Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disease that affects motor neurons in the brain and spinal cord. This devastating condition leads to muscle weakness, loss of motor function, and eventually, death, typically from respiratory failure within 2 to 3 years of diagnosis. The journey with ALS is incredibly challenging, not only for the individual diagnosed but also for their families and caregivers. While there is currently no cure for ALS, palliative care offers a crucial layer of support, focusing on improving the quality of life from diagnosis through bereavement.
Palliative care is specialized medical care for individuals facing serious illnesses like ALS. It centers on providing relief from the symptoms and stress of the illness, with the primary goal of enhancing the quality of life for both the patient and their family. For ALS, palliative care is not just end-of-life care; it’s an approach that should be integrated from the moment of diagnosis, evolving with the patient’s needs throughout the disease trajectory and extending to support the family through bereavement.
Understanding the Role of Palliative Care in ALS
The multifaceted symptoms of ALS, including progressive weakness, spasticity, excessive saliva (sialorrhea), speech difficulties (dysarthria), swallowing problems (dysphagia), weight loss, shortness of breath, and emotional lability (pseudobulbar affect), create a significant burden. Furthermore, a notable percentage of ALS patients may also develop frontotemporal dementia, adding cognitive and behavioral challenges to the physical decline. These complexities underscore the necessity of a holistic approach to care, which palliative care expertly provides.
Early integration of palliative care in ALS management is highly recommended by leading medical organizations worldwide. It assists with:
- Symptom Management: Addressing the wide array of physical and psychological symptoms associated with ALS to maximize comfort and function.
- Advance Care Planning: Facilitating crucial conversations about patient values, preferences, and future care decisions, especially concerning life-sustaining treatments.
- Support for Family Caregivers: Providing emotional, practical, and respite support to those who are essential in the care of individuals with ALS.
Despite these recognized benefits, the implementation of effective palliative care models in ALS is still evolving. This article will delve into the structure, impact, and essential components of integrating palliative care into the comprehensive management of ALS, from diagnosis to bereavement, drawing on insights from a pilot program designed to provide longitudinal, interdisciplinary palliative care.
A Model for Longitudinal, Interdisciplinary Palliative Care in ALS
A pioneering model of collaborative care was developed and studied at the University of California, San Francisco (UCSF), embedding a specialized palliative care team within an existing ALS clinic. This program aimed to provide continuous, interdisciplinary palliative care to patients and families facing ALS, aiming to understand its effectiveness and share valuable lessons for others developing similar collaborations.
Collaborative Care Structure
The UCSF model involved a transdisciplinary palliative care team comprising physicians, a nurse, a social worker, and a chaplain, working in close coordination with the ALS clinic’s team. Referrals to palliative care were made by ALS physicians based on patient needs, typically for complex symptom management, intricate goals of care discussions, or significant psychosocial or spiritual distress.
The collaborative nature of this model ensured a clear division of labor and expertise:
- ALS Physician: Focused on neurological monitoring, prognosis, and disease-modifying treatments.
- Palliative Care Physician: Managed physical and psychological symptoms, such as pain, shortness of breath, depression, and anxiety.
- ALS Nurse: Coordinated care related to disease treatments, feeding tubes, assistive devices, and equipment.
- Palliative Care Nurse: Provided symptom follow-up, medication management support, and acted as a point of contact between visits.
- ALS Social Worker: Counseled on benefits, resources, and services available through organizations like the ALS Association.
- Palliative Care Social Worker: Offered emotional support, non-pharmacological symptom management techniques (mindfulness, coping strategies), and family support.
- Palliative Care Chaplain: Addressed spiritual and existential concerns, provided support for anticipatory grief and loss of meaning.
This integrated approach minimized duplication and maximized the strengths of each team, providing comprehensive and well-coordinated care. Initially, palliative care visits were often scheduled on the same day as ALS clinic appointments. However, this evolved to separate video visits to reduce patient fatigue and accommodate differing visit frequencies. Regular communication, including shared clinical notes and case conferences, maintained strong collaboration between the teams.
