Care
Once a comprehensive assessment is complete, nurses formulate nursing diagnoses to guide care planning. Nursing diagnoses are clinical judgments about individual, family, or community responses to actual and potential health problems and life processes. In wound care, several nursing diagnoses are commonly relevant, providing a framework for addressing patient needs. Here are examples of key nursing diagnoses, along with related factors, defining characteristics, expected outcomes, and nursing interventions.
Acute Pain
Nursing Diagnosis: Acute Pain
Related to:
- Tissue damage from the wound
- Inflammatory process
- Nerve irritation
- Infection
As evidenced by:
- Verbal reports of pain (using pain scale)
- Guarding behavior
- Restlessness, irritability
- Facial grimacing, moaning
- Changes in vital signs (increased heart rate, blood pressure, respiratory rate)
- Tenderness to palpation around the wound
Expected Outcomes:
- Patient will report a pain level of [insert patient-specific goal] or less on a 0-10 pain scale within [specify timeframe].
- Patient will demonstrate effective pain management strategies, both pharmacological and non-pharmacological.
- Patient will be able to participate in wound care activities with minimal pain.
Nursing Assessments:
- Pain Assessment using a Pain Scale: Quantify pain intensity using a standardized pain scale (NRS, VAS) at regular intervals and before/after wound care procedures.
- Pain Characteristics: Assess pain location, quality (sharp, burning, throbbing), onset, duration, aggravating and alleviating factors.
- Palpation for Tenderness: Gently palpate the wound and surrounding tissue to assess for tenderness, which can indicate inflammation or infection.
Nursing Interventions:
- Premedication for Wound Care: Administer prescribed analgesics (oral or IV) 30-60 minutes prior to painful procedures like dressing changes or debridement.
- Pain Management Education: Educate the patient about their pain medication regimen, including dosage, frequency, and potential side effects. Emphasize the importance of taking pain medication as prescribed, even if pain is not severe, to maintain comfort and facilitate healing.
- Non-Pharmacological Pain Relief: Implement non-pharmacological pain management techniques:
- Positioning: Support and elevate the wounded extremity to reduce edema and pressure.
- Distraction: Engage the patient in distracting activities during wound care (music, conversation).
- Relaxation techniques: Teach and encourage relaxation techniques (deep breathing, guided imagery).
- Therapeutic touch or massage (if appropriate and not contraindicated).
- Splinting or Support: Consider splinting or using supportive devices to immobilize the wounded area and minimize movement-related pain.
- Address Contributing Factors: Manage factors that exacerbate pain, such as excessive wound drainage, dryness, edema, or maceration, through appropriate wound care interventions.
Impaired Skin Integrity
Nursing Diagnosis: Impaired Skin Integrity
Related to:
- Physical injury (surgical incision, trauma, pressure, shearing, friction, burns)
- Altered nutritional status
- Impaired circulation
- Moisture (excessive or insufficient)
- Delayed wound healing (comorbidities like diabetes)
As evidenced by:
- Disruption of skin surface (open wound, laceration, abrasion, ulcer)
- Destruction of skin layers (partial-thickness, full-thickness wound)
- Drainage (serous, sanguinous, purulent)
- Redness (erythema)
- Swelling (edema)
- Pain
- Delayed healing
Expected Outcomes:
- Patient will demonstrate progressive wound healing as evidenced by decreased wound size, presence of granulation tissue, and absence of necrotic tissue within [specify timeframe].
- Patient will verbalize understanding of wound care management and preventative measures to promote skin integrity.
- Patient will participate in wound care activities as able.
Nursing Assessments:
- Wound Assessment at Each Dressing Change: Thoroughly assess and document wound characteristics (size, location, depth, drainage, wound bed, periwound skin) at each dressing change to monitor healing progress and identify any deterioration. Utilize the T.I.M.E. framework.
