Papillary thyroid carcinoma (PTC) stands as the most prevalent form of thyroid cancer, recognized for its follicular cell differentiation and unique nuclear characteristics. While generally carrying a favorable prognosis, early and accurate Ptc Diagnosis is paramount for effective management and optimal patient outcomes. This comprehensive guide, crafted for healthcare professionals and those seeking in-depth knowledge, delves into the multifaceted aspects of PTC diagnosis, aiming to enhance understanding and diagnostic precision.
Understanding Papillary Thyroid Carcinoma
PTC, an epithelial malignancy, typically manifests as an irregular solid mass within the thyroid gland, although cystic variations can occur. A hallmark of PTC is its propensity for lymphatic invasion, with approximately 10% of patients exhibiting metastatic disease at the time of initial diagnosis. Despite this, the overall prognosis remains positive for the majority, particularly for individuals under 45 years of age. This article will explore the critical components of PTC diagnosis, from initial presentation to advanced diagnostic techniques.
Etiology and Risk Factors in PTC Diagnosis
Identifying risk factors is crucial in assessing patient susceptibility and can guide diagnostic strategies. Several factors have been linked to an increased risk of PTC development:
Radiation Exposure: A Significant Risk Factor
Exposure to ionizing radiation is a well-established risk factor for PTC. This includes:
- Childhood Radiation Therapy: Low-dose radiation to the head and neck during childhood, historically used for benign conditions, is associated with an elevated PTC risk. The latency period can be extensive, ranging from 10 to over 30 years post-exposure.
- High-Dose Medical Radiation: Therapeutic doses of radiation (>2000 cGy) for malignant diseases also contribute to increased PTC risk.
- Environmental Radiation: Events like the Chernobyl nuclear accident have demonstrated a significant surge (3- to 75-fold) in PTC incidence in affected regions, especially among younger populations.
Genetic Predisposition
Genetic syndromes can predispose individuals to PTC:
- Familial Adenomatous Polyposis Syndromes: Gardner syndrome, Werner syndrome, and Carney complex type 1 are among the associated syndromes.
- Familial PTC: Approximately 5% of PTC cases are familial, potentially exhibiting a more aggressive disease progression.
Other Contributing Factors
- Iodine Intake: Higher PTC rates are observed in regions with high dietary iodine intake.
- Preexisting Benign Thyroid Disease: Individuals with existing benign thyroid conditions may have an increased risk.
- Obesity: Emerging evidence suggests a correlation between overweight and obesity and an increased incidence of thyroid cancer.
Epidemiology of PTC: Diagnostic Implications
PTC’s epidemiological profile has significant implications for diagnosis and screening considerations:
- Prevalence: PTC constitutes the majority of thyroid cancers, accounting for 80-85% of cases.
- Incidence Increase: Data from the SEER database reveals a notable rise in PTC incidence, from 4.8 to 14.9 per 100,000 between 1975 and 2012. This increase may be partly attributed to enhanced diagnostic scrutiny and detection methods.
- Overdiagnosis Concerns: The medical community acknowledges the potential for thyroid cancer overdiagnosis, primarily due to the incidental discovery of thyroid microcarcinomas during routine imaging. This raises questions about overtreatment and the need for refined diagnostic and management approaches.
- Demographics: PTC predominantly affects middle-aged adults, with a female-to-male ratio of 3:1 and a median age at diagnosis of 50 years. While less common in children, PTC remains the most frequent pediatric thyroid malignancy, with a higher prevalence in White populations compared to Black populations.
Pathophysiology: Molecular Insights for Diagnosis
Understanding the molecular underpinnings of PTC is increasingly relevant for diagnosis and targeted therapies. Key genetic alterations include:
- Chromosomal Rearrangements: Rearrangements involving the RET protooncogene, NTRK1, and MET gene overexpression are implicated in PTC pathogenesis.
- BRAF Gene Mutations: Mutations, particularly BRAFV600E, are frequently observed and have prognostic significance. BRAFV600E mutation status can influence disease aggressiveness and response to therapy.
- Radiation Association: A strong link between radiation exposure and PTC development is firmly established, highlighting the role of environmental and medical history in risk assessment.
Histopathological Diagnosis of PTC: The Gold Standard
Histopathology remains the cornerstone of PTC diagnosis. Characteristic features observed in PTC tissue samples are essential for definitive diagnosis:
Gross Examination
Macroscopic examination reveals:
- Appearance: PTC typically presents as an invasive neoplasm with ill-defined borders, firm consistency, and a granular, whitish cut surface.
