Nursing diagnoses are the cornerstone of effective nursing care. They are clinical judgments that nurses make about patient responses to actual and potential health problems. Understanding how to formulate these diagnoses is crucial for nursing students and practicing nurses alike. This guide will delve into the concept of nursing diagnosis, exploring its types, components, and providing numerous Nursing Diagnosis Statement Examples to help you master this essential skill.
Understanding Nursing Diagnosis
A nursing diagnosis is more than just identifying a patient’s illness. It’s a statement that describes a patient’s health condition from a nursing perspective. According to the North American Nursing Diagnosis Association (NANDA-I), it is defined as a “clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community.”
Nursing diagnoses are vital because they:
- Enhance Critical Thinking: For nursing students, formulating diagnoses sharpens problem-solving and critical thinking abilities.
- Prioritize Care: They help nurses identify the most pressing patient needs, guiding the direction of nursing interventions.
- Establish Expected Outcomes: They are essential for defining measurable goals and evaluating the effectiveness of care, meeting quality assurance standards.
- Recognize Patient Responses: They highlight how individuals respond to health issues and identify patient strengths that can be utilized in care.
- Facilitate Communication: They provide a standardized language for nurses and the healthcare team, improving communication and collaboration.
- Evaluate Care Effectiveness: They offer a basis to assess whether nursing care has positively impacted the patient and been cost-effective.
Nursing Diagnosis vs. Medical Diagnosis vs. Collaborative Problems
It’s important to distinguish nursing diagnoses from medical diagnoses and collaborative problems:
-
Nursing Diagnosis: Focuses on the patient’s response to a health condition. It addresses issues that nurses can independently treat within their scope of practice. Examples include Anxiety related to hospitalization or Deficient Knowledge about medication regimen.
-
Medical Diagnosis: Identifies the disease or pathology. This is made by a physician and deals with conditions that require medical treatment. Examples include Diabetes Mellitus, Pneumonia, or Appendicitis. Nurses implement medical orders related to medical diagnoses.
-
Collaborative Problems: These are potential or actual health complications that require both medical and nursing interventions. Nurses monitor for these complications and implement interventions prescribed by physicians and independently initiated nursing actions. An example is Risk for Complications related to surgery.
The key difference is that nursing diagnoses are patient-centered and focus on responses to illness, while medical diagnoses are disease-centered. Collaborative problems bridge both medical and nursing domains.