- Wound Classification: Classify the wound type (surgical, pressure ulcer, diabetic foot ulcer, etc.) and stage (if applicable, for pressure ulcers) to guide appropriate care.
- Risk Assessment Tools: Utilize validated risk assessment tools (Braden Scale for pressure ulcer risk) to identify patients at high risk for skin breakdown.
- Wound Culture (If Indicated): Obtain wound cultures if signs of infection are present (purulent drainage, increased redness, warmth, pain).
Nursing Interventions:
- Wound Cleansing and Debridement: Cleanse the wound using appropriate solutions (sterile saline, prescribed cleansers) with each dressing change. Perform debridement as needed to remove nonviable tissue (slough, eschar).
- Appropriate Dressing Application: Select and apply wound dressings based on wound type, exudate level, and healing phase. Utilize dressings that promote a moist wound healing environment, manage exudate, and protect the wound from further trauma and contamination.
- Promote Moist Wound Healing: Maintain a moist wound bed with appropriate dressings to facilitate cell migration, angiogenesis, and collagen synthesis.
- Topical Agents: Apply topical antibiotics or antiseptics as prescribed by the physician or wound care specialist for infected wounds. Use with caution and according to guidelines.
- Manage Wound Healing Stages: Tailor wound care interventions to the specific stage of wound healing, adjusting dressing types and cleansing solutions as needed.
- Wound Moisture Management: Manage wound exudate effectively using appropriate dressings to prevent maceration of periwound skin.
- Suture/Staple Removal: Remove sutures or staples as prescribed, typically within 10-14 days for surgical wounds (earlier for face/scalp wounds).
- Referral to Wound Care Specialist: Refer patients with complex, chronic, or non-healing wounds to a wound care specialist for advanced management.
Ineffective Protection
Nursing Diagnosis: Ineffective Protection
Related to:
- Compromised immune system
- Inadequate primary defenses (broken skin, tissue damage)
- Malnutrition
- Older age
- Immobility
- Incontinence
- Ineffective health self-management
As evidenced by:
- Recurrent infections
- Delayed wound healing
- Pressure ulcer development
- Maladaptive stress response
- Weakness, fatigue
- Neurosensory impairment
- Poor mobility
Expected Outcomes:
- Patient will remain free from developing wound infection during hospitalization or within [specify timeframe].
- Patient will demonstrate protective measures to prevent skin breakdown and infection.
- Patient will verbalize understanding of infection prevention strategies.
Nursing Assessments:
- Vital Signs Monitoring: Monitor vital signs (temperature, heart rate, blood pressure) regularly for signs of systemic infection (fever, tachycardia, hypotension).
- Nutritional Status Assessment: Assess nutritional status, including dietary intake of protein, vitamins, and minerals, and hydration status, as nutrition plays a crucial role in immune function and wound healing.
- ADL Assessment: Assess the patient’s ability to perform activities of daily living (ADLs), particularly mobility and hygiene, as these factors impact skin protection and infection risk.
Nursing Interventions:
- Antibiotic Therapy (If Indicated): Administer prescribed antibiotic therapy for existing infections or as prophylaxis for high-risk wounds, ensuring timely administration and monitoring for effectiveness and side effects.
- Dietary Consultation: Refer the patient to a dietitian for nutritional assessment and development of a meal plan that supports immune function and wound healing, focusing on adequate protein, vitamin, and mineral intake.
- Infection Control Education: Educate the patient and caregivers on infection control measures, including:
- Hand hygiene: Emphasize proper handwashing technique and frequency.
- Wound care techniques: Demonstrate and reinforce correct wound cleansing and dressing change procedures.
- Environmental hygiene: Maintain a clean environment and proper disposal of soiled dressings.
- Signs and symptoms of infection: Instruct on recognizing signs of wound infection (redness, swelling, purulent drainage) and when to seek medical attention.
- Wound Care Provision: Provide appropriate wound care according to established protocols and physician orders, ensuring aseptic or clean technique as indicated.
