Primary pericardial malignant mesothelioma (PPM) stands as an exceptionally rare and aggressive cancer, originating from the mesothelial cells lining the pericardium – the sac surrounding the heart. Its rarity, coupled with non-specific initial symptoms, makes “Pericardial Mesothelioma Diagnosis” a significant challenge for clinicians. Often, this diagnosis is only confirmed during surgery or, unfortunately, at autopsy. This article delves into the complexities of diagnosing pericardial mesothelioma, exploring the clinical presentations, advanced imaging techniques, and definitive pathological methods crucial for identifying this elusive malignancy.
Understanding Pericardial Mesothelioma: A Diagnostic Perspective
Pericardial mesothelioma’s rarity is striking, observed in a mere 0.0022% of nearly 500,000 autopsies. Within primary heart and pericardial tumors, it represents a small fraction (2-3%), overshadowed by angiosarcomas and rhabdomyosarcomas. This infrequency is a primary factor contributing to diagnostic delays.
While asbestos exposure is strongly linked to pleural and peritoneal mesothelioma, its association with PPM is less clear, adding another layer of complexity to risk assessment and diagnosis. Other potential risk factors, though less defined, include radiation exposure and certain viral infections. In many cases, like the 68-year-old patient detailed in the original case study, a clear etiology remains unidentified, emphasizing the idiopathic nature of many PPM occurrences.
Unraveling the Symptom Puzzle: Clinical Presentation and Initial Suspicion
The insidious onset of PPM further complicates early “pericardial mesothelioma diagnosis”. Symptoms often mimic common cardiac conditions, including:
- Dyspnea (shortness of breath): Frequently triggered by exertion, reflecting impaired cardiac function.
- Chest Pain: Non-specific and variable, ranging from mild discomfort to more pronounced pain.
- Cough: Can be present, adding to the diagnostic ambiguity.
- Orthopnea (difficulty breathing when lying down): Indicating fluid accumulation and cardiac strain.
- Peripheral Edema (swelling in legs and ankles): A sign of fluid overload and potential heart failure.
- Unexplained Weight Loss and Malaise: Constitutional symptoms that are non-specific but should raise clinical suspicion in conjunction with cardiac symptoms.
These symptoms often arise due to pericardial effusion (fluid buildup around the heart) or tumor encroachment, leading to cardiac compression and dysfunction. Clinical presentations can vary, ranging from constrictive pericarditis (inflammation and thickening of the pericardium restricting heart function), pericardial effusion, cardiac tamponade (life-threatening compression of the heart due to fluid), to congestive heart failure.
Imaging Modalities: Guiding the Diagnostic Process
When clinical suspicion arises from the presented symptoms, imaging plays a pivotal role in the “pericardial mesothelioma diagnosis” pathway.
Echocardiography: Often the first-line cardiac imaging technique, echocardiography can reveal pericardial effusion and may detect pericardial masses. In the case study, it identified circumferential pericardial effusion and a hyperechoic mass in the posterior pericardium, prompting further investigation.
Computed Tomography (CT) Scan: CT scanning offers detailed anatomical visualization. Contrast-enhanced CT, as utilized in the case study (Figure 1), is crucial for characterizing pericardial masses, assessing their size, location, and any enhancement patterns suggestive of malignancy. CT can also reveal the extent of the disease, including pleural effusions and potential mediastinal involvement.
Magnetic Resonance Imaging (MRI): MRI provides superior soft tissue contrast, further aiding in delineating the pericardial mass from surrounding structures and assessing for invasion. It can be particularly helpful in complex cases or when CT findings are equivocal.
Positron Emission Tomography/Computed Tomography (PET/CT): PET/CT, while not always the primary diagnostic tool, can be valuable in assessing the metabolic activity of pericardial lesions. Increased radiotracer uptake in a pericardial mass can raise suspicion for malignancy and help differentiate between benign and malignant conditions.
Pathological Confirmation: The Gold Standard for Pericardial Mesothelioma Diagnosis
While imaging provides crucial clues, definitive “pericardial mesothelioma diagnosis” rests on pathological examination.
Pericardiocentesis and Cytology: Pericardiocentesis, the aspiration of pericardial fluid, can be performed under echocardiographic or CT guidance. Cytological analysis of the fluid may reveal malignant cells, but the diagnostic yield is often low. In the literature, malignant cells are found in only a minority of PPM cases through pericardial fluid cytology. While pericardial hyaluronic acid content can be elevated in mesothelioma, it is not a highly sensitive or specific diagnostic marker.