Classification of Nursing Diagnoses: NANDA-I Taxonomy
Nursing diagnoses are not randomly created; they are standardized and classified. The most widely used classification system is the NANDA-I (North American Nursing Diagnosis Association International) taxonomy. This system organizes diagnoses into a multi-axial framework for clarity and consistency.
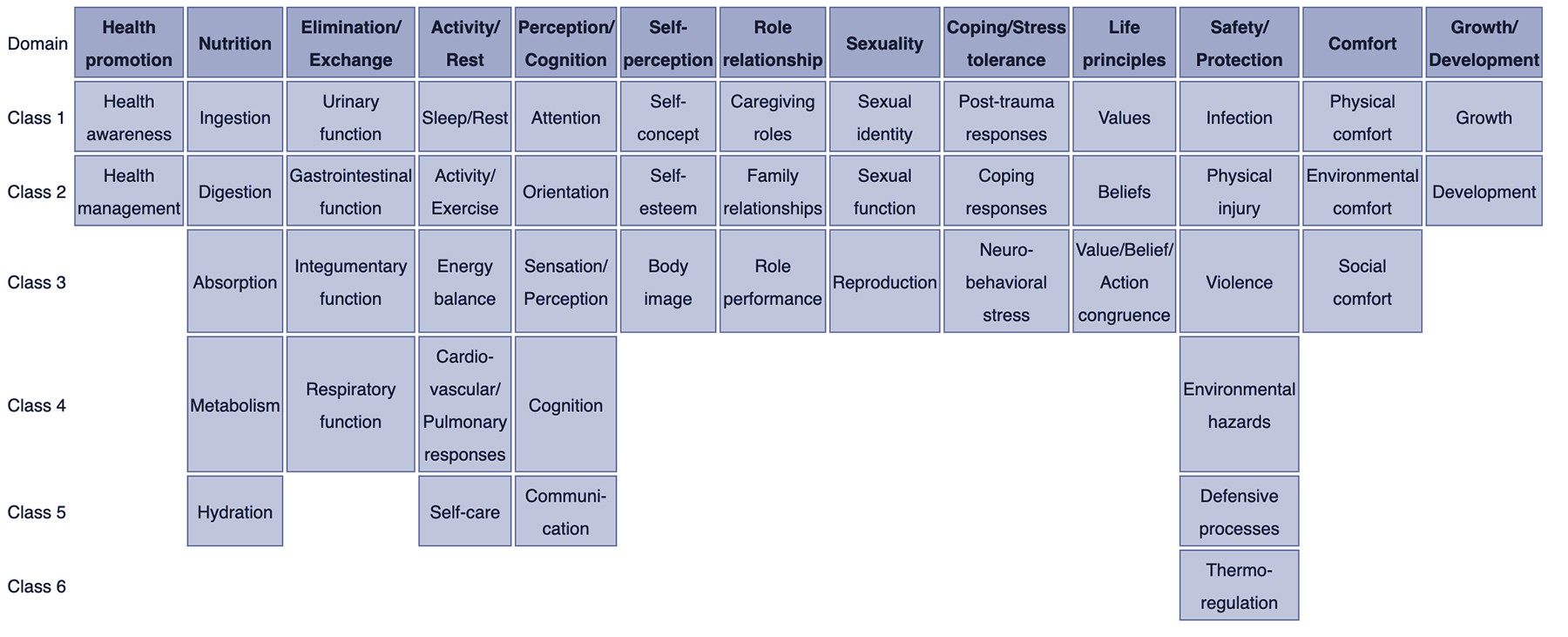
The NANDA-I taxonomy is organized into:
- Domains (13): Broad areas of human functioning (e.g., Health Promotion, Nutrition, Elimination and Exchange).
- Classes (47): Subcategories within domains (e.g., Health Awareness, Ingestion, Urinary Function).
- Nursing Diagnoses: Specific diagnostic labels within classes, providing a standardized language.
Here’s a brief overview of the NANDA-I Domains and Classes:
Domain 1. Health Promotion
- Class 1. Health Awareness
- Class 2. Health Management
Domain 2. Nutrition
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
Domain 3. Elimination and Exchange
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
Domain 4. Activity/Rest
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
Domain 5. Perception/Cognition
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
Domain 6. Self-Perception
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
Domain 7. Role relationship
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
Domain 8. Sexuality
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
Domain 9. Coping/stress tolerance
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
Domain 10. Life principles
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
Domain 11. Safety/Protection
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
Domain 12. Comfort
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
Domain 13. Growth/Development
- Class 1. Growth
- Class 2. Development
This taxonomy provides a structured approach to selecting appropriate nursing diagnoses.
Types of Nursing Diagnoses with Statement Examples
There are four main types of nursing diagnoses: Problem-Focused (Actual), Risk, Health Promotion, and Syndrome. Understanding each type is essential for accurate diagnosis.
1. Problem-Focused Nursing Diagnosis (Actual Diagnosis)
A problem-focused diagnosis describes a current problem that the patient is experiencing at the time of assessment. It’s supported by defining characteristics – observable signs and symptoms.
Components:
- Nursing Diagnosis Label: The NANDA-I approved name for the diagnosis.
- Related Factors: Factors contributing to the problem (etiology).
- Defining Characteristics: Signs and symptoms that demonstrate the presence of the problem.
Connecting Phrases: “related to” (R/T) links the diagnosis label to related factors, and “as evidenced by” (AEB) links related factors to defining characteristics.
Nursing Diagnosis Statement Examples:
- Pain related to surgical incision AEB patient reporting a pain level of 7 out of 10, guarding behavior, and increased heart rate.
