Caring for patients with respiratory issues requires a thorough understanding of assessment and accurate nursing diagnoses. This guide expands upon the essential concepts of oxygenation and hypoxia to provide a detailed overview of how nurses utilize the nursing process to effectively care for clients experiencing alterations in oxygenation, focusing specifically on nursing diagnoses on respiratory system dysfunction.
Respiratory System Assessment: Subjective and Objective Data Collection
A comprehensive assessment of a client’s respiratory status is crucial for identifying appropriate nursing diagnoses and interventions. This assessment encompasses both subjective and objective data collection.
Subjective Respiratory Assessment: Gathering Patient Perspectives
Subjective assessment relies on the patient’s self-reported experiences and symptoms. Dyspnea, the clinical term for shortness of breath, is a primary subjective symptom. It’s vital to quantify the patient’s dyspnea using a standardized scale, such as a 0-10 rating, allowing for consistent monitoring and comparison over time, similar to pain assessment. This subjective feeling can significantly impact a patient’s quality of life, and understanding its severity is the first step in effective management.
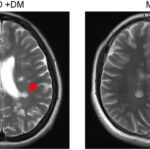
Cough is another critical symptom to investigate. If present, detailed questioning is needed to determine characteristics such as frequency, timing (day or night), and whether it is productive or non-productive. Productive coughs involve sputum expectoration. Sputum, a mixture of mucus and other respiratory secretions, should be further assessed for color, consistency, odor, and amount. Changes in sputum characteristics can indicate various underlying conditions. For instance, purulent sputum, often yellow, green, or brown, is typically associated with respiratory infections, signaling the presence of bacteria or inflammatory processes.
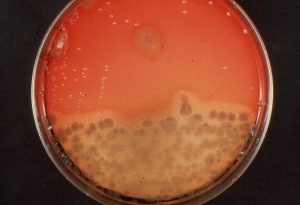
Figure 8.7 Purulent Sputum
Chest pain is a significant symptom that requires careful evaluation. When a patient reports chest pain, it is paramount to initially rule out cardiac emergencies. Questions to immediately assess for emergency conditions include:
- “Does the pain feel like pressure, tightness, or squeezing?”
- “Does the pain radiate to your jaw, arm, back, or shoulder?”
- “Are you experiencing shortness of breath, dizziness, nausea, or sweating alongside the pain?”
Positive responses to these questions necessitate immediate emergency medical intervention. If cardiac causes are less likely, a focused respiratory assessment of chest pain should be conducted, exploring onset, location, duration, character (sharp, dull, aching), aggravating and alleviating factors (e.g., coughing, deep breathing, position), radiation, and any self-treatment measures taken. Pleuritic chest pain, often associated with respiratory conditions, typically worsens with coughing or deep inspiration.
Objective Respiratory Assessment: Clinical Signs and Examination
Objective assessment involves observable and measurable data obtained through physical examination and diagnostic testing. Key objective assessments for respiratory function include:
- Airway Assessment: Ensuring a patent airway is the priority. Assess for any obstructions, such as foreign bodies, secretions, or swelling.
- Respiratory Rate, Effort, and Quality: Observe the rate, depth, and rhythm of respirations. Note any signs of labored breathing, such as nasal flaring, accessory muscle use (sternocleidomastoid, abdominal), or intercostal retractions. Assess the quality of breathing – is it shallow, deep, or normal?
- Pulse Oximetry: Measure peripheral oxygen saturation (SpO2) to estimate the percentage of hemoglobin saturated with oxygen. Note any deviations from the normal range (typically 95-100% in healthy adults).
- Lung Auscultation: Using a stethoscope, listen to breath sounds in all lung fields. Identify normal breath sounds (vesicular, bronchovesicular, bronchial) and adventitious (abnormal) sounds such as wheezes, crackles (rales), rhonchi, or pleural rubs. These sounds provide clues about underlying pathology.
- Heart Rate: Monitor heart rate for tachycardia, which can be an early sign of hypoxia as the body attempts to compensate for decreased oxygen levels.
Visual inspection should also include observing for cyanosis, a bluish discoloration of the skin and mucous membranes indicating hypoxemia, and clubbing of the fingers. Clubbing, a bulbous enlargement of the distal phalanges, is a sign of chronic hypoxia, often seen in conditions like COPD or congenital heart defects.
Figure 8.8 Clubbing of Fingertips
Another objective sign associated with chronic respiratory disease, particularly COPD, is barrel chest. This refers to an increased anterior-posterior diameter of the chest, giving it a rounded, barrel-like appearance. Barrel chest develops due to chronic air trapping in the alveoli, leading to lung hyperinflation.
Figure 8.9 Comparison of Chest with Normal Anterior/Posterior Diameter (A) to a Barrel Chest(B)
Diagnostic Tests and Laboratory Findings for Respiratory Issues
Diagnostic tests and laboratory studies are essential to confirm suspected diagnoses and guide treatment. The choice of tests depends on the patient’s clinical presentation and suspected underlying condition.
