Pinpoint pupils, clinically known as miosis, refer to excessively constricted pupils, typically measuring 2 millimeters or less in diameter. While pupil size naturally fluctuates in response to light and emotional states, persistently small pupils can signal underlying health concerns that require careful differential diagnosis. For automotive experts, understanding the nuances of pinpoint pupils can be metaphorically extended to diagnosing complex vehicle issues – pinpointing the root cause from a range of possibilities. This article delves into the various causes of pinpoint pupils, offering a comprehensive guide for differential diagnosis.
Understanding Pinpoint Pupils (Miosis)
Pupils are the black circles in the center of your eyes, acting as apertures that regulate the amount of light reaching the retina. In healthy eyes, the iris muscles automatically adjust pupil size based on ambient light conditions. In bright light, pupils constrict to limit light entry, while in dim light, they dilate to maximize light intake. This dynamic response ensures optimal vision across varying environments. However, pupil size can also be influenced by other factors, including emotional responses and focus of vision (e.g., constriction when focusing on near objects).
Pinpoint pupils, or miosis, occur when the pupils remain abnormally constricted, often unresponsive to changes in light. While temporary constriction can be a normal physiological response, persistent or sudden onset of pinpoint pupils can be indicative of an underlying medical condition. Distinguishing between benign and pathological causes of miosis is crucial for accurate diagnosis and appropriate intervention.
Differential Diagnosis: 6 Key Causes of Pinpoint Pupils
When environmental or emotional factors are ruled out, pinpoint pupils warrant further investigation to identify potential underlying causes. Several medical conditions and external factors can lead to miosis. A systematic approach to differential diagnosis is essential to pinpoint the exact cause.
1. Substance Abuse: Opioid-Induced Miosis
Opioid abuse is a leading cause of pinpoint pupils. Drugs like heroin, fentanyl, and prescription painkillers in overdose amounts are potent constrictors of pupils. Opioid-induced miosis is a significant clinical sign, particularly in emergency situations, as it can indicate life-threatening opioid overdose. The mechanism involves opioids affecting the central nervous system, leading to pupillary constriction.
Besides opioids, other substances of abuse can also cause pinpoint pupils, including:
- Sedatives: Barbiturates, benzodiazepines, and other sedatives, when abused, can lead to miosis.
- Clonidine: While medically prescribed, abuse or misuse can result in pinpoint pupils.
- GHB (Gamma-hydroxybutyrate): This central nervous system depressant can cause pupillary constriction.
- Nicotine: Tobacco and nicotine products can cause miosis, although less pronounced than opioids.
- PCP (Phencyclidine): While often associated with dilated pupils, PCP can paradoxically cause pinpoint pupils in some cases.
In differential diagnosis, considering substance abuse as a cause requires evaluating patient history, clinical context, and potentially toxicology screening. The presence of other signs of intoxication or withdrawal can further support this diagnosis.
2. Prescription Drug Side Effects: Medication-Induced Miosis
Numerous prescription medications can induce pinpoint pupils as a side effect. This is particularly relevant when considering differential diagnosis, as patients may be taking these medications for legitimate medical reasons. Common culprits include:
- Cholinergic Drugs (Alzheimer’s Medications): Medications like Pyridostigmine, used to treat Alzheimer’s disease and myasthenia gravis, increase acetylcholine levels, leading to pupillary constriction.
- Antipsychotics (e.g., Zyprexa, Haloperidol, Quetiapine): Certain antipsychotic medications, particularly neuroleptics, can have anticholinergic or other mechanisms that result in miosis.
- Hypertension Medications (e.g., Clonidine, Tetrahydrozoline): Some drugs used to treat high blood pressure, such as clonidine and tetrahydrozoline (found in some eye drops), can cause pupillary constriction.
- Glaucoma Eye Drops: Certain prescription eye drops used to manage glaucoma work by constricting the pupil (miotics) to improve fluid drainage from the eye.
- Antidepressants (Noradrenergic Serotonergic Antidepressants): Some antidepressants like Mirtazapine can have side effects that include pupillary changes.
When pinpoint pupils are observed, a thorough review of the patient’s medication list is crucial. Differentiating medication-induced miosis involves correlating the onset of miosis with the initiation or dosage change of a potentially causative drug.
3. Toxin Exposure: Environmental and Chemical Agents
Exposure to certain toxins, particularly insecticides, herbicides, and nerve agents, can induce significant miosis. Organophosphates and carbamates, common in insecticides, inhibit acetylcholinesterase, leading to an excess of acetylcholine and subsequent pupillary constriction. Nerve agents, such as those used in chemical warfare, also exert their toxic effects by similar mechanisms, causing rapid and pronounced miosis.
In cases of suspected toxin exposure, history of potential exposure (e.g., agricultural work, chemical spills, or intentional poisoning) is critical for differential diagnosis. Other symptoms of cholinergic poisoning, such as SLUDGE syndrome (Salivation, Lacrimation, Urination, Defecation, Gastrointestinal distress, Emesis) and muscle weakness, may accompany pinpoint pupils.
4. Diseases Affecting the Iris and Neurological Pathways
Certain diseases can directly affect the iris or the neurological pathways controlling pupillary size, resulting in miosis.
