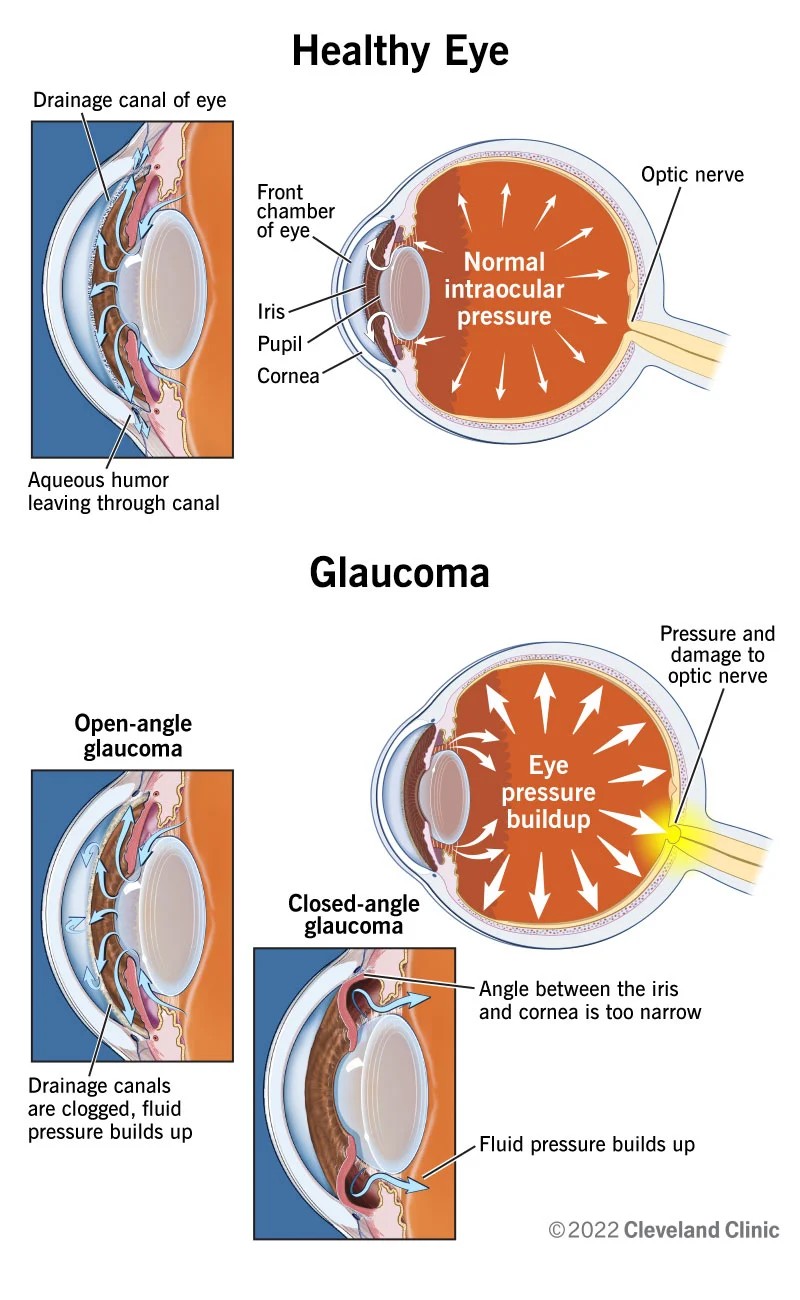
 Understanding Glaucoma: Visual representation of optic nerve damage and increased intraocular pressure in glaucoma patients, highlighting key nursing diagnosis considerations.
Understanding Glaucoma: Visual representation of optic nerve damage and increased intraocular pressure in glaucoma patients, highlighting key nursing diagnosis considerations.
Introduction
Glaucoma, a progressive optic neuropathy, stands as a leading cause of irreversible blindness globally. Characterized by damage to the optic nerve, often due to elevated intraocular pressure (IOP), glaucoma necessitates vigilant and comprehensive nursing care. For nurses, understanding the nuances of “Nursing Diagnosis On Glaucoma” is paramount to delivering effective patient care, preventing vision loss, and enhancing the quality of life for individuals affected by this condition. This guide aims to provide an in-depth exploration of nursing diagnoses relevant to glaucoma, empowering nurses to formulate robust care plans and implement evidence-based interventions.