- Protective Measures: Implement measures to protect the skin and prevent further breakdown:
- Pressure relief: Implement pressure relief strategies for immobile patients (frequent repositioning, pressure-redistributing support surfaces).
- Skin care: Maintain skin hygiene, keep skin clean and dry, and apply barrier creams to protect skin from moisture and irritants.
- Fall prevention: Implement fall prevention measures for patients with mobility impairments.
Ineffective Tissue Perfusion
Nursing Diagnosis: Ineffective Tissue Perfusion (Peripheral)
Related to:
- Interruption of arterial or venous blood flow
- Edema
- Smoking
- Sedentary lifestyle/immobility
- Chronic conditions (diabetes mellitus, peripheral vascular disease, hypertension)
- Insufficient knowledge of comorbidity impact on wound healing
As evidenced by:
- Skin discoloration (pallor, cyanosis, rubor)
- Edema (peripheral)
- Decreased or absent peripheral pulses
- Delayed capillary refill
- Cool skin temperature
- Pain (intermittent claudication, rest pain)
- Paresthesia (numbness, tingling)
- Delayed wound healing in extremities
- Abnormal ankle-brachial index (ABI) or toe-brachial index (TBI)
Expected Outcomes:
- Patient will demonstrate improved peripheral tissue perfusion as evidenced by palpable peripheral pulses, warm and pink extremities, and timely wound healing.
- Patient will verbalize understanding of factors affecting tissue perfusion and strategies to improve circulation.
- Patient will participate in activities to improve circulation as tolerated.
Nursing Assessments:
- Diagnostic Test Review: Monitor results of diagnostic tests assessing peripheral perfusion, such as ABI, TBI, skin perfusion pressure (SPP), and transcutaneous oxygen pressure (TcPO2).
- Signs of Ineffective Perfusion: Assess for clinical signs of ineffective peripheral tissue perfusion in the extremities and wound area: skin color, temperature, peripheral pulses (palpate and compare bilaterally), capillary refill time, edema, pain (claudication, rest pain), paresthesias, and presence of hair loss on legs or feet.
- Comorbidity Assessment: Identify and assess comorbidities that impact peripheral perfusion, such as diabetes mellitus, peripheral vascular disease, hypertension, hyperlipidemia, and smoking history.
Nursing Interventions:
- Foot Care Education: Instruct patients on proper foot care, especially those with diabetes or peripheral vascular disease:
- Daily foot inspection: Encourage daily inspection of feet and legs for blisters, cuts, redness, or any skin abnormalities.
- Proper footwear: Advise wearing well-fitting, protective shoes and socks at all times to prevent injury.
- Avoidance of extreme temperatures: Instruct to avoid soaking feet in hot water or using heating pads, which can cause burns in patients with neuropathy.
- Nail care: Teach proper nail trimming techniques to prevent ingrown toenails.
- Exercise Promotion: Encourage regular exercise, particularly walking, to improve peripheral circulation, unless contraindicated by wound location (e.g., plantar foot ulcer) or other medical conditions. Recommend exercises like ankle circles and seated calf raises if ambulation is limited.
- Positioning:
- Leg elevation: Elevate lower extremities for patients with venous insufficiency to reduce edema and improve venous return.
- Avoid leg elevation for arterial insufficiency: Leg elevation can worsen arterial blood flow; position legs in a dependent position or neutral position as tolerated.
- Smoking Cessation: Strongly emphasize smoking cessation for patients with vascular conditions. Provide resources and support for quitting smoking, as smoking significantly impairs tissue perfusion and wound healing.
- Hyperbaric Oxygen Therapy Referral: Consider referral to a wound care specialist for hyperbaric oxygen therapy (HBOT) for patients with chronic, non-healing wounds and evidence of impaired tissue perfusion. HBOT increases oxygen delivery to tissues, promoting wound healing.
