Nursing diagnosis is a cornerstone of modern nursing practice. As a crucial step in the nursing process, it empowers nurses to deliver patient-centered care and achieve optimal health outcomes. This guide provides an in-depth exploration of nursing diagnosis, designed to enhance your understanding and skills, particularly within nursing lab settings. We will delve into the definition, purpose, types, and formulation of nursing diagnoses, ensuring you are well-equipped to excel in both academic and clinical environments.
What is a Nursing Diagnosis?
A nursing diagnosis is defined as a clinical judgment concerning a human response to health conditions, life processes, or vulnerabilities to those responses. This response can be observed in individuals, families, groups, or communities. Essentially, it’s a statement that describes a patient’s health problem that nurses are licensed and competent to treat. Nursing diagnoses form the foundation for selecting nursing interventions and achieving specific patient outcomes for which nurses are accountable. These diagnoses are meticulously developed based on data gathered during the comprehensive nursing assessment, enabling nurses to create individualized nursing care plans.
Purposes of Nursing Diagnosis
Nursing diagnoses serve several vital purposes in healthcare, especially within the context of nursing labs and practical training:
- Enhancing Critical Thinking and Problem-Solving: For nursing students, working with nursing diagnoses in labs is an invaluable teaching tool. It hones problem-solving and critical thinking skills, essential for effective patient care.
- Prioritizing Nursing Care: Nursing diagnoses help identify immediate patient needs and establish nursing priorities. This prioritization guides the direction of nursing interventions to address the most pressing issues first.
- Formulating Expected Outcomes: They are instrumental in setting measurable expected outcomes, which are crucial for quality assurance and meeting the requirements of healthcare payers.
- Understanding Patient Responses: Nursing diagnoses facilitate a deeper understanding of how patients respond to actual or potential health challenges and life events. Recognizing available patient resources and strengths becomes easier, aiding in problem prevention and resolution.
- Facilitating Communication: They establish a common language and framework for clear communication among nursing professionals and the broader healthcare team. This shared understanding is vital for collaborative patient care.
- Evaluating Nursing Care Effectiveness: Nursing diagnoses provide a basis for evaluation, helping to determine the effectiveness and cost-efficiency of nursing care provided to patients.
Nursing Diagnoses vs. Medical Diagnoses vs. Collaborative Problems
It’s important to distinguish between nursing diagnoses, medical diagnoses, and collaborative problems. The term nursing diagnosis is directly linked to the diagnosis phase, the second step in the nursing process (Assessment, Diagnosis, Planning, Implementation, Evaluation – ADPIE). It also refers to the specific label assigned when nurses interpret assessment data and identify a patient problem that falls within the nursing domain.
For example, during a patient assessment, a nurse might observe that a patient is experiencing feelings of anxiety, expresses fear, and has difficulty falling sleep. These observations lead to the nursing diagnoses: Anxiety, Fear, and Disturbed Sleep Pattern. In this context, the nursing diagnosis focuses on the patient’s response to their medical condition, not the medical condition itself. This is why it’s termed a ‘nursing diagnosis’ – it pertains to issues nurses are autonomously qualified to address within the context of a disease or condition, encompassing physical, mental, and spiritual responses. Therefore, nursing diagnosis is fundamentally care-oriented.
COMPARISON TABLE. Nursing Diagnoses, Medical Diagnoses, and Collaborative Problems
| Feature | Nursing Diagnosis | Medical Diagnosis | Collaborative Problems |
|---|---|---|---|
| Focus | Patient’s response to health conditions/life processes | Disease, pathology, or medical condition itself | Potential complications from medical conditions or treatments |
| Who Diagnoses | Nurses | Physicians or advanced healthcare practitioners | Nurses (in collaboration with physicians) |
| Treatment Focus | Nursing interventions, patient care, support | Medical treatments, medications, surgery, therapies | Monitoring, preventing complications, collaborative interventions |
| Examples | Anxiety, Impaired Skin Integrity, Acute Pain | Diabetes Mellitus, Pneumonia, Appendicitis | Potential Complications of Surgery, Side Effects of Medications |
| Changes? | Can change as patient’s condition changes | Generally remains constant throughout the illness | Resolve when the potential complication is prevented or managed |
Medical diagnoses, on the other hand, are made by physicians or advanced practitioners. They pinpoint specific diseases, medical conditions, or pathological states that only medical professionals can treat. Through their expertise, physicians identify the precise clinical entity causing the illness and prescribe appropriate medication or treatments to cure it. Examples of medical diagnoses include Diabetes Mellitus, Tuberculosis, Amputation, Hepatitis, and Chronic Kidney Disease. Medical diagnoses typically remain constant throughout the illness. Nurses are responsible for implementing physician’s orders and carrying out prescribed medical treatments and therapies.