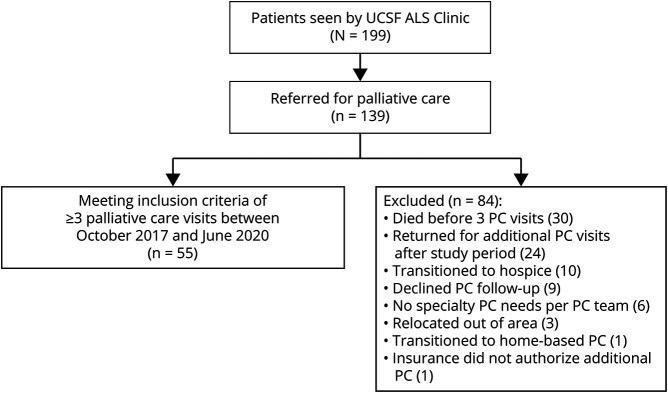
Patient Flowchart: Enrollment in Amyotrophic Lateral Sclerosis (ALS) Palliative Care Program Study.
Patient Demographics and Referral Reasons
The study cohort included 55 ALS patients who received at least three palliative care visits. The demographic profile of these patients was largely representative of the broader ALS population, with a mean age of 65.8 years, and a slight female majority (47.3%). The majority were Caucasian (74.5%) and English-speaking (78.2%).
Patients were typically referred to palliative care around six months after establishing care at the ALS clinic, indicating a move towards earlier integration of palliative support. The primary reasons for referral highlighted the core needs palliative care addresses in ALS:
- Advance Care Planning (ACP) and Goals of Care (58.2%): Reflecting the importance of early conversations about future care preferences.
- Patient and Family Support (52.7%): Acknowledging the significant emotional and practical burden of ALS on the entire family unit.
- Non-Pain Symptom Management (50.9%): Addressing the complex array of distressing physical symptoms beyond pain.
- Specific Treatment Decision Support (23.6%): Assisting with challenging choices regarding interventions like ventilation or feeding tubes.
- Pain Management (9.1%): While less frequent as a primary referral reason, pain is still a significant concern for some ALS patients.
- Hospice Referral and Discussion (9.1%): Initiating conversations about end-of-life care options when appropriate.
These referral patterns underscore the diverse needs that palliative care addresses in ALS, spanning from early planning and symptom control to end-of-life considerations.
Impact of Palliative Care on Advance Care Planning and End-of-Life Care
One of the most significant findings of the UCSF pilot program was the substantial increase in advance care planning documentation among patients receiving palliative care. Before palliative care involvement, only 16.4% of patients had advance directives documented in their electronic health records, and 10.9% had Physician Orders for Life-Sustaining Treatment (POLST) forms. Following palliative care, these rates dramatically increased to 36.4% for advance directives and 63.6% for POLST forms.
This marked improvement highlights the effectiveness of palliative care in facilitating crucial conversations and documentation regarding patients’ wishes for future medical care. It’s important to note that palliative care supports informed decision-making aligned with individual values, and not all patients opted to forgo life-sustaining interventions. This underscores that palliative care is about patient-centered care, respecting diverse goals and preferences.
Trends in Advance Care Planning With Palliative Care for ALS Patients, demonstrating increased completion of Advance Directives and POLST forms.
Furthermore, the study revealed a high rate of hospice utilization among patients who received palliative care. Among those who died during the study period, 75.9% utilized hospice services at the end of life, with a significant proportion (over half) receiving hospice care for more than 30 days. This suggests that palliative care not only facilitates advance care planning but also promotes the utilization of appropriate end-of-life care services like hospice, which focuses on comfort and quality of life in the final stages of illness.
Addressing Diverse Needs Through Interdisciplinary Care
The interdisciplinary palliative care team consistently addressed a wide range of needs across physical, psychological, social, and spiritual domains. The most frequently identified needs and interventions included:
- Non-Pain Symptoms (94.5%): Comprehensive management of symptoms like shortness of breath, fatigue, insomnia, and gastrointestinal issues.
- Care Planning (96.4%): Facilitating discussions about goals of care, advance directives, and future medical decisions.
