Introduction
Pericardial effusion, the abnormal accumulation of fluid in the pericardial cavity, is a frequently encountered condition in clinical settings. For automotive repair professionals at xentrydiagnosis.store, understanding the intricacies of medical diagnoses, even those seemingly outside the automotive realm, enhances critical thinking and problem-solving skills applicable to complex vehicle diagnostics. While seemingly disparate, the systematic approach to diagnosing pericardial effusion shares parallels with diagnosing intricate vehicle malfunctions. The initial challenge in Pericardial Effusion Diagnosis, much like in automotive repair, lies in establishing the underlying cause. In some cases, the effusion is clearly linked to pre-existing conditions such as acute myocardial infarction, post-cardiac surgery complications, end-stage renal disease, or metastatic cancers. However, when the etiology is not immediately apparent, a thorough diagnostic approach is crucial. This article provides a comprehensive overview of pericardial effusion diagnosis, encompassing etiology, hemodynamic impact, and management strategies, mirroring the detailed diagnostic processes we champion at xentrydiagnosis.store for automotive repair.
Clinical Approach to Etiologic Diagnosis of Pericardial Effusion
When faced with a patient exhibiting pericardial effusion, the primary step in pericardial effusion diagnosis is determining the underlying cause. Similar to troubleshooting a vehicle issue, a systematic approach is essential. In some instances, the cause is readily apparent, linked to existing medical conditions or recent procedures. For example, pericardial effusion can arise as a complication of acute myocardial infarction, cardiac surgery, chest radiation therapy, or in patients with end-stage renal failure or those who have undergone invasive cardiac procedures. However, even when these predisposing factors are present, it’s crucial to consider other potential etiologies in the differential diagnosis.
The presence of malignancy in a patient with pericardial effusion presents a complex diagnostic challenge. It’s important to note that pericardial effusion in cancer patients isn’t always directly attributable to neoplastic pericardial involvement. Studies have shown that in a significant proportion of cancer patients with pericardial effusion, the cause may be benign, such as idiopathic pericarditis or radiation-induced pericarditis. Therefore, accurate pericardial effusion diagnosis in this context is vital for appropriate prognostic and therapeutic decisions. Advanced imaging techniques like CT, MRI, and positron emission tomography, along with pericardioscopy, can be valuable tools in determining the presence and extent of neoplastic disease and differentiating it from other causes of effusion.
Table 1: Common Causes of Pericardial Effusion
| Secondary to Underlying Known Disease | Without Underlying Known Disease |
|---|---|
| Acute Myocardial Infarction | Acute Inflammatory Pericarditis (Infectious, Autoimmune) |
| Cardiac Surgery | Previously Unknown Neoplasia |
| Trauma | Idiopathic Pericardial Effusion |
| Widespread Known Neoplasia | |
| Chest Radiation | |
| End-Stage Renal Failure | |
| Invasive Cardiac Procedures | |
| Hypothyroidism | |
| Autoimmune Diseases |
In many cases, the etiology of pericardial effusion remains unclear initially. While definitive pericardial effusion diagnosis requires specific investigations, certain clinical indicators can guide clinicians toward a likely etiologic category. Factors such as hemodynamic compromise, cardiomegaly, pleural effusion, and the size of the pericardial effusion itself can provide clues. Hemorrhagic pericardial effusion, while sometimes associated with neoplasia, can also occur in idiopathic pericarditis.
A prospective study analyzing clinical findings in patients with moderate to severe pericardial effusion revealed that the presence or absence of inflammatory signs (pericarditic chest pain, fever, pericardial friction rub), along with the presence of underlying disease and cardiac tamponade, are significant predictors in pericardial effusion diagnosis. The study highlighted that inflammatory signs strongly suggest acute idiopathic pericarditis, while the absence of these signs in severe effusion without tamponade points towards chronic idiopathic pericardial effusion. Conversely, tamponade without inflammatory signs raises suspicion for neoplastic pericardial effusion. Epidemiological factors are also crucial; idiopathic pericarditis is prevalent in developed countries, while tuberculous pericarditis remains a leading cause in underdeveloped regions, emphasizing the importance of considering geographical context in pericardial effusion diagnosis.