Collaborative problems represent potential physiological complications that nurses monitor and manage using both independent nursing interventions and physician-prescribed treatments. These problems necessitate a collaborative approach, with nursing interventions focused on closely monitoring the patient’s condition and preventing potential complications from developing.
Understanding these distinctions is crucial for effective nursing practice. Nursing diagnoses direct nursing care towards patient-centered responses, while medical diagnoses guide medical treatment of diseases. Collaborative problems bridge the gap, requiring both medical and nursing expertise for optimal patient outcomes.
Classification of Nursing Diagnoses (Taxonomy II)
Nursing diagnoses are systematically organized and classified to provide a standardized framework for nursing practice. In 2002, Taxonomy II was adopted, based on Dr. Mary Joy Gordon’s Functional Health Patterns assessment framework. Taxonomy II is hierarchical, comprising three levels: Domains (13), Classes (47), and individual nursing diagnoses. While not directly grouped by Gordon’s patterns anymore, diagnoses are coded using seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. Importantly, diagnoses are now listed alphabetically by their concept, not the first word, for easier navigation.
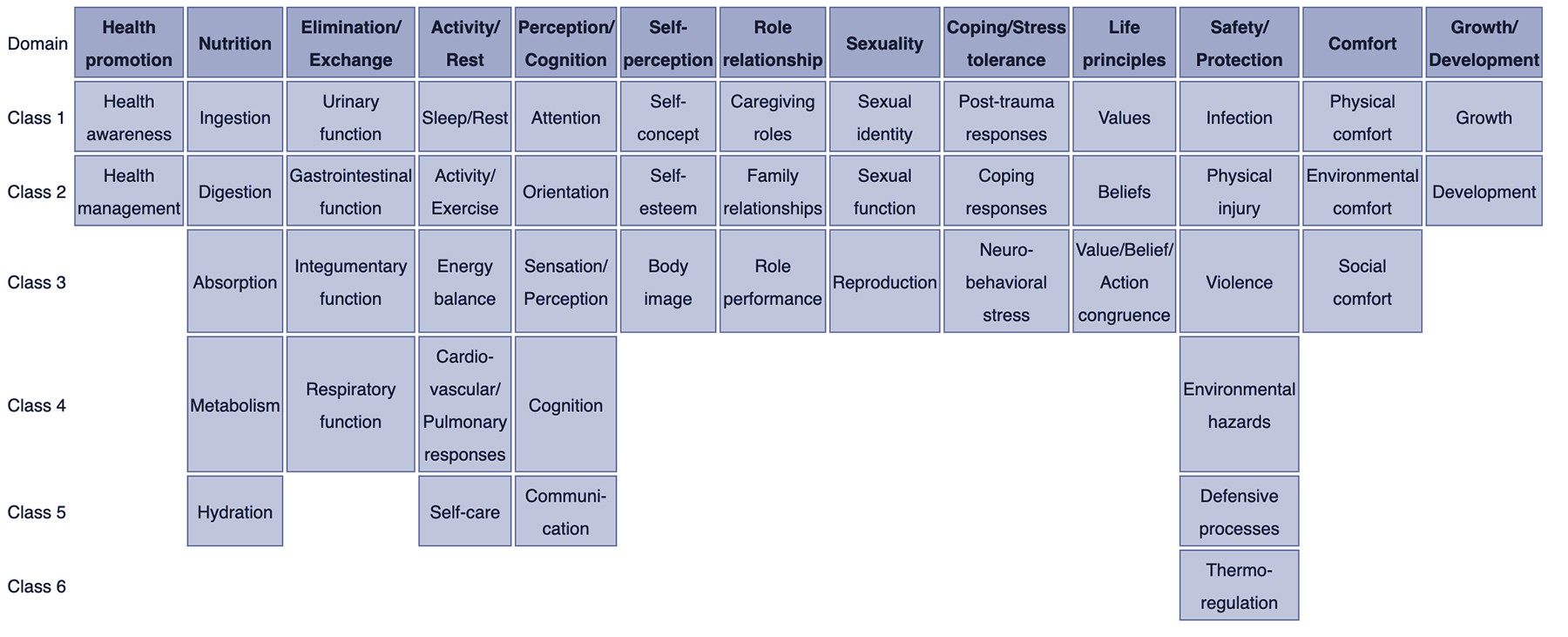
NURSING DIAGNOSIS TAXONOMY II. Taxonomy II provides a structured classification system with 13 domains and 47 classes. Image source: Wikipedia.com
Here’s a breakdown of the Domains and Classes within Taxonomy II, offering a comprehensive overview of the scope of nursing diagnoses:
- Domain 1. Health Promotion
- Class 1. Health Awareness
- Class 2. Health Management
- Domain 2. Nutrition
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Domain 3. Elimination and Exchange
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Domain 4. Activity/Rest
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Domain 5. Perception/Cognition
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Domain 6. Self-Perception
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Domain 7. Role relationship
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Domain 8. Sexuality
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Domain 9. Coping/stress tolerance
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Domain 10. Life principles