- Family/Caregiver Support (96.4%): Providing emotional support, education, and practical resources to family caregivers.
- Psychosocial Distress (78.2%): Addressing anxiety, depression, coping with diagnosis, and emotional lability.
- Spiritual Concerns (29.1%): Supporting patients and families in exploring meaning, purpose, and spiritual well-being in the face of serious illness.
- Pain (43.6%): Managing pain through pharmacological and non-pharmacological approaches.
This data highlights the breadth of palliative care’s impact, extending beyond just physical symptom management to encompass the emotional, social, and spiritual well-being of both the patient and their family. The interdisciplinary team approach allows for a holistic response to the complex challenges of ALS.
Palliative Care Needs Identified and Interventions Provided to ALS Patients, demonstrating the breadth of issues addressed by the interdisciplinary team.
Palliative Care and Medical Aid in Dying in ALS
An important aspect of end-of-life care in regions where it is legal, like California, is Medical Aid in Dying (MAID). The study found that a significant proportion of patients (30.9%) inquired about MAID, and nearly 30% of deaths in the cohort occurred through the ingestion of MAID medications.
This highlights the importance of palliative care teams being prepared to discuss MAID openly and respectfully with patients who express interest. The collaborative model between ALS and palliative care teams is crucial in these cases, ensuring coordinated care that adheres to legal requirements and respects patient autonomy. For ALS patients, the progressive physical decline and communication challenges make timely and well-coordinated access to MAID, when desired and eligible, particularly important.
From Diagnosis to Bereavement: Palliative Care as a Continuous Support System
Palliative care in ALS is not a one-time intervention; it’s a continuous support system that evolves alongside the patient’s journey with the disease. From the initial diagnosis, palliative care focuses on proactive symptom management, advance care planning, and emotional support. As the disease progresses, palliative care intensifies its focus on managing increasing symptom burden, adapting care plans to changing needs, and providing ongoing psychosocial and spiritual support.
In the later stages of ALS, palliative care seamlessly integrates with hospice care, providing specialized comfort-focused care as death approaches. Hospice services offer an enhanced level of support, including home-based care, medication management, and bereavement support for families.
Furthermore, palliative care extends beyond the patient’s death to provide bereavement support for the family. Grief is a natural and complex process, and families who have cared for a loved one with ALS often face unique challenges. Palliative care teams can offer counseling, resources, and support groups to help families navigate the bereavement period and adjust to life after loss.
Conclusion: The Essential Role of Palliative Care in ALS
This study and the experiences of the UCSF pilot program reinforce the vital role of integrating longitudinal, interdisciplinary palliative care into the management of amyotrophic lateral sclerosis. Palliative care is feasible, addresses critical needs across multiple domains, and significantly improves advance care planning for individuals with ALS. It emphasizes quality of life, patient-centered care, and comprehensive support for both patients and their families throughout the entire disease trajectory, from diagnosis to bereavement.
While further controlled studies are needed to fully quantify the impact of palliative care in ALS, the evidence strongly supports its integration as a standard of care. For healthcare providers, early referral to palliative care should be a priority for all individuals diagnosed with ALS. For patients and families facing ALS, understanding and accessing palliative care is essential to navigating this challenging journey with dignity, comfort, and the best possible quality of life.
Take-Home Points:
- Longitudinal palliative care comanagement for ALS is feasible and addresses physical, psychological, practical, and spiritual needs.
- Palliative care should be integrated early after ALS diagnosis, focusing on advance care planning, symptom management, and family support.
- Interdisciplinary palliative care significantly increases advance care planning rates, promotes hospice utilization, and supports informed decision-making, including discussions about Medical Aid in Dying where legal.
- Palliative care in ALS extends from diagnosis through bereavement, providing continuous support for patients and families.
End-of-Life Care for Patients Who Died in the ALS Palliative Care Program, showing location of death and hospice utilization rates.
References
[References from the original article would be listed here, maintaining the original numbering and content.]
Disclaimer: This article is for informational purposes only and does not provide medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of amyotrophic lateral sclerosis.