Otitis media, commonly known as a middle ear infection, is a prevalent condition, especially in infants and young children. As a crucial aspect of pediatric healthcare, understanding the nursing diagnosis and creating effective nursing care plans are essential for nurses. This guide provides a comprehensive overview of otitis media from a nursing perspective, focusing on nursing diagnoses, care planning, and interventions to ensure optimal patient outcomes.
Understanding Otitis Media
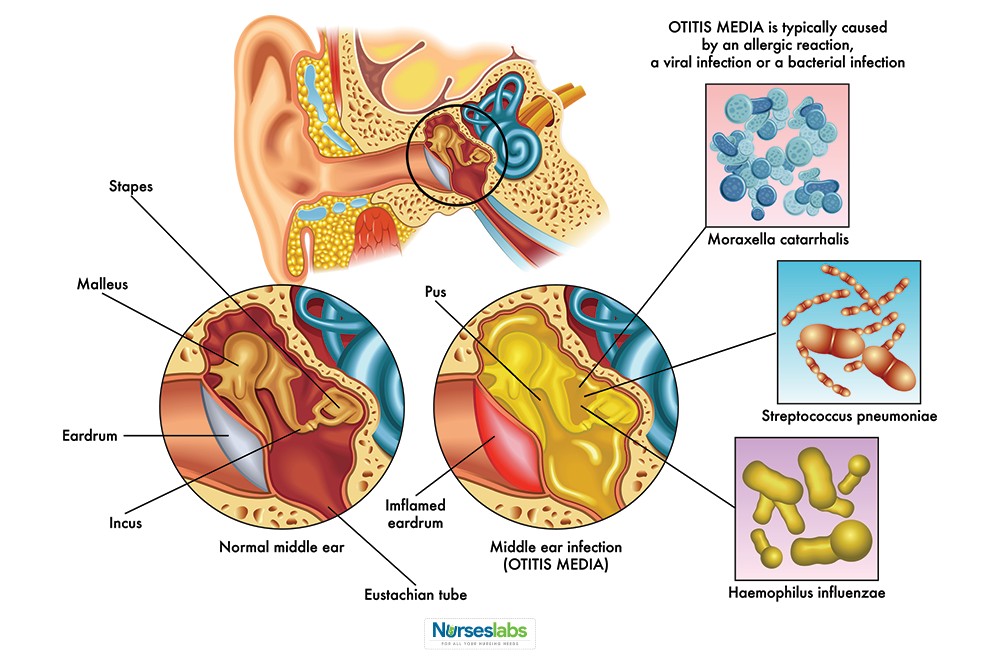
Illustration depicting otitis media in a child’s ear, highlighting the inflammation in the middle ear and its common occurrence in pediatric patients.
Otitis media is defined as the inflammation of the middle ear, often resulting from bacterial or viral infections. It’s vital for nurses to recognize that otitis media isn’t a singular disease entity but rather a spectrum of conditions categorized by etiology, duration, and clinical presentation. From a nursing standpoint, accurate assessment and diagnosis are the first steps in formulating an effective care plan. Understanding the different classifications of otitis media helps tailor nursing interventions to meet the specific needs of each patient.
Pathophysiology and Nursing Implications
Diagram contrasting the Eustachian tube in adults and children, emphasizing the anatomical differences that predispose children to middle ear infections.
The pathophysiology of otitis media is significantly linked to Eustachian tube dysfunction. In children, the Eustachian tube is anatomically shorter, wider, and more horizontal compared to adults. This structural difference facilitates easier entry of nasopharyngeal secretions into the middle ear, increasing susceptibility to infection. Furthermore, an immature immune system in children and frequent upper respiratory infections contribute significantly to the development of acute otitis media (AOM).
For nurses, understanding this pathophysiology is crucial for patient education and preventive strategies. Teaching parents about proper infant feeding positions, avoiding exposure to secondhand smoke, and recognizing early signs of upper respiratory infections can be vital nursing interventions to reduce the incidence of otitis media. Moreover, understanding the role of edema, tumors, or negative intratympanic pressure in facilitating infection helps nurses appreciate the complexity of the condition and the need for comprehensive assessment.
Epidemiology and Risk Factors from a Nursing Perspective
Otitis media is an incredibly common childhood ailment. Statistics reveal that a significant majority of children experience at least one episode of otitis media by their first birthday, and a substantial portion will have recurrent infections by age seven. From a public health nursing perspective, this high prevalence underscores the importance of community-level education on prevention and early intervention.