- Impaired Physical Mobility related to right knee pain and stiffness AEB inability to bear weight on right leg and limited range of motion in right knee.
- Deficient Knowledge related to newly diagnosed diabetes mellitus AEB patient asking questions about insulin administration and dietary management, and stating “I don’t know how to check my blood sugar.”
- Anxiety related to upcoming surgery AEB patient expressing feelings of worry and apprehension, restlessness, and increased perspiration.
- Ineffective Airway Clearance related to excessive mucus AEB productive cough with thick yellow sputum, adventitious breath sounds (rhonchi), and decreased oxygen saturation.
- Constipation related to decreased fluid intake and immobility AEB reported infrequent bowel movements, abdominal distention, and hard, dry stools.
- Disturbed Sleep Pattern related to hospital environment and pain AEB patient reports difficulty falling asleep and frequent awakenings, dark circles under eyes, and irritability.
- Self-Care Deficit: Bathing/Hygiene related to physical weakness AEB inability to wash body and comb hair without assistance, and unkempt appearance.
- Impaired Skin Integrity related to prolonged pressure AEB stage II pressure ulcer on sacrum, redness, and broken skin.
- Ineffective Health Management related to complexity of medication regimen and lack of social support AEB missed medication doses, expressed difficulty remembering medications, and lives alone.
2. Risk Nursing Diagnosis
A risk nursing diagnosis identifies potential problems that a patient is vulnerable to developing. It doesn’t describe a current problem, but rather highlights risk factors that increase susceptibility.
Components:
- Nursing Diagnosis Label: NANDA-I approved risk diagnosis.
- Risk Factors: Factors that increase the patient’s vulnerability.
Connecting Phrase: “as evidenced by” (AEB) is used to link the risk diagnosis label to risk factors.
Nursing Diagnosis Statement Examples:
- Risk for Infection as evidenced by surgical incision, compromised immune system, and presence of intravenous catheter.
- Risk for Falls as evidenced by muscle weakness, unsteady gait, history of falls, and use of walker.
- Risk for Injury as evidenced by altered sensory perception (peripheral neuropathy) and decreased lower extremity sensation.
- Risk for Impaired Skin Integrity as evidenced by immobility, incontinence, and poor nutritional status.
- Risk for Deficient Fluid Volume as evidenced by excessive vomiting, diarrhea, and decreased oral intake.
- Risk for Unstable Blood Glucose Level as evidenced by inconsistent meal times, lack of adherence to diabetic diet, and insufficient insulin administration.
- Risk for Spiritual Distress as evidenced by loss of loved one, lack of social support, and questioning meaning of suffering.
- Risk for Delayed Surgical Recovery as evidenced by advanced age, chronic obstructive pulmonary disease (COPD), and poor nutritional status.
- Risk for Aspiration as evidenced by impaired swallowing, decreased level of consciousness, and presence of nasogastric tube.
- Risk for Caregiver Role Strain as evidenced by complexity of caregiving tasks, insufficient resources, and social isolation.
3. Health Promotion Diagnosis
A health promotion diagnosis focuses on a patient’s desire and motivation to improve their well-being and health. It identifies strengths and readiness to enhance health behaviors.
Components:
- Nursing Diagnosis Label: NANDA-I approved health promotion diagnosis (often a one-part statement).
- Defining Characteristics: May be added to clarify the patient’s readiness.
Nursing Diagnosis Statement Examples:
- Readiness for Enhanced Knowledge related to medication management as evidenced by patient actively seeking information and asking specific questions about medication side effects and administration.
- Readiness for Enhanced Nutrition as evidenced by patient expressing interest in learning about healthy eating habits and requesting dietary counseling.
- Readiness for Enhanced Self-Care as evidenced by patient demonstrating motivation to participate in activities of daily living and expressing desire for increased independence.
- Readiness for Enhanced Coping as evidenced by patient verbalizing effective stress management techniques and seeking support systems.