Patient Assessment for Glaucoma Nursing Diagnosis
A thorough patient assessment is the cornerstone of accurate nursing diagnosis and effective care planning for glaucoma. This assessment encompasses both subjective and objective data collection to provide a holistic understanding of the patient’s condition and needs.
Subjective Assessment Data:
Gathering subjective data involves eliciting information directly from the patient regarding their experience with glaucoma. Key areas to explore include:
- Symptomology: Patients may report a spectrum of visual disturbances, ranging from subtle blurred vision or halos around lights to more pronounced eye pain, headaches, or tunnel vision in advanced stages. However, it’s crucial to note that primary open-angle glaucoma, the most common form, is often asymptomatic in its early stages, underscoring the importance of routine eye exams.
- Impact on Daily Life: Inquire about how glaucoma symptoms, or the diagnosis itself, are affecting the patient’s daily activities. This includes difficulties with reading, driving, mobility, and performing self-care tasks. Understanding these limitations is vital for tailoring interventions to maintain independence and safety.
- Psychosocial Concerns: Glaucoma diagnosis can evoke significant anxiety and fear related to potential vision loss and its implications for their future. Patients may express concerns about their ability to work, maintain their lifestyle, or care for themselves and their families. Assessing their emotional state and support systems is essential for addressing these psychosocial needs.
- Knowledge of Glaucoma and Treatment: Evaluate the patient’s understanding of glaucoma, its causes, progression, and treatment modalities. Identify any knowledge gaps that need to be addressed through patient education.
Objective Assessment Data:
Objective data is derived from clinical examinations and diagnostic tests, providing measurable indicators of the patient’s glaucoma status. Key objective data points include:
- Intraocular Pressure (IOP) Measurement: Tonometry is used to measure IOP, a primary risk factor for glaucoma. Document the IOP readings and note the target IOP range recommended by the ophthalmologist.
- Visual Field Testing (Perimetry): Perimetry assesses peripheral vision and identifies any visual field defects characteristic of glaucoma. Document the results of visual field tests, noting any progression of visual field loss.
- Optic Nerve Head Assessment: Ophthalmoscopy or imaging techniques like Optical Coherence Tomography (OCT) are used to examine the optic nerve head for signs of glaucomatous damage, such as cupping or nerve fiber layer thinning. Document findings from optic nerve evaluations.
- Gonioscopy: This examination determines the angle between the iris and cornea, crucial for classifying the type of glaucoma (open-angle vs. angle-closure).
- Medical History Review: Review the patient’s medical history for pre-existing conditions (e.g., diabetes, hypertension, myopia) and medications that may influence glaucoma risk or management.
Common Nursing Diagnoses Related to Glaucoma
Based on the comprehensive assessment data, several nursing diagnoses may be pertinent for patients with glaucoma. These diagnoses provide a framework for planning and implementing targeted nursing interventions. Key nursing diagnoses include:
- Impaired Visual Sensory/Perception Function related to optic nerve damage secondary to increased intraocular pressure. This diagnosis addresses the core physiological impact of glaucoma on vision.
- Risk for Injury related to visual field deficits and impaired depth perception. Glaucoma-related vision loss, particularly peripheral vision loss, increases the risk of falls and accidents.
- Deficient Knowledge related to glaucoma disease process, treatment regimen, and self-management techniques. Effective glaucoma management relies heavily on patient understanding and adherence to treatment plans.
- Anxiety related to glaucoma diagnosis, potential for vision loss, and impact on lifestyle. The progressive nature of glaucoma and the threat of blindness can induce significant anxiety.
- Ineffective Health Management related to complexity of treatment regimen and lack of understanding of disease process. Managing glaucoma often involves long-term medication use and lifestyle modifications, which can be challenging for some patients.
Nursing Interventions for Glaucoma
Nursing interventions are tailored to address the identified nursing diagnoses and promote optimal patient outcomes. These interventions encompass a range of actions, including monitoring, medication administration, education, and emotional support.
For Impaired Visual Function:
- Regular Visual Acuity and Visual Field Assessments: Monitor visual function at regular intervals to detect any changes or progression of visual impairment.
- Medication Management: Administer prescribed eye drops accurately and consistently, adhering to the prescribed dosage and frequency. Educate patients on proper eye drop instillation techniques.
- Collaboration with Ophthalmology: Work closely with the ophthalmology team to ensure timely medical and surgical interventions to manage IOP and preserve vision.
- Assistive Devices and Strategies: Introduce and educate patients on the use of low vision aids, such as magnifiers or large-print materials, to optimize remaining vision.