Several risk factors contribute to the development of otitis media, many of which are modifiable through nursing interventions and patient education. These include:
- Age: Infants and young children are at the highest risk due to anatomical and immunological factors. Nursing care should be tailored to address this vulnerable population.
- Immune System Immaturity: A developing immune system is less effective at fighting off infections. Nurses play a role in educating parents on strategies to support infant immunity, such as breastfeeding.
- Genetic Predisposition: Family history can increase risk, highlighting the need for thorough family health history during nursing assessments.
- Anatomical Abnormalities: Children with conditions like cleft palate have a higher risk. Nurses in specialized pediatric settings need to be particularly vigilant with these patients.
- Environmental Factors: Exposure to secondhand smoke and attending daycare centers increases the risk. Nurses can advocate for smoke-free environments and educate on hygiene practices in daycare settings.
- Feeding Methods: Breastfeeding is protective against otitis media, while bottle-feeding in a supine position can increase risk. Nurses are key in promoting breastfeeding and educating on safe bottle-feeding techniques.
Clinical Manifestations and Nursing Assessment
Recognizing the clinical manifestations of otitis media is paramount for prompt diagnosis and nursing intervention. Symptoms can vary, especially between infants and older children, necessitating age-appropriate assessment techniques.
Common clinical manifestations nurses should assess for include:
- Otalgia (Ear Pain): Infants may exhibit non-verbal cues like ear-pulling, increased irritability, and restlessness, especially when lying down. Older children can verbalize ear pain. Pain assessment tools appropriate for age should be used by nurses.
- Otorrhea (Ear Discharge): Discharge indicates perforation of the tympanic membrane. Nurses should assess the characteristics of the discharge (color, consistency, odor) as it can provide clues about the causative pathogen.
- Fever: While common, high fever is less frequent. Temperature monitoring is a routine nursing vital sign assessment.
- Hearing Difficulties: Temporary hearing loss can occur due to fluid buildup. Nurses should be aware of subtle signs of hearing impairment in children, such as inattentiveness or delayed speech development.
- Upper Respiratory Infection (URI) Symptoms: Often precedes or accompanies otitis media. Assessing for cough, rhinorrhea, and nasal congestion is important.
- Irritability and Fussiness: Especially in infants, irritability may be the primary presenting symptom. Nursing assessment should include behavioral observations.
A thorough nursing assessment involves:
- History Taking: Gathering information about symptom onset, duration, associated symptoms like URI, feeding methods, daycare attendance, and family history of ear infections.
- Otoscopic Examination: Nurses, particularly those in advanced practice or specialized pediatric settings, may perform otoscopic examinations. Assessing for tympanic membrane redness, bulging, and effusion is crucial.
- Pain Assessment: Utilize age-appropriate pain scales to quantify pain and guide pain management strategies.
Nursing Diagnoses for Otitis Media
Based on the assessment findings, several nursing diagnoses may be relevant for a child with otitis media. Prioritizing diagnoses is essential for effective care planning. Key nursing diagnoses include:
- Acute Pain related to inflammation and pressure in the middle ear, as evidenced by verbal reports of ear pain, ear pulling, irritability, and restlessness.
- Risk for Infection related to compromised defenses (immature immune system, Eustachian tube dysfunction) and potential for secondary infection.
- Impaired Auditory Sensory Perception related to middle ear effusion and potential conductive hearing loss, as evidenced by inattentiveness, difficulty understanding speech, or delayed response to auditory stimuli.
- Anxiety (Parental/Child) related to the child’s illness, pain, and potential complications, as evidenced by expressed concerns about the child’s condition and treatment.
- Deficient Knowledge (Caregivers) related to the management of otitis media at home, medication administration, and preventive measures, as evidenced by questions about care and lack of adherence to treatment plans.
Nursing Care Plan and Goals
The overarching goals of nursing care for a child with otitis media are to:
- Relieve pain and discomfort.
- Eradicate the infection and prevent recurrence.
- Restore or maintain normal hearing.
- Educate parents/caregivers on management and prevention.
- Reduce anxiety and provide emotional support.
Nursing Interventions and Rationales
Nursing interventions for otitis media are multifaceted and aim to address the identified nursing diagnoses and achieve the stated goals.