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Domain 11. Safety/Protection
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Domain 12. Comfort
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Domain 13. Growth/Development
- Class 1. Growth
- Class 2. Development
Nursing Process Integration
The nursing process is a systematic, five-stage approach to patient care: assessment, diagnosing, planning, implementation, and evaluation. Nursing diagnosis is the critical second step, directly following assessment and leading to planning. Each stage of the nursing process demands critical thinking and clinical reasoning from the nurse. Beyond simply understanding nursing diagnosis definitions, nurses must be adept at recognizing defining characteristics and behaviors associated with each diagnosis, identifying related factors, and selecting appropriate interventions.
To further explore the steps, importance, purposes, and characteristics of the nursing process, refer to this comprehensive guide: “The Nursing Process: A Comprehensive Guide“. This resource will deepen your understanding of how nursing diagnosis fits within the broader framework of patient care.
Types of Nursing Diagnoses
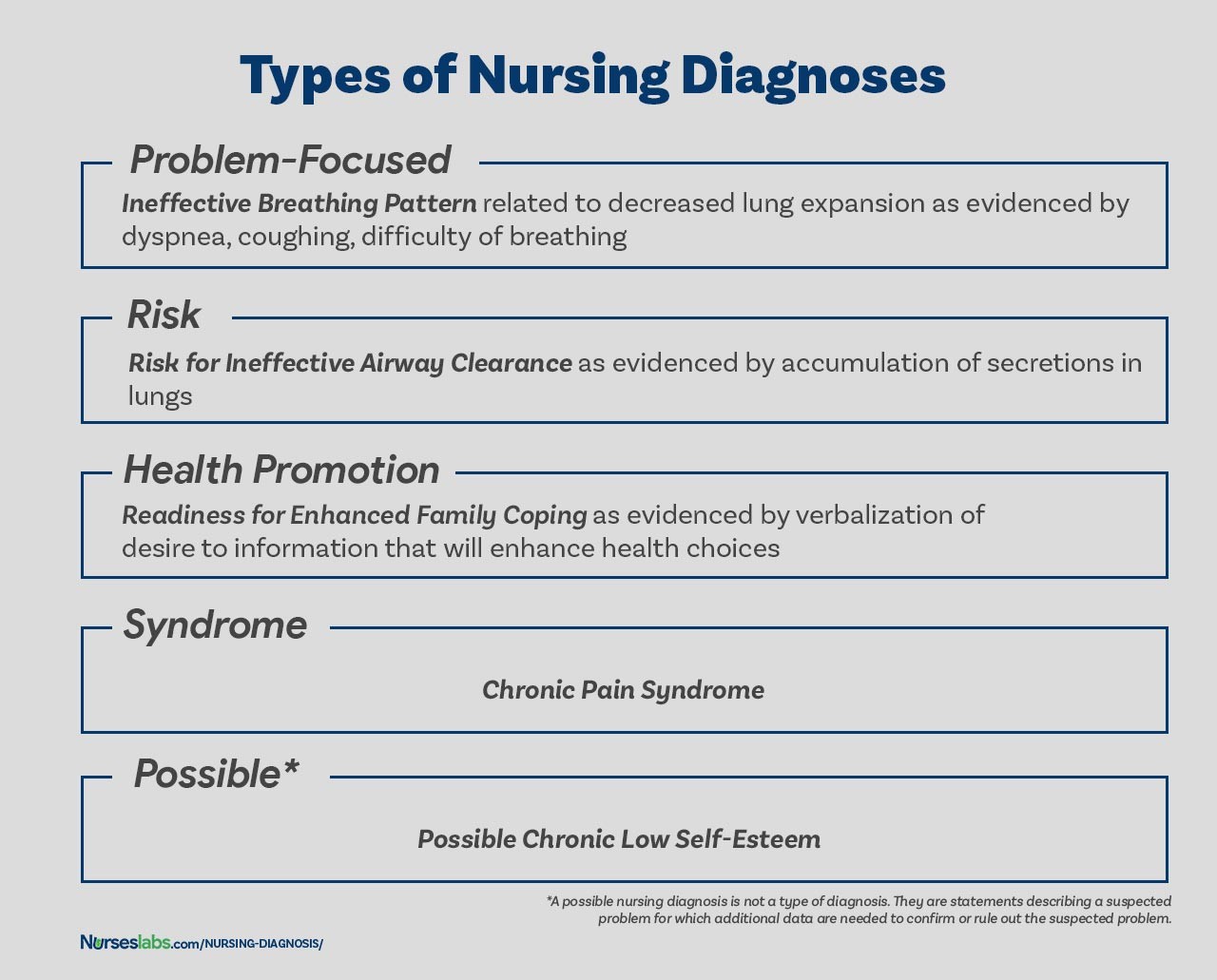
There are four primary types of nursing diagnoses: Problem-Focused (Actual), Risk, Health Promotion, and Syndrome. Understanding these categories is essential for accurate diagnosis and care planning.
TYPES OF NURSING DIAGNOSES. These four categories – Problem-Focused, Risk, Health Promotion, and Syndrome – encompass the range of nursing diagnoses used in practice.
Problem-Focused Nursing Diagnosis
A problem-focused diagnosis, also known as an actual diagnosis, identifies a patient problem that is present at the time of the nursing assessment. These diagnoses are substantiated by the presence of defining signs and symptoms. It’s crucial to recognize that actual diagnoses are not inherently more critical than risk diagnoses; in many situations, a risk diagnosis can be the top priority for patient care.
Problem-focused nursing diagnoses are structured with three key components: (1) the nursing diagnosis label, (2) related factors, and (3) defining characteristics.
Examples of problem-focused nursing diagnoses include:
- Acute Pain related to surgical incision as evidenced by patient reporting pain level of 7/10 and guarding behavior.