- Environmental Modifications: Recommend modifications to the home environment to enhance safety and visual accessibility, such as improved lighting and reduced clutter.
For Risk for Injury:
- Fall Risk Assessment: Conduct thorough fall risk assessments, considering visual field deficits, mobility, and environmental hazards.
- Safety Education: Educate patients and families on fall prevention strategies, including home safety modifications, proper footwear, and using assistive devices like canes or walkers if needed.
- Environmental Safety Measures: Implement safety measures in healthcare settings, such as clear pathways, adequate lighting, and handrails, to minimize fall risks.
- Referral to Occupational Therapy: Consider referrals to occupational therapy for comprehensive home safety evaluations and adaptive equipment recommendations.
For Deficient Knowledge:
- Glaucoma Education: Provide comprehensive education on glaucoma, covering the disease process, risk factors, treatment options (medications, laser therapy, surgery), and the importance of adherence to treatment.
- Medication Education: Thoroughly educate patients on their prescribed eye medications, including the name, purpose, dosage, administration technique, potential side effects, and importance of consistent use.
- Self-Management Education: Teach patients self-monitoring techniques, such as recognizing signs and symptoms that warrant prompt medical attention, and strategies for managing daily activities with vision impairment.
- Resource Provision: Provide patients with written materials, online resources, and referrals to glaucoma support groups and organizations to enhance their understanding and access ongoing support.
For Anxiety:
- Therapeutic Communication: Establish a trusting and supportive nurse-patient relationship. Utilize active listening and empathy to allow patients to express their fears and concerns about vision loss.
- Emotional Support and Reassurance: Provide emotional support and reassurance, acknowledging the patient’s anxieties and validating their feelings. Offer realistic hope and emphasize the importance of proactive management to preserve vision.
- Information and Education: Provide clear and accurate information about glaucoma and its management to reduce uncertainty and anxiety related to the unknown.
- Stress Reduction Techniques: Introduce and encourage stress-reducing activities, such as relaxation techniques, deep breathing exercises, or mindfulness practices.
- Referral for Counseling: If anxiety is severe or impacting the patient’s ability to cope, consider referral to mental health professionals or counseling services.
For Ineffective Health Management:
- Assess Barriers to Adherence: Identify factors that may hinder the patient’s ability to adhere to the treatment regimen, such as complexity of medication schedule, forgetfulness, physical limitations, cost, or lack of understanding.
- Simplify Treatment Regimen: Collaborate with the healthcare team to simplify the treatment regimen whenever possible, such as using combination eye drops or simplifying the medication schedule.
- Memory Aids and Reminders: Suggest memory aids, such as medication organizers, alarms, or reminder apps, to improve medication adherence.
- Ongoing Support and Follow-up: Provide ongoing support and regular follow-up to monitor adherence, address any challenges, and reinforce the importance of consistent glaucoma management.
Glaucoma Nursing Evaluation
Evaluation is an ongoing process to assess the effectiveness of nursing interventions and make necessary adjustments to the care plan. Evaluation criteria should be specific, measurable, achievable, relevant, and time-bound (SMART). Expected outcomes for patients with glaucoma may include:
- Stable or Improved Visual Function: Maintenance of visual acuity and visual fields within acceptable parameters for the individual patient, as determined by ophthalmological assessments.
- Absence of Injury: Patient remains free from falls and eye injuries related to visual impairment.
- Adequate Knowledge of Glaucoma: Patient demonstrates understanding of glaucoma, its treatment, and self-management strategies through verbalization and appropriate self-care behaviors.
- Reduced Anxiety Levels: Patient reports reduced anxiety and demonstrates effective coping mechanisms in managing emotional distress related to glaucoma.
- Effective Health Management: Patient adheres to the prescribed treatment regimen, including medication administration and follow-up appointments, and actively participates in self-management activities.
Documentation in Glaucoma Nursing Care
Accurate and comprehensive documentation is crucial in glaucoma nursing care. Documentation should include:
- Subjective and objective assessment data
- Nursing diagnoses identified
- Nursing interventions implemented
- Patient responses to interventions
- Evaluation of patient outcomes
- Communication with the interdisciplinary healthcare team
- Patient education provided
Regularly review and update the nursing care plan based on ongoing assessments and evaluations to ensure it remains relevant and responsive to the patient’s evolving needs.
Disclaimer: This nursing care plan guide provides general information and should not replace professional medical advice. Always consult with qualified healthcare professionals for individualized patient care plans and treatment recommendations.