Evaluation of Hemodynamic Compromise in Pericardial Effusion
Evaluating hemodynamic compromise is a critical aspect of pericardial effusion diagnosis and management. Cardiac tamponade represents the most severe form of hemodynamic compromise resulting from pericardial effusion. Clinical signs of tamponade are readily recognizable and include dyspnea, tachycardia, jugular venous distension, pulsus paradoxus, and in severe cases, arterial hypotension and shock.
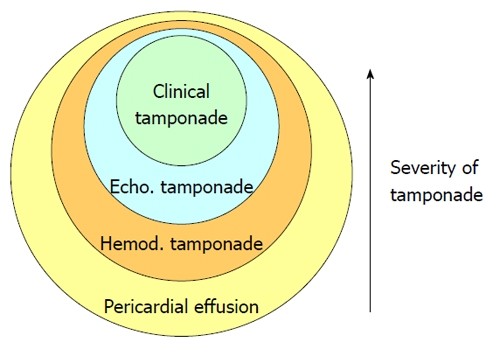
Figure 1: Grading Severity of Hemodynamic Compromise in Pericardial Effusion
Echocardiography plays a vital role in pericardial effusion diagnosis, often revealing signs of hemodynamic compromise, such as cardiac chamber collapse and altered mitral and tricuspid flow patterns, even in the absence of overt clinical tamponade. These echocardiographic findings are significant as they indicate elevated intrapericardial pressure, even in patients without classic clinical tamponade signs. Studies correlating echocardiographic and cardiac catheterization data have demonstrated that echocardiography can detect hemodynamic compromise earlier than clinical examination alone.
Research has established that cardiac tamponade exists on a continuum, ranging from subtle increases in intrapericardial pressure to severe hemodynamic instability. Even asymptomatic large pericardial effusions can exhibit hemodynamic tamponade criteria, highlighting the importance of echocardiographic assessment in all cases of pericardial effusion for accurate pericardial effusion diagnosis and risk stratification. The severity of hemodynamic derangement, rather than simply its presence or absence, is the crucial factor to assess in patients with pericardial effusion.
Etiologic Spectrum of Moderate and Large Pericardial Effusions
A wide range of conditions can lead to pericardial effusion, making comprehensive pericardial effusion diagnosis essential. Acute pericarditis, regardless of etiology (idiopathic, viral, autoimmune, or physical), is frequently associated with pericardial effusion. Other conditions include neoplasia, myxoedema, renal failure, pregnancy, aortic rupture, and conditions causing fluid retention such as heart failure and nephrotic syndrome.
The prevalence of different etiologies varies depending on patient populations and geographic location. Idiopathic/viral pericarditis is common in outpatient settings in the Western world, while neoplastic, uremic, and iatrogenic causes are more prevalent in hospital settings. Tuberculous pericarditis remains a leading cause in developing countries. Understanding these epidemiological variations is important for effective pericardial effusion diagnosis.
Several prospective studies have investigated the etiology of large pericardial effusions of unknown origin. These studies, while varying in their definitions of “large” effusion and study protocols, consistently highlight the diagnostic challenges and the spectrum of underlying causes. Neoplastic, idiopathic, and uremic etiologies are frequently reported, but the precise distribution varies across studies. Sophisticated diagnostic protocols, including molecular techniques, can increase the yield of specific etiologic diagnoses, particularly in infectious pericarditis, but the cost-effectiveness of such extensive investigations must be considered in routine pericardial effusion diagnosis.
The hemodynamic severity of pericardial effusion also correlates with etiology. Studies focusing on patients with clinical cardiac tamponade show a higher prevalence of neoplastic etiologies, emphasizing the importance of considering malignancy in cases of tamponade during pericardial effusion diagnosis.