- Impaired Physical Mobility related to musculoskeletal injury as evidenced by limited range of motion and inability to ambulate independently.
- Deficient Knowledge related to new medication regimen as evidenced by patient asking questions about medication purpose and dosage.
Risk Nursing Diagnosis
Risk nursing diagnoses are clinical judgments that a problem does not currently exist, but risk factors are present indicating a heightened likelihood of the problem developing without nursing intervention. A risk diagnosis is based on the patient’s current health status, past health history, and identified risk factors that increase their susceptibility to a health problem. These diagnoses are integral to proactive nursing care, enabling nurses to identify potential issues early and implement preventive measures.
Unlike problem-focused diagnoses, risk diagnoses do not have etiological factors or “related to” factors. Instead, the increased susceptibility is directly attributed to the identified risk factors. For instance, an elderly patient with diabetes and vertigo who struggles with walking and refuses assistance with ambulation would be appropriately diagnosed with Risk for Injury or Risk for Falls.
IMPORTANT: For risk nursing diagnoses, the phrase “as evidenced by” connects the risk diagnosis label directly to the risk factors, not defining characteristics. The components are:
- Risk diagnostic label, linked by “as evidenced by”
- Risk factors
Examples of risk nursing diagnoses include:
- Risk for Injury as evidenced by impaired cognitive awareness and use of sedative medications.
- Risk for Infection as evidenced by surgical wound, compromised immune system, and prolonged hospitalization.
- Risk for Falls as evidenced by muscle weakness, history of previous falls, impaired mobility, and use of assistive devices.
Health Promotion Diagnosis
Health promotion diagnoses, also known as wellness diagnoses, are clinical judgments concerning a patient’s motivation and desire to enhance their well-being. They articulate a patient’s readiness to engage in activities that promote health and improve their current wellness level. For instance, a new mother expressing keen interest in learning proper breastfeeding techniques could receive a health promotion diagnosis of “Readiness for Enhanced Breastfeeding.” This diagnosis then guides nursing interventions focused on supporting the patient in learning and successfully implementing breastfeeding practices.