- Readiness for Enhanced Parenting as evidenced by parents actively participating in infant care education and demonstrating positive attachment behaviors.
- Readiness for Enhanced Spiritual Well-being as evidenced by patient expressing desire for spiritual growth and seeking opportunities for prayer and meditation.
- Readiness for Enhanced Family Processes as evidenced by family members expressing desire to improve communication and resolve conflicts.
- Readiness for Enhanced Immunization Status as evidenced by patient expressing understanding of the importance of vaccinations and scheduling appointments for recommended immunizations.
- Readiness for Enhanced Sleep as evidenced by patient expressing desire to improve sleep hygiene and seeking information on relaxation techniques to promote sleep.
- Readiness for Enhanced Therapeutic Regimen Management as evidenced by patient demonstrating understanding of treatment plan and actively participating in self-management strategies.
4. Syndrome Nursing Diagnosis
A syndrome diagnosis represents a cluster of nursing diagnoses that often occur together in a specific situation. It’s a diagnostic label that encompasses a group of predictable actual or risk diagnoses.
Components:
- Nursing Diagnosis Label: NANDA-I approved syndrome diagnosis (one-part statement).
Nursing Diagnosis Statement Examples:
- Rape-Trauma Syndrome
- Relocation Stress Syndrome
- Impaired Environmental Interpretation Syndrome
- Post-Trauma Syndrome
- Chronic Pain Syndrome
- Disuse Syndrome
- Failure to Thrive Syndrome
- Sudden Infant Death Syndrome (SIDS) – While nurses do not diagnose SIDS, they address parental grieving and support related to this syndrome.
- Maternal Role Attainment Syndrome – Focuses on the process of a woman adopting a maternal role.
- Frailty Syndrome – Characterized by decreased physiological reserve and increased vulnerability to stressors in older adults.
5. Possible Nursing Diagnosis
A possible nursing diagnosis is used when the nurse suspects a diagnosis but lacks sufficient evidence to confirm it. It indicates that more data is needed to either confirm or rule out the suspected problem. It is not officially recognized as a type of diagnosis like the other four, but is a useful term in practice.
Nursing Diagnosis Statement Examples:
- Possible Ineffective Coping related to unclear stressors. Further assessment is needed to identify specific stressors and coping mechanisms.
- Possible Risk for Spiritual Distress related to unknown personal values and beliefs. Requires further exploration of patient’s spiritual background.
- Possible Deficient Knowledge related to new treatment regimen, needs further assessment to determine specific knowledge gaps.
Components of a Nursing Diagnosis Statement
A complete nursing diagnosis statement, particularly for problem-focused diagnoses, often includes three parts, often referred to as the PES format:
- P (Problem): The NANDA-I diagnostic label (concise term or phrase).
- E (Etiology): The related factors or “related to” phrase (causes or contributing factors).
- S (Signs and Symptoms): The defining characteristics or “as evidenced by” phrase (observable cues).
For risk diagnoses, it is a two-part statement (PR), and health promotion and syndrome diagnoses are usually one-part statements (P).
Example using PES Format:
P: Acute Pain
E: related to surgical incision
S: as evidenced by patient reporting pain level of 8/10, guarding behavior, and facial grimacing.
Full Nursing Diagnosis Statement (PES): Acute Pain related to surgical incision as evidenced by patient reporting pain level of 8/10, guarding behavior, and facial grimacing.
Writing Effective Nursing Diagnosis Statements
To write clear and effective nursing diagnosis statements:
- Be Specific and Concise: Use precise language and avoid jargon.
- Patient-Centered: Focus on the patient’s response, not the nurse’s needs.
- Use NANDA-I Terminology: Utilize standardized diagnostic labels for clarity and consistency.
- Address Only One Problem: Each diagnosis statement should focus on a single patient issue.
- Be Ethically and Culturally Sensitive: Consider the patient’s background and values.
- Base on Assessment Data: Ensure the diagnosis is supported by evidence from your assessment.
- Review and Revise: Nursing diagnoses are dynamic and should be reviewed and revised as the patient’s condition changes.