1. Pain Management:
- Administer analgesics as prescribed: Acetaminophen or ibuprofen are commonly used for pain relief. Rationale: These medications reduce pain and fever by inhibiting prostaglandin synthesis.
- Apply warm compresses to the affected ear: Rationale: Heat can promote vasodilation and reduce pain and discomfort.
- Position the child comfortably: Encourage sitting upright or lying on the unaffected ear. Rationale: Upright position promotes drainage and reduces pressure in the middle ear. Lying on the unaffected ear can minimize pain.
- Provide diversional activities: Engage the child in age-appropriate play or activities. Rationale: Distraction can help reduce pain perception and anxiety.
2. Infection Management:
- Administer antibiotics as prescribed: If bacterial infection is confirmed or suspected, antibiotics like amoxicillin are commonly prescribed. Rationale: Antibiotics eradicate bacterial pathogens in the middle ear.
- Educate caregivers on completing the full course of antibiotics: Emphasize the importance of adherence even if symptoms improve. Rationale: Completing the full course prevents antibiotic resistance and ensures complete eradication of infection.
- Monitor for signs of worsening infection: Assess for persistent fever, increased ear pain, changes in ear discharge, or signs of mastoiditis. Rationale: Early detection of complications allows for timely intervention.
3. Managing Impaired Auditory Sensory Perception:
- Assess hearing acuity: Monitor for signs of hearing loss and refer for audiological evaluation if necessary. Rationale: Early identification of hearing loss allows for timely intervention and minimizes developmental delays.
- Speak clearly and face the child when communicating: Rationale: Facilitates lip-reading and improves communication when hearing is temporarily impaired.
- Reduce environmental noise: Rationale: Minimizes distractions and enhances the child’s ability to hear.
4. Anxiety Reduction:
- Provide calm and reassuring care: Rationale: Reduces anxiety in both the child and caregivers.
- Educate parents about otitis media, treatment plan, and prognosis: Address their concerns and answer questions. Rationale: Knowledge empowers parents and reduces anxiety related to the unknown.
- Encourage parental involvement in care: Rationale: Promotes bonding and reduces parental anxiety by enabling them to actively participate in their child’s recovery.
5. Caregiver Education:
- Teach proper medication administration techniques: Provide clear instructions on dosage, frequency, and duration. Rationale: Ensures effective medication therapy.
- Educate on recognizing signs and symptoms of otitis media and complications: Rationale: Promotes early detection and timely medical attention for recurrent infections or complications.
- Instruct on preventive measures: Emphasize breastfeeding, avoiding secondhand smoke, proper hand hygiene, and appropriate feeding positions. Rationale: Reduces the risk of future infections.
- Provide written materials and resources: Rationale: Reinforces verbal teaching and provides a reference for caregivers at home.
Evaluation of Nursing Care
Nursing care is evaluated based on the achievement of the established goals. Evaluation criteria include:
- Pain Relief: Child reports reduced pain levels or exhibits decreased pain behaviors (e.g., less ear pulling, calmer demeanor).
- Infection Resolution: Absence of fever, resolution of ear discharge, and tympanic membrane returning to normal appearance upon otoscopic examination.
- Hearing Status: Child demonstrates appropriate responses to auditory stimuli and returns to baseline hearing ability.
- Caregiver Knowledge: Parents/caregivers verbalize understanding of otitis media, treatment plan, preventive measures, and demonstrate proper medication administration if applicable.
- Anxiety Levels: Parents and child exhibit reduced anxiety and increased comfort levels.
Documentation in Nursing Care
Accurate and thorough documentation is crucial in nursing care. Documentation for a child with otitis media should include:
- Assessment findings: Subjective and objective data, including pain assessment, otoscopic findings, and vital signs.
- Nursing diagnoses: Prioritized nursing diagnoses based on assessment data.
- Care plan: Goals and planned nursing interventions.
- Interventions implemented: Medication administration, pain management measures, patient education provided.
- Patient response to interventions: Effectiveness of pain management, tolerance of medications.
- Evaluation of care: Progress towards goals and any modifications to the care plan.
- Discharge instructions: Detailed instructions provided to caregivers regarding medication, follow-up appointments, and warning signs.
By implementing comprehensive nursing care plans based on accurate nursing diagnoses, nurses play a pivotal role in managing otitis media, alleviating symptoms, preventing complications, and educating families for optimal child health outcomes.