Health promotion diagnoses focus on facilitating an individual’s, family’s, or community’s transition from their current wellness state to a higher level. Components typically include only the diagnostic label—a one-part statement. However, related factors can be added for clarity and to further specify the area of health promotion.
Examples of health promotion diagnoses:
- Readiness for Enhanced Nutrition
- Readiness for Enhanced Family Coping
- Readiness for Enhanced Knowledge
Syndrome Diagnosis
A syndrome diagnosis is a clinical judgment describing a cluster of actual or risk nursing diagnoses predicted to occur together due to a specific situation or event. Like health promotion diagnoses, they are written as a one-part statement, requiring only the diagnostic label. Syndrome diagnoses recognize patterns of diagnoses that frequently co-occur.
Examples of syndrome nursing diagnoses:
- Rape Trauma Syndrome
- Disuse Syndrome
- Relocation Stress Syndrome
Possible Nursing Diagnosis
A possible nursing diagnosis is not a distinct type like the others. Instead, it signifies a statement describing a suspected problem requiring additional data to confirm or rule out. Possible diagnoses serve as a communication tool among nurses, indicating a potential diagnosis but highlighting the need for further data collection to confirm or refute it.
Examples include:
- Possible Spiritual Distress related to loss of faith as evidenced by patient statements of questioning beliefs (requires further spiritual assessment).
- Possible Situational Low Self-Esteem related to job loss (requires further assessment of self-perception and coping mechanisms).
Components of a Nursing Diagnosis
A well-formulated nursing diagnosis typically comprises three components: (1) the problem and its definition, (2) the etiology (related factors), and (3) the defining characteristics or risk factors (for risk diagnoses).
Problem and Definition
The problem statement, or diagnostic label, concisely describes the patient’s health problem or response requiring nursing intervention. A diagnostic label usually has two parts: a qualifier and the focus of the diagnosis. Qualifiers, also known as modifiers, are words added to diagnostic labels to provide further context, specificity, or limitation to the diagnostic statement. One-word nursing diagnoses (e.g., Anxiety, Constipation, Diarrhea, Nausea) are exceptions, as their qualifier and focus are inherent in the term itself.
| Qualifier | Focus of the Diagnosis |
|---|---|
| Deficient | Fluid volume |
| Imbalanced | Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange |
| Ineffective | Tissue Perfusion |
| Risk for | Injury |
Etiology
The etiology, or related factors, component identifies the probable cause(s) of the health problem. These are the conditions contributing to the problem’s development, guiding nursing therapy and allowing for individualized patient care. Nursing interventions should be directed at addressing the etiological factors to resolve the underlying cause of the nursing diagnosis. Etiology is linked to the problem statement using the phrase “related to.”
Example:
- Acute Pain related to surgical incision. (Here, “surgical incision” is the etiology of the acute pain.)
Risk Factors
Risk factors are used in place of etiological factors for risk nursing diagnoses. Risk factors are elements that increase an individual’s or group’s vulnerability to an unhealthy condition. They are written following the phrase “as evidenced by” in the diagnostic statement.
Examples:
- Risk for falls as evidenced by advanced age and use of walker.
- Risk for infection as evidenced by break in skin integrity.
Defining Characteristics
Defining characteristics are clusters of signs and symptoms that indicate the presence of an actual nursing diagnosis. For problem-focused diagnoses, these are the observable signs and symptoms exhibited by the patient. Risk diagnoses, by nature, do not have present signs and symptoms; instead, the risk factors themselves serve as the evidence for the potential problem. Defining characteristics are linked to the diagnostic label using the phrases “as evidenced by” or “as manifested by.”
Example:
- Anxiety related to unfamiliar hospital environment as manifested by restlessness, verbalization of worry, and increased heart rate. (Restlessness, verbal worry, and increased heart rate are the defining characteristics of anxiety in this case.)
Diagnostic Process: How to Diagnose
The diagnostic process involves three key phases: (1) data analysis, (2) identification of health problems, risks, and strengths, and (3) formulation of diagnostic statements.
Analyzing Data
Data analysis involves several critical steps: comparing patient data against established norms and standards, clustering related cues together, and identifying any gaps or inconsistencies in the data. This rigorous analysis ensures a comprehensive understanding of the patient’s health status.