Table 2: Etiologies in Moderate-Large Pericardial Effusion Trials
| Etiology (%) | Corey et al. | Colombo et al. | Sagristà-Sauleda et al. | Corey et al. |
|---|---|---|---|---|
| Effusion Size | > 5 mm | > 10 mm | > 10 mm | Not reported |
| n | 57 | 25 | 322 | 106 |
| Tamponade (%) | Not reported | 44 | 37 | Not reported |
| Idiopathic (%) | 7 | 32 | 20¹ | 25 |
| Chronic Idiopathic Effusion (%) | ? | ? | 9 | ? |
| Neoplastic (%) | 23 | 36 | 13 | 37 |
| Uremia (%) | 12 | 20 | 6 | 4 |
| Iatrogenic (%) | 0 | 0 | 16 | 0 |
| Post-AMI (%) | 0 | 8 | 8 | 0 |
| Viral (%) | 14 | 0 | 0 | 7 |
| Collagen Vascular Disease (%) | 12 | 0 | 5 | 5 |
| Tuberculosis (%) | 0 | 0 | 2 | 2 |
| Other (%) | 9 | 4 | 21 | 20² |
¹Acute idiopathic pericarditis; ²Includes bacterial pericardial effusion; ?: No distinction between acute idiopathic pericarditis and idiopathic chronic pericardial effusion.
Medical Treatment of Pericardial Effusion
Medical treatment of pericardial effusion is guided by the presence of inflammatory signs and the underlying etiology, integral considerations in pericardial effusion diagnosis. For patients with acute inflammatory signs, aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) are recommended. Steroids should be avoided in acute inflammatory pericarditis due to the increased risk of relapses. Colchicine is effective for relapsing pericarditis and may prevent recurrences in initial episodes of acute pericarditis.
Patients with acute viral or idiopathic pericarditis without high-risk features can be managed as outpatients. Figure 2 outlines the management of acute pericarditis. When a specific etiology is identified (bacterial, tuberculous), treatment targets the causative agent, often with pericardial drainage if hemodynamic compromise is present. Close monitoring is necessary due to the risk of constrictive pericarditis. For acute idiopathic or viral pericarditis with moderate to severe effusion, regular echocardiographic follow-up is crucial until resolution. Neoplastic pericarditis management requires a tailored approach, considering the underlying malignancy and prognosis, which is vital in the overall pericardial effusion diagnosis and treatment strategy.
Figure 2: Management Strategy for Pericardial Effusion with Acute Pericarditis
Indications for Pericardial Drainage Procedures
Pericardial drainage procedures are performed for both diagnostic and therapeutic purposes, particularly in cases of cardiac tamponade. However, in patients without hemodynamic compromise, the diagnostic yield of pericardial fluid or tissue analysis is low, impacting the pericardial effusion diagnosis pathway. Routine pericardial drainage in the absence of hemodynamic compromise is generally not justified.
Exceptions to this include suspected purulent or tuberculous pericarditis, where invasive procedures are warranted. In patients with underlying malignancies, pericardial fluid examination helps differentiate between neoplastic and non-neoplastic effusions. Furthermore, prophylactic pericardiocentesis is recommended in asymptomatic patients with massive idiopathic chronic pericardial effusion due to the risk of unexpected tamponade. These specific indications highlight the nuanced decision-making process in pericardial effusion diagnosis and management.
Selection of Pericardial Drainage Procedures
Various pericardial drainage procedures exist, ranging from needle pericardiocentesis to open surgical drainage. The choice of procedure depends largely on the etiology of the effusion, a key factor identified during pericardial effusion diagnosis. Simple pericardiocentesis is often sufficient for idiopathic or viral pericarditis. Purulent pericarditis typically requires surgical drainage, often via subxiphoid pericardiotomy.