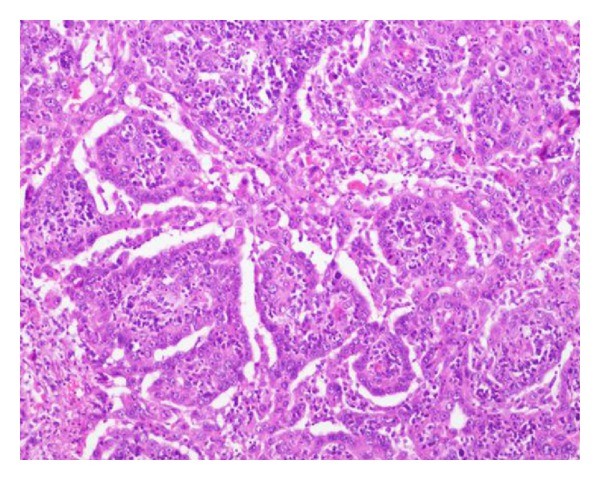
Surgical Biopsy and Histopathology: Surgical exploration and biopsy of the pericardial mass are frequently necessary to obtain sufficient tissue for definitive diagnosis. In the presented case, surgical resection provided the specimen for pathological evaluation. Histopathological examination, as seen in Figure 2, reveals characteristic features of mesothelioma, including pleomorphic malignant cells with epithelial appearance.
Immunohistochemistry: Immunohistochemical staining is critical for confirming the mesothelial origin of the tumor and differentiating PPM from other malignancies, particularly adenocarcinomas. Mesothelioma cells typically stain positive for markers like vimentin, calretinin, CK AE1/AE3, and CK7, while being negative for adenocarcinoma markers such as carcinoembryonic antigen (CEA). Figure 3 illustrates the immunohistochemical profile in the case study, demonstrating the positivity for key mesothelial markers.
Differential Diagnosis: Distinguishing PPM from Other Conditions
Accurate “pericardial mesothelioma diagnosis” necessitates differentiating it from other conditions that can mimic its presentation, including:
- Metastatic Cardiac Tumors: Metastases to the pericardium are far more common than primary PPM. Lung cancer, breast cancer, melanoma, and lymphoma are frequent sources. Clinical history and immunohistochemistry help differentiate.
- Primary Cardiac Sarcomas: Angiosarcoma and rhabdomyosarcoma, while also rare, are more frequent primary cardiac tumors. Histopathology and immunohistochemistry are essential for distinguishing these from PPM.
- Benign Pericardial Conditions: Pericarditis of various etiologies (viral, bacterial, idiopathic), pericardial cysts, and benign tumors must be considered and ruled out through a combination of imaging, clinical context, and sometimes biopsy.
Prognosis and Treatment Implications
The aggressive nature of PPM and challenges in achieving complete surgical resection contribute to a poor prognosis. The median survival time is often less than six months from diagnosis. While radical surgery may be attempted for localized disease, complete eradication is often not feasible. Chemotherapy and radiotherapy have limited efficacy in PPM.
Post-operatively, as shown in Figure 4, chest radiographs may demonstrate improved cardiac silhouette, but recurrence remains a significant concern, as seen in the described case where local recurrence led to the patient’s demise 27 months post-surgery.
Conclusion: Improving Pericardial Mesothelioma Diagnosis for Better Outcomes
“Pericardial mesothelioma diagnosis” remains a formidable challenge due to the tumor’s rarity and non-specific presentation. A high index of clinical suspicion, coupled with advanced imaging techniques and definitive pathological evaluation through surgical biopsy and immunohistochemistry, are crucial for accurate identification. Continued research into diagnostic biomarkers and improved therapeutic strategies are essential to improve outcomes for patients facing this devastating malignancy.
References
The authors declare that they have no conflict of interests.
[1] Patel J, Sheppard MN. Primary malignant pericardial mesothelioma: macroscopic and microscopic pathological features in 20 cases. Cardiovasc Pathol. 2004 Nov-Dec;13(6):297-303.
[2] Burke AP, Cowan D, Farb A, Li L, Smialek J, Virmani R. Primary sarcomas of the heart. Cancer. 1992 Jul 1;69(12):2814-21.
[3] Allen MS, Mathisen DJ. Primary pericardial mesothelioma. Semin Thorac Cardiovasc Surg. 1999 Jul;11(3):261-5.
[4] Butchart EG, Ashcroft T, Barnsley PA, Holden MP. Pericardial mesothelioma. Thorax. 1976 Aug;31(4):457-63.
[5] Armitage JO, Rostomily RC, Pettengell R, Levine AM. Primary pericardial mesothelioma presenting as a rapidly progressive lymphoma. Am J Med. 1984 Aug;77(2):349-52.
[6] Kumar V, Abbas AK, Fausto N, Aster JC. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Philadelphia, PA: Elsevier Saunders; 2014.
[7] Baumann F, Taeger D, Vogel J, et al. Association between genetic susceptibility, asbestos exposure, and malignant mesothelioma: a case-control study. Cancer Epidemiol Biomarkers Prev. 2012 Oct;21(10):1749-59.
[8] Doddoli C, Barlesi F, Giovanoli R, et al. Primary pericardial mesothelioma: a clinicopathologic study of 9 cases. Chest. 2003 Apr;123(4):1085-91.
[9] Plönes T, Schröder C, Boldt J, Kremer M, Wagner R. [Primary malignant mesothelioma of the pericardium. Case report and review of the literature]. Herz. 2002 Aug;27(5):501-7.
[10] Ordonez NG. Value of calretinin, WT1, mesothelin, CK5/6, and MOC-31 immunostaining in differentiating epithelioid mesothelioma from adenocarcinoma. Am J Surg Pathol. 2003 Nov;27(10):1283-91.