Effective respiratory function is paramount to overall health, and nurses play a vital role in identifying and managing respiratory issues. Understanding Nursing Diagnosis Respiratory conditions is essential for providing optimal patient care. This article will explore the nursing process as it applies to patients experiencing respiratory distress, focusing on assessment, diagnosis, planning, intervention, and evaluation.
Respiratory Assessment: Subjective and Objective Data Collection
A thorough respiratory assessment is the cornerstone of identifying and addressing oxygenation problems. This assessment includes both subjective and objective data collection to provide a complete picture of the patient’s respiratory status.
Subjective Respiratory Assessment
Subjective assessment relies on the patient’s description of their symptoms. Dyspnea, or shortness of breath, is a primary symptom. It is crucial to quantify the patient’s dyspnea using a scale of 0 to 10, similar to a pain scale. This allows for a standardized and trackable measurement of their breathing difficulty.[^1] Understanding the severity of dyspnea is vital as it significantly impacts a patient’s quality of life and ability to perform daily activities.
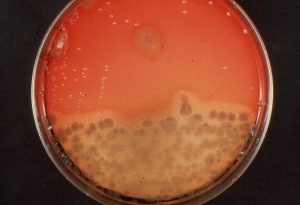
Cough is another significant symptom to evaluate. When assessing a cough, determine if it is productive, meaning if sputum is present. Sputum is expectorated matter from the respiratory tract, composed of mucus and other secretions. It’s the body’s way of clearing irritants and infections. In cases of respiratory infection, excess mucus is produced, leading to sputum production. The color, consistency, and amount of sputum are important indicators. Purulent sputum, often yellow, green, or brown, typically suggests a bacterial infection.[^2] Figure 8.7 illustrates purulent sputum.
Figure 8.7 Purulent Sputum
Chest pain is another critical subjective symptom. Respiratory and cardiac conditions can cause chest pain, some being life-threatening emergencies. If a patient reports chest pain, immediately assess for emergency signs using questions such as:
- “Does the pain feel like pressure or tightness?”
- “Is the pain radiating to your jaw, arm, or back?”
- “Are you experiencing shortness of breath, dizziness, or nausea alongside the pain?”
Positive responses to these questions necessitate immediate medical attention according to hospital protocols. If the chest pain is not emergent, a focused assessment is needed, including onset, location, duration, characteristics (sharp, dull, aching), alleviating or aggravating factors (e.g., breathing, coughing), radiation, and any pain management used.[^3] Noncardiac chest pain is often exacerbated by coughing and deep breaths.
Objective Respiratory Assessment
Objective assessments are observable and measurable signs of respiratory status. These include airway assessment, respiratory rate, effort, quality, pulse oximetry, lung auscultation, and heart rate.
A patent airway is the first priority. Assess for any obstructions or signs of airway compromise. Evaluate respiratory rate, depth, and rhythm. Note if breathing is labored, shallow, or deep. Observe the use of accessory muscles in the neck and chest, which indicates increased work of breathing. Pulse oximetry provides a noninvasive measurement of peripheral oxygen saturation (SpO2). Auscultate lung sounds to identify normal breath sounds and any adventitious sounds like wheezing, crackles (rales), or rhonchi. Tachycardia (increased heart rate) can be an early sign of hypoxia.
Cyanosis, a bluish discoloration of the skin and mucous membranes, and clubbing of the fingers are objective signs of chronic hypoxia. Clubbing is the bulbous enlargement of the fingertips, often associated with chronic lung diseases such as COPD or congenital heart defects in children. Figure 8.8 demonstrates clubbing.
Figure 8.8 Clubbing of Fingertips
Another sign of chronic respiratory conditions like COPD is barrel chest, an increased anterior-posterior diameter of the chest. This results from chronic air trapping in the alveoli. Figure 8.9 compares a normal chest to a barrel chest.
Figure 8.9 Comparison of Chest with Normal Anterior/Posterior Diameter (A) to a Barrel Chest(B)
Diagnostic Tests and Laboratory Analysis
Diagnostic tests and lab work are guided by the suspected underlying medical condition. For patients with a productive cough, a chest X-ray or sputum culture may be ordered. Patients in respiratory distress often require arterial blood gas (ABG) analysis.
A chest X-ray is a rapid, painless imaging technique using electromagnetic waves to visualize chest structures. It aids in diagnosing conditions like pneumonia, heart failure, lung cancer, and tuberculosis, monitoring treatment effectiveness, and detecting post-procedure complications. Chest X-rays are contraindicated during pregnancy.[^4],[^5] Figure 8.10 shows a chest X-ray image.