Identifying Health Problems, Risks, and Strengths
Following data analysis, the nurse, in collaboration with the patient when possible, identifies health problems that support potential actual, risk, and possible diagnoses. This step involves differentiating between nursing diagnoses, medical diagnoses, and collaborative problems to ensure the focus remains within the nursing domain. Crucially, this stage also includes recognizing the patient’s strengths, available resources, and coping abilities, which are vital for holistic care planning.
Formulating Diagnostic Statements
The final step is formulating clear and concise diagnostic statements. This process is detailed in the next section, outlining how to accurately and effectively write nursing diagnoses.
How to Write a Nursing Diagnosis?
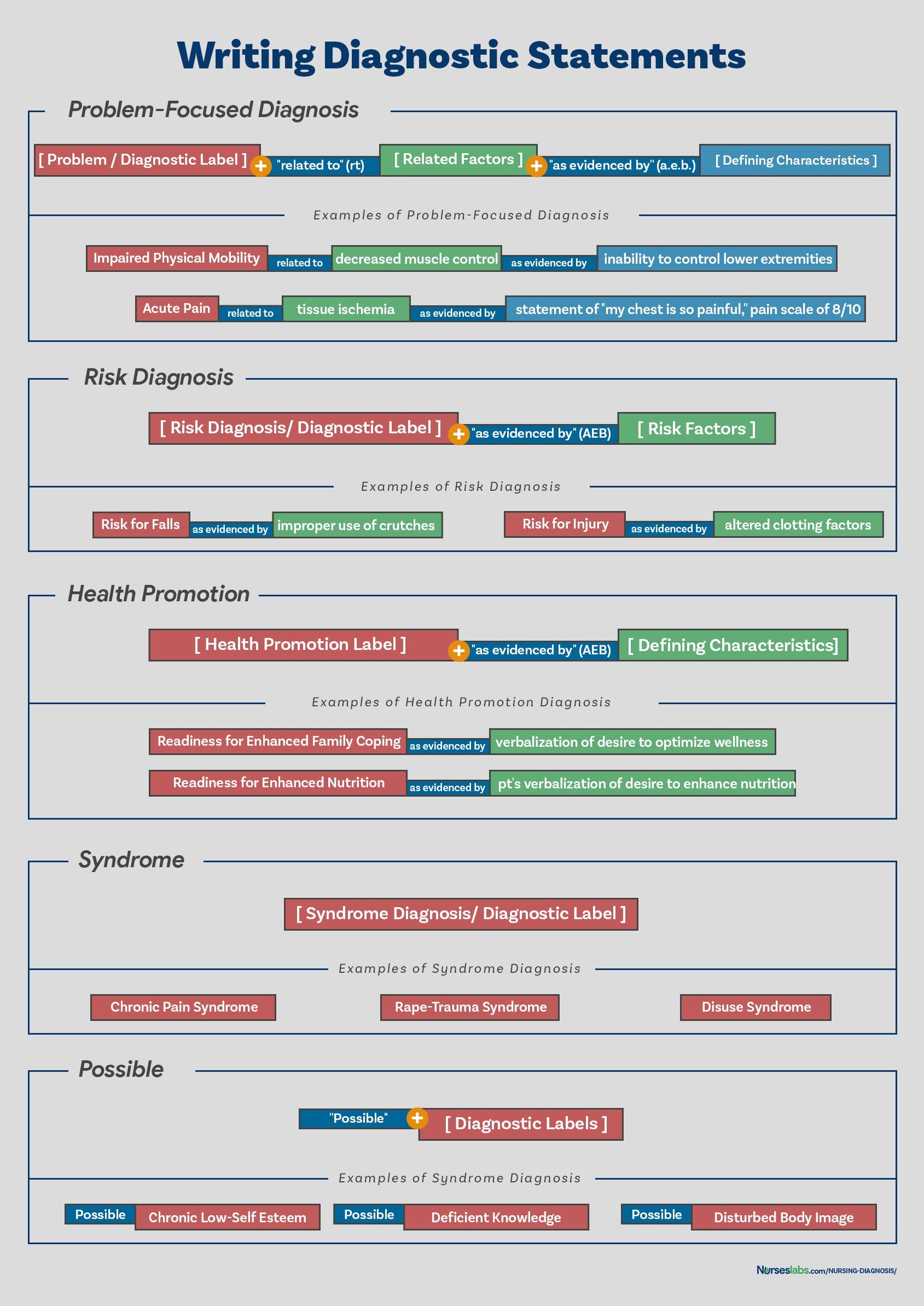
Writing effective nursing diagnostic statements requires clearly describing an individual’s health status and the contributing factors. Not all types of diagnostic indicators need to be included in every statement. The format for writing diagnostic statements varies depending on the type of nursing diagnosis.