- Chest X-ray: A common and readily available imaging technique that provides valuable information about the lungs, heart, and chest wall. Chest X-rays can detect pneumonia, pneumothorax, pleural effusions, lung masses, and cardiac enlargement. They are crucial for diagnosing and monitoring various respiratory and cardiac conditions. However, chest X-rays are contraindicated in pregnancy unless absolutely necessary.
Figure 8.10 Chest X-ray
- Sputum Culture: Indicated for patients with productive coughs, especially when infection is suspected. Sputum culture identifies the type of bacteria or fungi present in the sputum, guiding appropriate antibiotic or antifungal therapy. Gram stain and sensitivity testing are typically performed to further refine antimicrobial selection.
Figure 8.11 Sputum Culture
- Arterial Blood Gas (ABG) Analysis: Considered the gold standard for assessing oxygenation and acid-base balance. ABGs directly measure partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2), pH, bicarbonate (HCO3-), and oxygen saturation (SaO2). ABGs are crucial in patients with respiratory distress, acute respiratory failure, and for managing patients on mechanical ventilation.
Table 8.3a Normal Ranges of ABG Values in Adults
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |




Common Nursing Diagnoses Related to Respiratory Dysfunction
Based on the assessment findings, nurses formulate nursing diagnoses on respiratory system problems. NANDA-I (North American Nursing Diagnosis Association International) provides standardized nursing diagnoses. Commonly used diagnoses for patients with oxygenation alterations and dyspnea include:
-
Impaired Gas Exchange: This diagnosis is used when a patient experiences an imbalance between oxygen uptake and carbon dioxide elimination at the alveolar-capillary membrane. Defining characteristics include abnormal ABGs, cyanosis, altered respiratory rate or depth, bradypnea, confusion, hypercapnia, hypoxemia, irritability, nasal flaring, agitation, tachycardia, tachypnea, and somnolence.
-
Ineffective Breathing Pattern: This diagnosis applies when the patient’s spontaneous breathing pattern is inadequate to provide sufficient ventilation. Defining characteristics include altered breathing pattern, bradypnea, cyanosis, dyspnea, hypercapnia, hyperventilation, hypoventilation, increased anterior-posterior chest diameter, nasal flaring, orthopnea, pursed-lip breathing, tachypnea, accessory muscle use, and three-point positioning.
-
Ineffective Airway Clearance: This diagnosis is used when a patient is unable to clear secretions or obstructions from the respiratory tract to maintain a clear airway. Defining characteristics include absent or ineffective cough, adventitious breath sounds, altered respiratory rhythm, bradypnea, excessive sputum, inability to remove airway secretions, orthopnea, restlessness, and accessory muscle use.
-
Decreased Cardiac Output: While primarily a cardiac diagnosis, decreased cardiac output can significantly impact oxygenation. The heart’s ability to pump oxygenated blood to tissues directly affects oxygen delivery. Defining characteristics relevant to respiratory care include adventitious breath sounds (due to fluid overload), abnormal skin color (cyanosis, pallor), tachycardia, fatigue, and edema.
-
Activity Intolerance: Impaired oxygenation often leads to decreased energy and inability to tolerate activity. Defining characteristics include exertional dyspnea, reported fatigue, abnormal heart rate or blood pressure response to activity, and generalized weakness.
Table 8.3b NANDA-I Nursing Diagnoses Related to Decreased Oxygenation and Dyspnea
| NANDA-I Nursing Diagnoses | Definition | Selected Defining Characteristics |
|---|---|---|
| Impaired Gas Exchange | Excess or deficit in oxygenation and/or carbon dioxide elimination | Abnormal arterial pH, Abnormal skin color, Altered respiratory depth or rhythm, Bradypnea, Confusion, Hypercapnia, Hypoxia or hypoxemia, Irritable mood, Nasal flaring, Psychomotor agitation, Tachycardia, Tachypnea, Somnolence |
| Ineffective Breathing Pattern | Inspiration and/or expiration that does not provide adequate ventilation. | Abnormal breathing pattern, Bradypnea, Cyanosis, Dyspnea, Hypercapnia, Hyperventilation, Hypoventilation, Increased anterior-posterior chest diameter, Nasal flaring, Orthopnea, Pursed-lip breathing, Tachypnea, Uses accessory muscles to breathe, Uses three-point positioning |
| Ineffective Airway Clearance | Reduced ability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. | Absence of cough, Adventitious breath sounds, Altered respiratory rhythm, Bradypnea, Excessive sputum, Ineffective sputum elimination, Orthopnea, Psychomotor agitation, Uses accessory muscles to breath |
| Decreased Cardiac Output | Inadequate volume of blood pumped by the heart to meet the metabolic demands of the body. | Anxiety, Bradycardia, Adventitious breath sounds, Abnormal skin color, Tachycardia, Psychomotor agitation, Fatigue, Edema, Weight gain, Decreased peripheral pulses |
| Decreased Activity Tolerance | Insufficient endurance to complete required or desired daily activities. | Exertional dyspnea, Expresses fatigue, Abnormal heart rate or blood pressure response to activity, Generalized weakness |
For example, a patient with COPD presenting with dyspnea, barrel chest, nasal flaring, orthopnea, prolonged expiration, pursed-lip breathing, tachypnea, and accessory muscle use would likely have the nursing diagnosis of Ineffective Breathing Pattern. The nurse validates this diagnosis by matching the patient’s assessment findings with the defining characteristics of the diagnosis.