Figure 8.10 Chest X-ray
A sputum culture identifies bacteria and other microorganisms in sputum. Patients cough deeply and expectorate sputum into a sterile container. The sample is cultured in a lab for several days to identify pathogens and guide antimicrobial therapy.[^6] Figure 8.11 shows a sputum culture.
Figure 8.11 Sputum Culture
Arterial blood gas (ABG) tests are crucial for patients in respiratory distress. ABGs measure blood pH, partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), bicarbonate (HCO3-), and oxygen saturation (SaO2). Table 8.3a summarizes normal ABG values for adults.
Table 8.3a Normal Ranges of ABG Values in Adults
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |




Common Respiratory Nursing Diagnoses
Based on assessment findings, nurses formulate nursing diagnoses to guide care. For patients with decreased oxygenation and dyspnea, common NANDA-I nursing diagnoses include: Impaired Gas Exchange, Ineffective Breathing Pattern, Ineffective Airway Clearance, Decreased Cardiac Output, and Activity Intolerance.[^7] Table 8.3b provides definitions and defining characteristics for these diagnoses. Always consult a current nursing diagnosis resource when creating a patient care plan.
Table 8.3b NANDA-I Nursing Diagnoses Related to Decreased Oxygenation and Dyspnea[^8]
| NANDA-I Nursing Diagnoses | Definition | Selected Defining Characteristics |
|---|---|---|
| Impaired Gas Exchange | Excess or deficit in oxygenation and/or carbon dioxide elimination | – Abnormal arterial pH – Abnormal skin color – Altered respiratory depth or rhythm – Bradypnea – Confusion – Hypercapnia – Hypoxia or hypoxemia – Irritable mood – Nasal flaring – Psychomotor agitation – Tachycardia – Tachypnea – Somnolence |
| Ineffective Breathing Pattern | Inspiration and/or expiration that does not provide adequate ventilation. | – Abnormal breathing pattern – Bradypnea – Cyanosis – Dyspnea – Hypercapnia – Hyperventilation – Hypoventilation – Increased anterior-posterior chest diameter – Nasal flaring – Orthopnea – Pursed-lip breathing – Tachypnea – Uses accessory muscles to breathe – Uses three-point positioning |
| Ineffective Airway Clearance | Reduced ability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. | – Absence of cough – Adventitious breath sounds – Altered respiratory rhythm – Bradypnea – Excessive sputum – Ineffective sputum elimination – Orthopnea – Psychomotor agitation – Uses accessory muscles to breath |
| Decreased Cardiac Output | Inadequate volume of blood pumped by the heart to meet the metabolic demands of the body. | – Anxiety – Bradycardia – Adventitious breath sounds – Abnormal skin color – Tachycardia – Psychomotor agitation – Fatigue – Edema – Weight gain – Decreased peripheral pulses |
| Activity Intolerance | Insufficient endurance to complete required or desired daily activities. | – Exertional dyspnea – Expresses fatigue – Abnormal heart rate or blood pressure response to activity – Generalized weakness |
For example, in COPD patients, a nurse might identify Ineffective Breathing Pattern by comparing assessment findings to the defining characteristics: dyspnea, barrel chest, nasal flaring, orthopnea, prolonged expiration, pursed-lip breathing, tachypnea, accessory muscle use, and tripod positioning.
Outcome Identification for Respiratory Nursing Care
A broad goal for patients with altered oxygenation is:
- The patient will demonstrate adequate air movement into and out of the lungs.
A SMART (Specific, Measurable, Achievable, Relevant, Time-bound) outcome example for a patient with dyspnea is:
- The patient will report a dyspnea level within their desired range of 1-2 throughout their hospital stay.
Planning and Implementing Respiratory Nursing Interventions
Anxiety Reduction and Respiratory Monitoring are crucial independent nursing interventions for patients experiencing dyspnea and oxygenation issues. Anxiety Reduction involves minimizing apprehension and fear related to respiratory distress. Respiratory Monitoring entails collecting and analyzing patient data to ensure airway patency and adequate gas exchange.[^9] Selected interventions for anxiety reduction and respiratory monitoring are outlined below.
Selected Nursing Interventions for Anxiety Reduction and Respiratory Monitoring[^10]
Anxiety Reduction
- Maintain a calm and reassuring demeanor.
- Thoroughly explain all procedures, including expected sensations.
- Understand the patient’s perspective on stressful situations.
- Provide clear information regarding diagnosis, treatment, and prognosis.
- Stay with the patient to enhance safety and reduce fear.