WRITING DIAGNOSTIC STATEMENTS. This chart summarizes how to write diagnostic statements for different types of nursing diagnoses.
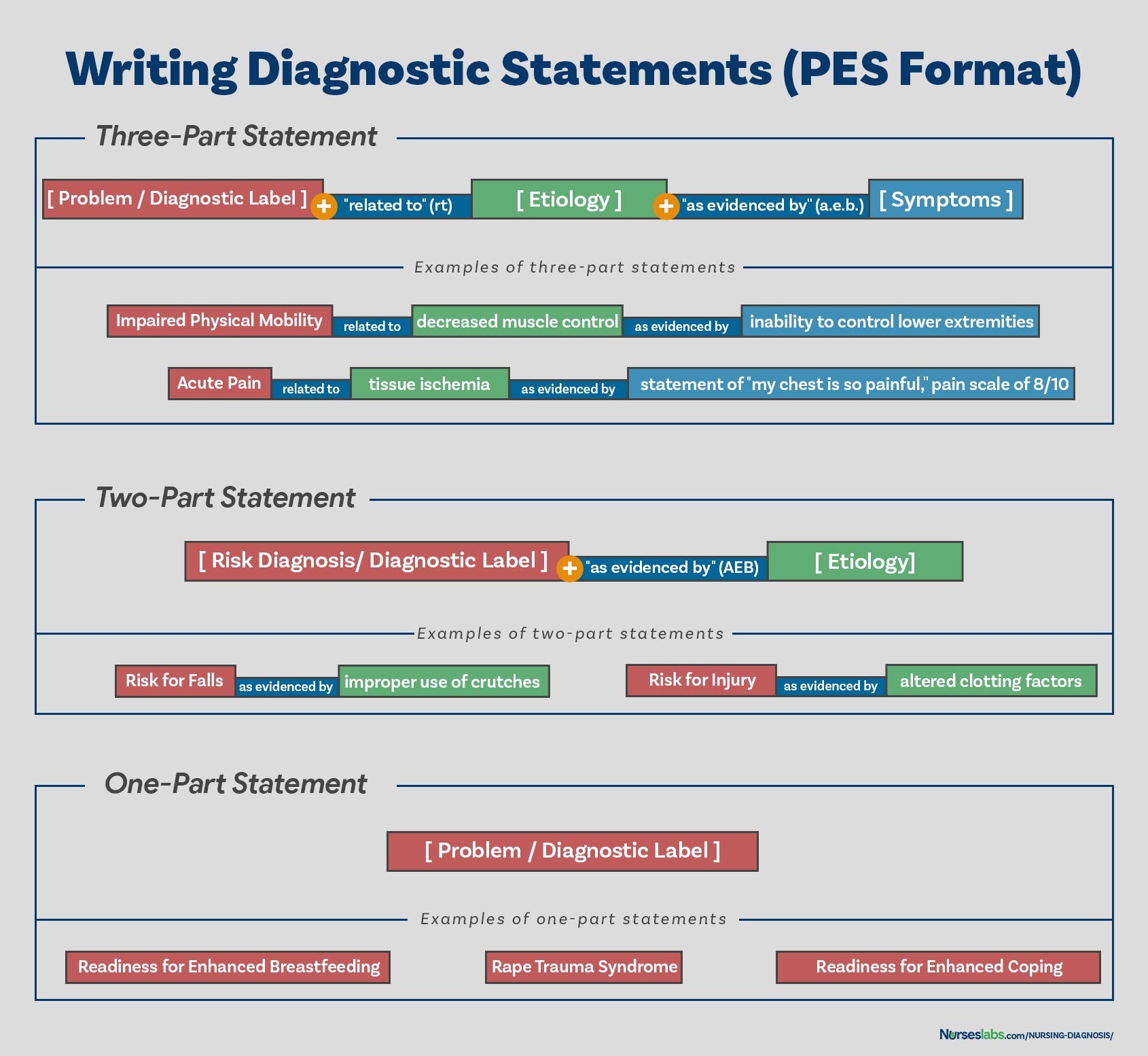
PES Format
The PES format is a widely used method for constructing nursing diagnostic statements. PES stands for:
- Problem (diagnostic label)
- Etiology (related factors)
- Signs/Symptoms (defining characteristics)
Diagnostic statements can be structured as one-part, two-part, or three-part statements using the PES format, depending on the type of diagnosis.