Nursing Diagnosis Examples for Care Plans
Nursing diagnoses are the foundation of nursing care plans. They guide the selection of nursing interventions and the establishment of patient outcomes. Here are more examples of nursing diagnoses commonly used in care plans, categorized by common nursing concepts:
Safety and Security:
- Risk for Falls related to impaired balance and medication side effects.
- Risk for Injury related to decreased sensation and cognitive impairment.
- Risk for Infection related to invasive procedures and compromised immune system.
- Deficient Knowledge related to home safety measures AEB expressed concerns about preventing falls at home.
Physiological Needs:
- Impaired Gas Exchange related to pneumonia AEB decreased oxygen saturation and shortness of breath.
- Ineffective Breathing Pattern related to anxiety AEB rapid, shallow respirations and reports of feeling breathless.
- Decreased Cardiac Output related to myocardial infarction AEB chest pain, dyspnea, and changes in blood pressure.
- Deficient Fluid Volume related to excessive diarrhea AEB decreased urine output, dry mucous membranes, and increased heart rate.
- Excess Fluid Volume related to heart failure AEB edema, weight gain, and shortness of breath.
- Imbalanced Nutrition: Less Than Body Requirements related to nausea and anorexia AEB weight loss and reported decreased appetite.
- Constipation related to pain medication and decreased mobility AEB infrequent bowel movements and abdominal distention.
- Diarrhea related to antibiotic therapy AEB frequent, watery stools and abdominal cramping.
- Urinary Incontinence related to decreased bladder control AEB involuntary loss of urine with coughing and sneezing.
- Impaired Skin Integrity related to pressure and friction AEB redness and breakdown of skin on heels.
- Acute Pain related to surgical incision AEB patient reporting pain level of 7/10 and guarding behavior.
- Chronic Pain related to arthritis AEB patient reporting persistent joint pain and limited mobility.
- Disturbed Sleep Pattern related to noise and unfamiliar environment AEB patient reports difficulty falling asleep and frequent awakenings.
Psychosocial Needs:
- Anxiety related to diagnosis and prognosis AEB patient expressing worry and apprehension, and restlessness.
- Fear related to upcoming procedures AEB patient verbalizing fear of pain and unknown outcomes.
- Ineffective Coping related to situational crises AEB patient expressing feelings of being overwhelmed and difficulty problem-solving.
- Disturbed Body Image related to amputation AEB patient expressing negative feelings about appearance and social withdrawal.
- Spiritual Distress related to loss of meaning and purpose AEB patient questioning beliefs and expressing feelings of hopelessness.
- Social Isolation related to chronic illness and mobility limitations AEB patient reports feeling lonely and withdrawn from social activities.
Learning Needs:
- Deficient Knowledge related to medication regimen AEB patient asking questions about medication purpose and side effects.
- Readiness for Enhanced Learning related to wound care management as evidenced by patient expressing interest and asking questions about wound care procedures.
These examples provide a starting point for understanding and formulating nursing diagnosis statements. Remember to always individualize diagnoses based on your patient’s specific assessment data and needs.
Recommended Resources
To further enhance your understanding of nursing diagnosis, consider these resources:
- Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care: A comprehensive guide with evidence-based interventions.
- Nursing Care Plans – Nursing Diagnosis & Intervention: Offers numerous care plans and reflects current evidence-based guidelines.
- Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales: A quick reference tool for identifying correct diagnoses and interventions.
- Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care: Detailed resource for planning and documenting individualized care.
- All-in-One Nursing Care Planning Resource: Covers various specialties and provides interprofessional perspectives.
By mastering nursing diagnosis, you will strengthen your clinical judgment, improve patient care planning, and contribute to better patient outcomes. The examples and guidance provided here are designed to empower you to confidently formulate accurate and effective nursing diagnosis statements.
References and Sources:
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- NANDA International, Inc. (2018). Nursing diagnoses: Definitions and classification 2018-2020. Eleventh edition. New York, NY: Thieme Medical Publishers, Inc.