Knowledge Deficit
Nursing Diagnosis: Knowledge Deficit (Wound Care Management)
Related to:
- Lack of exposure to information
- Misinformation
- Lack of recall
- Cognitive limitations
- Language barriers
- Low health literacy
As evidenced by:
- Verbalization of lack of knowledge about wound care
- Requests for information
- Inaccurate follow-through of wound care instructions
- Development of wound infection or worsening wound condition
- Non-adherence to wound care regimen
Expected Outcomes:
- Patient will verbalize understanding of wound care management, including wound cleansing, dressing changes, infection prevention, and signs/symptoms of complications before discharge or within [specify timeframe].
- Patient will demonstrate correct wound care techniques and dressing changes (or caregiver will demonstrate if patient is unable).
- Patient will identify resources for wound care supplies and support.
- Patient will adhere to the prescribed wound care treatment plan.
Nursing Assessments:
- Knowledge Assessment: Assess the patient’s current knowledge and understanding of wound care, wound healing, infection prevention, and prescribed treatment plan. Ask open-ended questions to gauge their understanding and identify knowledge gaps.
- Demonstration of Wound Care: Ask the patient (or caregiver) to demonstrate wound care techniques (cleansing, dressing changes) to assess their practical skills and identify areas needing correction.
- Identify Barriers to Learning: Assess for potential barriers to learning and adherence, such as language barriers, low literacy, cognitive impairments, cultural beliefs, financial constraints, and lack of support systems.
- Resource Assessment: Assess the patient’s access to wound care resources, including financial resources for supplies, transportation to appointments, home healthcare services, and social support.
Nursing Interventions:
- Wound Care Education: Provide comprehensive, individualized education on wound care management, tailored to the patient’s learning needs and abilities. Include:
- Wound cleansing techniques: Demonstrate and explain proper wound cleansing procedures using recommended solutions and techniques.
- Dressing change procedures: Provide step-by-step instructions and demonstrations on how to perform dressing changes correctly, including hand hygiene, aseptic/clean technique, and proper disposal of soiled dressings.
- Infection prevention: Teach infection control measures, such as hand hygiene, avoiding contamination of dressings, and recognizing signs of wound infection.
- Medication education: Explain the purpose, dosage, frequency, and side effects of any prescribed medications (antibiotics, analgesics).
- Wound healing process: Explain the stages of wound healing and factors that promote or hinder healing.
- When to seek medical attention: Instruct on recognizing signs of wound complications (infection, worsening pain, increased drainage) and when to contact their healthcare provider.
- Teach-Back and Return Demonstration: Use teach-back methods to confirm patient understanding. Ask the patient to repeat key information in their own words and demonstrate wound care techniques to ensure competency.
- Involve Caregivers: Include family members or caregivers in education sessions to ensure they are also knowledgeable and capable of providing support and wound care assistance at home.
- Provide Written Materials: Supplement verbal education with written materials, diagrams, and videos in the patient’s preferred language and literacy level to reinforce learning and provide a reference at home.
- Address Misconceptions: Identify and correct any misconceptions or cultural beliefs about wound care practices that may interfere with adherence to the treatment plan.
- Resource Referral: Refer patients to appropriate resources for wound care support:
- Social worker or case manager: For assistance with financial resources, home healthcare arrangements, transportation, and equipment needs.
- Home health nursing: For ongoing wound care management and education in the home setting.
- Dietitian: For nutritional counseling to optimize wound healing.
- Wound care clinic: For specialized wound care services and follow-up.
By utilizing these nursing diagnoses and implementing targeted interventions, nurses can significantly enhance wound care outcomes, promote patient healing, prevent complications, and improve the quality of life for individuals with wounds. Effective nursing diagnosis for wound care is not merely a label but a dynamic tool that guides patient-centered, evidence-based practice in this critical area of healthcare.
References
(Note: As the original article did not provide specific references, for a real-world article, you would include a list of credible sources here. For this exercise, we will omit them as per the instructions to focus on rewriting the content based on the provided source.)