- Encourage family presence, when appropriate.
- Listen attentively to patient concerns.
- Foster a trusting environment.
- Encourage verbalization of feelings, perceptions, and anxieties.
- Monitor anxiety levels and changes.
- Offer diversional activities to reduce tension.
- Instruct on relaxation techniques (guided imagery, music, massage, aromatherapy, art therapy, yoga, Tai Chi).
- Administer anti-anxiety medications as prescribed.
Respiratory Monitoring
- Monitor respiratory rate, rhythm, depth, and effort.
- Observe chest movement for symmetry, accessory muscle use, and retractions.
- Monitor for abnormal respiratory sounds like snoring, stridor or gurgling.
- Assess breathing patterns (bradypnea, tachypnea, hyperventilation, Kussmaul’s, Cheyne-Stokes).
- Continuously monitor oxygen saturation in sedated patients.
- Utilize continuous oxygen sensors with alarms for at-risk patients, as per policy.
- Auscultate lung sounds, noting decreased/absent sounds and adventitious sounds.
- Assess cough effectiveness.
- Document cough onset, characteristics, and duration.
- Monitor respiratory secretions (color, consistency, amount).
- Determine the need for suctioning.
- Provide frequent respiratory status checks for at-risk patients.
- Monitor dyspnea and factors that improve or worsen it.
- Review chest X-ray reports as indicated.
- Monitor ABG changes and notify the provider as needed.
- Initiate resuscitation efforts when necessary.
- Implement respiratory therapy treatments (nebulizers, chest physiotherapy) as ordered.
In addition to these independent interventions, manage hypoxia with techniques like teaching enhanced breathing and coughing exercises, repositioning, oxygen therapy management, medication administration, and suctioning.
Health promotion is also crucial. Encourage annual influenza and pneumococcal vaccinations (as indicated), smoking cessation, adequate fluid intake to thin secretions, and regular physical activity within tolerance.
Evaluation of Respiratory Nursing Interventions
Continuously evaluate the effectiveness of implemented interventions. Document findings and reassess the nursing care plan. Focused reassessments include heart rate, respiratory rate, pulse oximetry, lung sounds, and patient-reported dyspnea levels. Adjust interventions based on the patient’s response and progress towards desired outcomes.
Glossary of Terms:
Sputum: Mucus and other secretions expelled from the mouth after being coughed up from the respiratory tract.
Purulent Sputum: Yellow, green, or brown sputum, often indicating a respiratory infection.
Clubbing: Enlargement of the fingertips associated with chronic hypoxia.
Barrel Chest: Increased anterior-posterior chest diameter due to air trapping in alveoli, seen in chronic respiratory diseases.
Bradypnea: Abnormally slow respiratory rate, below the normal range for the patient’s age.
Tachypnea: Abnormally fast respiratory rate, above the normal range for the patient’s age.
Orthopnea: Difficulty breathing when lying down, relieved by sitting upright.
[^1]: Registered Nurses’ Association of Ontario. (2005). Nursing care of dyspnea: The 6th vital sign in individuals with chronic obstructive pulmonary disease. https://rnao.ca/bpg/guidelines/dyspnea
[^2]: Barrel, A. (2017). What is a sputum culture test? MedicalNewsToday. https://www.medicalnewstoday.com/articles/318924#what-is-a-sputum-culture-test
[^3]: U.S. National Library of Medicine. (2024). Chest pain. MedlinePlus. https://medlineplus.gov/ency/article/003079.htm
[^4]: National Heart, Lung, and Blood Institute. (n.d.). Chest x-ray. https://www.nhlbi.nih.gov/health-topics/chest-x-ray
[^5]: U.S. National Library of Medicine. (2022). Chest X-ray. MedlinePlus. https://medlineplus.gov/ency/article/003804.htm
[^6]: U.S. National Library of Medicine. (2023). Sputum culture. MedlinePlus. https://medlineplus.gov/ency/article/003723.htm
[^7]: Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2021). Nursing diagnoses: Definitions and classification 2021-2023, Twelfth Edition. Thieme Publishers New York.
[^8]: Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (Eds.). (2021). Nursing diagnoses: Definitions and classification 2021-2023, Twelfth Edition. Thieme Publishers New York.
[^9]: Wagner, C. M., Butcher, H. K., & Clarke, M. F. (2024). Nursing interventions classification (NIC) (8th ed.). Elsevier.
[^10]: Wagner, C. M., Butcher, H. K., & Clarke, M. F. (2024). Nursing interventions classification (NIC) (8th ed.). Elsevier.