PES FORMAT. This illustrates how the PES format is applied to different types of nursing diagnoses.
One-Part Nursing Diagnosis Statement
Health promotion diagnoses are typically written as one-part statements because the related factor is inherently “motivated to achieve a higher level of wellness.” While related factors can be added for further clarification, they are not always necessary. Syndrome diagnoses also generally lack related factors, making them suitable for one-part statements.
Examples of one-part nursing diagnosis statements:
- Readiness for Enhanced Coping
- Rape Trauma Syndrome
Two-Part Nursing Diagnosis Statement
Risk and possible nursing diagnoses are written as two-part statements. The first part is the diagnostic label, and the second part is the validation for a risk diagnosis (risk factors) or the reason for suspecting a possible diagnosis. A third part (signs and symptoms) is not applicable to risk or possible diagnoses because the problem is not yet confirmed or present.
Examples of two-part nursing diagnosis statements:
- Risk for Infection as evidenced by weakened immune system response
- Risk for Injury as evidenced by unstable hemodynamic profile
Three-part Nursing Diagnosis Statement
Problem-focused (actual) nursing diagnoses are typically written as three-part statements, utilizing the full PES format. This includes: diagnostic label (Problem), contributing factors (“related to” – Etiology), and signs and symptoms (“as evidenced by” or “as manifested by” – Signs/Symptoms). The three-part statement provides a comprehensive picture of the nursing diagnosis.
Example of a three-part nursing diagnosis statement:
- Deficient Fluid Volume related to excessive vomiting and diarrhea as evidenced by decreased urine output, dry mucous membranes, and poor skin turgor.
Variations on Basic Statement Formats
There are slight variations in writing nursing diagnosis statements to ensure clarity and accuracy in different clinical situations. These variations generally involve adding qualifiers or specifying locations or affected body parts to the basic PES format.
Nursing Diagnosis for Care Plans
This section serves as a starting point for developing your nursing care plans. It provides a database of common nursing diagnosis examples that you can adapt and utilize to create individualized care plans for your patients.
See also: Nursing Care Plans (NCP): Ultimate Guide and List for a comprehensive resource on care planning.
Recommended Resources
To further enhance your understanding and skills in nursing diagnosis and care planning, consider these recommended books and resources:
Disclosure: The following are affiliate links from Amazon. Purchases made through these links may earn a small commission, at no additional cost to you. For more information, please review our privacy policy.
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care
This handbook is highly recommended for its evidence-based approach to nursing interventions. It uses a clear three-step system to guide you through client assessment, nursing diagnosis, and care plan development. It includes step-by-step instructions for implementing care and evaluating outcomes, helping you build diagnostic reasoning and critical thinking skills.
Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition)
This resource includes over two hundred care plans reflecting the latest evidence-based guidelines. The 10th edition features new content on ICNP diagnoses, LGBTQ health issues, and electrolyte and acid-base balance.
Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales
This quick-reference tool is essential for identifying accurate diagnoses and planning efficient patient care. The 16th edition includes the most current nursing diagnoses and interventions, with an alphabetized listing of diagnoses covering over 400 disorders.
Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care
This manual assists in identifying interventions for planning, individualizing, and documenting care for over 800 diseases and disorders. For each diagnosis, it provides subjective and objective data, sample clinical applications, prioritized actions/interventions with rationales, documentation sections, and more.
This comprehensive e-book features over 100 care plans across medical-surgical, maternity/OB, pediatrics, and psychiatric-mental health nursing. It utilizes an interprofessional “patient problems” approach, familiarizing you with patient-centered communication.
See also
Explore these additional resources on our site for further learning:
- Nursing Care Plans (NCP): Ultimate Guide and List
- The Nursing Process: A Comprehensive Guide
- Head-to-Toe Assessment: Complete Physical Assessment Guide
References and Sources
The information in this Nursing Diagnosis guide is based on the following references and resources, recommended for further reading:
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice. Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis. Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education. New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis. Qualitative health research, 12(7), 945-965.