Table 3: Pericardial Drainage Procedures
| Procedures |
|---|
| Pericardiocentesis only |
| Indwelling pericardial catheter |
| Percutaneous balloon pericardiotomy |
| Subxiphoid pericardiotomy |
| Pleuropericardial window |
| Partial pericardiectomy |
| Wide anterior pericardiectomy |
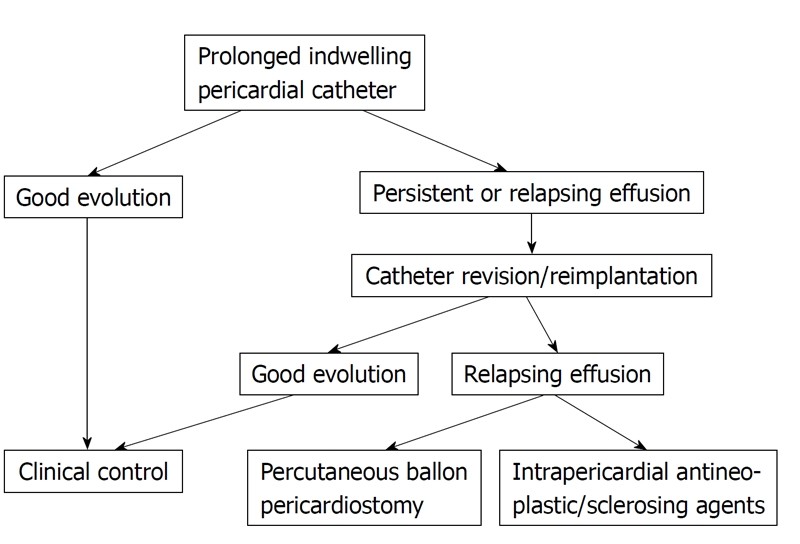
Neoplastic pericardial effusion management presents unique challenges, with treatment focused on tamponade relief and preventing fluid re-accumulation. Less invasive procedures are preferred, especially in advanced cases. While pericardiocentesis provides immediate relief, effusion recurrence is common. Indwelling pericardial catheters offer a higher success rate in preventing recurrence. Balloon pericardiotomy is another less invasive option, particularly for malignancy-related effusions.
Surgical drainage procedures, including pericardiectomy and pericardial window creation, are also effective but carry higher perioperative risks. In neoplastic pericardial effusion, a stepwise approach starting with indwelling catheters, followed by percutaneous pericardiotomy or sclerosing agents, and rarely surgical drainage, is often employed. Figure 3 summarizes a management strategy for neoplastic pericardial effusion. Recognizing and addressing potential effusive-constrictive pericarditis is also crucial in patients with persistent venous hypertension post-drainage, further refining the pericardial effusion diagnosis and treatment approach.
Figure 3: Management Strategy for Neoplastic Pericardial Effusion
Idiopathic Chronic Pericardial Effusion Management
Idiopathic chronic pericardial effusion, characterized by large effusions lasting over three months without a known cause, often presents asymptomatically. However, it carries a risk of unexpected tamponade. Medical therapies are generally ineffective. Pericardiocentesis is the initial treatment for tamponade and is also recommended prophylactically in asymptomatic patients. Repeat pericardiocentesis may be necessary for relapsing effusions. For persistent relapses after two pericardiocentesis procedures, wide anterior pericardiectomy is recommended, even in asymptomatic patients, demonstrating a proactive approach to managing this specific pericardial effusion diagnosis category.
Prognosis of Pericardial Effusion
The prognosis of pericardial effusion is highly dependent on the underlying etiology, underscoring the importance of accurate pericardial effusion diagnosis. Neoplastic pericardial effusion, particularly secondary to lung cancer with malignant cytology, carries a poor prognosis. Idiopathic/viral pericarditis has an excellent prognosis. Prognosis in tuberculous or purulent pericarditis depends on early diagnosis and treatment, while chronic idiopathic pericardial effusion has a generally good prognosis but with the potential risk of tamponade.
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48