Outcome Identification: Setting SMART Goals for Respiratory Care
Once nursing diagnoses are established, the next step is outcome identification. A broad goal for patients with altered oxygenation is: The patient will demonstrate adequate movement of air into and out of the lungs.
SMART (Specific, Measurable, Achievable, Relevant, Time-bound) outcomes provide more specific and measurable targets. For a patient with dyspnea, a SMART outcome could be: The patient will report dyspnea within their desired range of 1-2 on a 0-10 scale throughout their hospital stay.
Planning and Implementing Nursing Interventions for Respiratory Issues
Nursing interventions are planned and implemented to achieve the desired patient outcomes. Common nursing interventions for patients with respiratory dysfunction fall into categories such as Anxiety Reduction and Respiratory Monitoring.
-
Anxiety Reduction: Dyspnea can be a frightening experience, exacerbating anxiety. Anxiety reduction interventions aim to minimize fear and promote relaxation. These include:
- Using a calm and reassuring approach.
- Providing clear explanations of procedures and sensations.
- Seeking to understand the patient’s perspective and concerns.
- Providing information about diagnosis, treatment, and prognosis.
- Staying with the patient during periods of acute distress.
- Encouraging family support.
- Active listening and creating a trusting environment.
- Encouraging verbalization of feelings.
- Identifying anxiety level changes.
- Providing diversional activities.
- Teaching relaxation techniques (guided imagery, music therapy, etc.).
- Administering anxiolytic medications as prescribed.
-
Respiratory Monitoring: Continuous and intermittent monitoring is crucial to detect changes in respiratory status and evaluate intervention effectiveness. Respiratory monitoring interventions include:
- Monitoring respiratory rate, rhythm, depth, and effort.
- Observing chest movement for symmetry, accessory muscle use, and retractions.
- Monitoring for abnormal breath sounds (snoring, stridor).
- Identifying abnormal breathing patterns (bradypnea, tachypnea, hyperventilation, Cheyne-Stokes).
- Continuous pulse oximetry monitoring, especially in at-risk patients.
- Auscultating lung sounds for adventitious sounds or decreased ventilation.
- Assessing cough effectiveness and sputum characteristics.
- Determining the need for suctioning.
- Frequent monitoring of at-risk patients.
- Monitoring for dyspnea and its triggers.
- Reviewing chest X-ray and ABG results and reporting changes to the provider.
- Initiating resuscitation efforts when needed.
- Implementing respiratory therapy treatments (nebulizers, etc.).
Beyond these independent nursing interventions, managing hypoxia involves specific actions such as:
- Teaching and encouraging deep breathing and coughing exercises.
- Repositioning patients to optimize lung expansion (e.g., high Fowler’s, prone positioning).
- Managing oxygen therapy (delivery device, flow rate, monitoring response).
- Administering respiratory medications (bronchodilators, corticosteroids, etc.).
- Performing airway suctioning to remove secretions.
Patient education is also vital for long-term respiratory health. Health promotion teaching includes:
- Annual influenza vaccination.
- Pneumococcal vaccination as recommended.
- Smoking cessation.
- Adequate fluid intake to thin secretions.
- Regular physical activity within tolerance.
Evaluation of Nursing Interventions for Respiratory Status
The final step of the nursing process is evaluation. After implementing interventions, it’s essential to evaluate their effectiveness in achieving the desired outcomes. This involves reassessing the patient’s respiratory status, including:
- Heart rate.
- Respiratory rate.
- Pulse oximetry.
- Lung sounds.
- Patient-reported dyspnea level.
Documentation of intervention effectiveness and overall care plan evaluation are crucial for ongoing patient management and quality improvement.
Definition of Terms:
Sputum: Mucus and other secretions expelled from the mouth after being coughed up from the respiratory tract.
Purulent Sputum: Sputum that is yellow, green, or brown in color, often indicative of respiratory infection due to the presence of white blood cells and bacteria.
Clubbing: Abnormal enlargement of the distal fingers and toes due to chronic hypoxemia.
Barrel Chest: Increased anterior-posterior diameter of the chest, often associated with chronic air trapping in conditions like COPD.
Bradypnea: Abnormally slow respiratory rate, below the age-appropriate normal range.
Tachypnea: Abnormally rapid respiratory rate, exceeding the age-appropriate normal range.
Orthopnea: Shortness of breath that occurs in the supine position and is relieved by sitting or standing upright.