- Anterior Uveitis (Iritis): Inflammation of the iris (anterior uveitis) can cause pupillary constriction and pain. This condition is often associated with autoimmune diseases like rheumatoid arthritis, as well as infections and other systemic illnesses.
- Systemic Diseases: Various systemic diseases have been linked to miosis, although the mechanisms are not always fully understood. These include:
- Rheumatic diseases (e.g., rheumatoid arthritis)
- Skin diseases
- Gastrointestinal problems
- Lung diseases
- Infections like mumps, rubella, and neurosyphilis
Differential diagnosis in these cases involves considering the patient’s overall medical history, associated symptoms, and ophthalmological examination findings. Anterior uveitis, for example, typically presents with eye pain, redness, and light sensitivity in addition to miosis.
5. Horner Syndrome: Disruption of Sympathetic Nerve Supply
Horner syndrome is a neurological condition characterized by a triad of symptoms resulting from disruption of the sympathetic nerve pathway to the eye and face. The classic triad includes:
- Miosis (Pinpoint Pupil): Due to unopposed parasympathetic activity.
- Ptosis (Drooping Eyelid): Weakness of the muscle that elevates the upper eyelid.
- Anhidrosis (Absence of Sweating): On the affected side of the face.
Horner syndrome can be caused by various underlying conditions, including stroke, tumors in the brain or neck, spinal cord injury, and carotid artery dissection. Crucially, Horner syndrome typically presents with unilateral miosis (pinpoint pupil in only one eye), which is a key differentiating feature from causes that usually produce bilateral miosis.
Differential diagnosis of Horner syndrome involves neurological examination to identify the complete triad of symptoms and neuroimaging (e.g., MRI) to determine the underlying cause and location of the sympathetic pathway disruption.
6. Trauma to the Eye or Brain: Structural and Neurological Damage
Trauma to the eye or brain can directly damage the iris muscles or the neurological pathways controlling pupillary reflexes, leading to miosis. Eye trauma, such as direct injury to the iris, can cause permanent pupillary constriction. Brain trauma, particularly injuries affecting the brainstem or sympathetic pathways, can also result in miosis, which may be temporary or permanent depending on the severity and location of the injury.
In cases of traumatic miosis, a history of eye or head trauma is paramount. Neurological assessment and imaging studies are essential to evaluate the extent of the injury and guide management.
Diagnosis and Management of Pinpoint Pupils
Diagnosing the cause of pinpoint pupils involves a comprehensive approach:
- Medical History: Detailed questioning about medications, substance use, toxin exposure, past medical conditions, and recent trauma.
- Physical Examination: General physical assessment and focused neurological and ophthalmological examinations. Pupil examination includes assessing size, reactivity to light (both direct and consensual reflexes), and symmetry.
- Ancillary Tests: Depending on the suspected cause, further investigations may include:
- Toxicology screening (urine or blood drug tests)
- Blood tests to assess for infections or systemic diseases
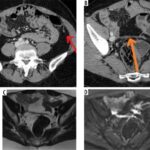
- Neuroimaging (CT or MRI of the brain and neck) to evaluate for Horner syndrome or structural brain lesions
- Ophthalmological examination to rule out anterior uveitis or other eye conditions
Management of pinpoint pupils is directed at treating the underlying cause. There is no direct treatment to “cure” miosis itself.
- Substance Abuse: Management involves detoxification, addiction rehabilitation programs, and addressing potential opioid overdose with naloxone.
- Medication Side Effects: Review and potential adjustment of medications by the prescribing physician. In some cases, alternative medications may be necessary.
- Toxin Exposure: Decontamination and supportive medical care, potentially including antidotes for specific toxins.
- Diseases: Treatment of the underlying systemic or ocular disease by the appropriate specialist (e.g., rheumatologist, ophthalmologist, infectious disease specialist).
- Horner Syndrome and Trauma: Management depends on the underlying cause and may involve surgical intervention, medication, or supportive care.
Prevention and When to Seek Medical Attention
Preventing pinpoint pupils primarily involves avoiding known risk factors:
- Responsible Medication Use: Adhering to prescribed dosages and discussing potential side effects with your doctor.
- Avoiding Substance Abuse: Seeking help for substance use disorders.
- Occupational Safety: Using appropriate protective gear when working with toxins (e.g., insecticides, herbicides).
- Regular Medical Check-ups: Routine eye examinations and medical assessments can help detect underlying health issues early.
Seek immediate medical attention if you experience sudden onset of pinpoint pupils, especially if accompanied by:
- Changes in vision
- Eye pain or discomfort
- Headache, dizziness, or confusion
- Nausea or vomiting
- Breathing difficulties
- Changes in skin color (e.g., blue-tinged lips or fingertips)
While pupils may naturally become slightly smaller with age, sudden or unexplained pinpoint pupils are a significant clinical sign that warrants prompt medical evaluation to determine the underlying cause and initiate appropriate management. Just as automotive experts meticulously diagnose complex vehicle malfunctions, a thorough differential diagnosis of pinpoint pupils is essential for effective medical care.
References
This content is for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
- [Original article source – nvisioncenters.com] (https://www.nvisioncenters.com/eye-conditions/pinpoint-pupils-miosis/) (Adapted from the provided source article)
- MedlinePlus – Pinpoint Pupils
- American Academy of Ophthalmology – Uveitis
- National Institute of Neurological Disorders and Stroke – Horner Syndrome