- Calcifications: Calcifications may be present within the tumor mass.
- Size Variability: Tumor size is variable, with an average diameter of 2-3 cm.
- Classification: PTC is categorized based on size and invasiveness:
- Minimal/Occult/Microcarcinoma: Tumors ≤1.5 cm, non-invasive, often incidental findings.
- Intra-thyroid: Tumors >1.5 cm, confined to the thyroid gland without extra-thyroidal extension.
- Extra-thyroid: Tumors extending beyond the thyroid capsule, invading adjacent structures.
Microscopic Hallmarks: Key to PTC Diagnosis
Microscopic examination is critical for confirming PTC diagnosis. The two cardinal features are:
- Papillae Formation: Papillae, consisting of a fibrovascular core covered by neoplastic epithelium, are a defining architectural feature. Papillae morphology can vary (long, short, branched, tightly packed), and the stromal component is also variable.
- Nuclear Features: Nuclear changes are diagnostic hallmarks, irrespective of architectural patterns. These include:
- Nuclear Enlargement and Elongation: Crowded and overlapping nuclei.
- Irregular Nuclear Contours: Deviations from smooth nuclear outlines.
- Chromatin Clearing (Orphan Annie Eye Nuclei): Central clearing of chromatin with peripheral margination.
Microscopic view of Papillary Thyroid Carcinoma cells demonstrating characteristic Orphan Annie eye nuclei, a key feature in PTC diagnosis.
4. **Micronucleoli:** Multiple small nucleoli located near the nuclear membrane.
5. **Nuclear Grooves:** Two-dimensional infoldings of the nuclear membrane.
6. **Intranuclear Cytoplasmic Pseudo-inclusions:** Cytoplasmic invaginations into the nucleus.
7. **Psammoma Bodies:** Concentrically laminated calcifications, although not always present.Immunohistochemistry in PTC Diagnosis
Immunohistochemistry plays a limited role in primary PTC diagnosis but can be valuable in specific contexts, such as metastatic disease. PTC cells typically exhibit strong and diffuse immunoreactivity for:
- Keratins: Cytokeratin, CK7.
- Thyroid Markers: Thyroglobulin, TTF1, PAX8.
- Variable Markers: HBME-1, Galectin-3, S100 protein, CITED1, CK19 show variable expression patterns.
Clinical Presentation and Initial Evaluation for PTC Diagnosis
The clinical presentation of PTC often guides initial diagnostic steps:
History and Physical Examination
- Asymptomatic Thyroid Mass: The most common presentation is a painless thyroid nodule, often without systemic symptoms.
- Cervical Lymphadenopathy: Regional lymph node enlargement may be present in up to 27% of patients at diagnosis, frequently in the ipsilateral neck. Lateral neck involvement can occur in some cases.
- Hoarseness and Dysphagia: These symptoms, present in about 20% of cases, may indicate recurrent laryngeal nerve involvement or tracheal compression, suggesting more advanced disease.
- Palpation Findings: Examination typically reveals a firm, hard, painless lesion, often less than 5 cm in size, potentially fixed and with irregular borders.
Fine Needle Aspiration (FNA): A Primary Diagnostic Tool
FNA is frequently the initial diagnostic procedure for suspected PTC:
- Specimen Characteristics: FNA samples from PTC are usually cellular, displaying papillary structures, monolayer sheets, and three-dimensional cell clusters in a background of watery or thick colloid, nuclear debris, macrophages, and stromal fragments.
- Cell Morphology: Tumor cells are enlarged, elongated, or oval, with eosinophilic cytoplasm and the characteristic nuclear features of PTC (enlargement, elongation, chromatin clearing, grooves, pseudo-inclusions).
- Follicular Cell Arrangement: Enlarged follicular cells arranged in monolayer sheets and follicular groups within a colloid background are also typical findings.
Laboratory Tests: Limited Role in Initial PTC Diagnosis
Thyroid function tests are generally not helpful in diagnosing PTC, as most patients present with normal thyroid function. However, they are important for overall patient assessment and post-treatment monitoring.
Radiographic Evaluation: Imaging Modalities in PTC Diagnosis
Imaging plays a crucial role in PTC diagnosis, staging, and management:
- Thyroid Scans: PTC typically appears as “cold” (hypofunctioning) nodules on thyroid scans, although rarely, “hot” (hyperfunctioning) nodules can occur.
- Ultrasound: The Imaging Modality of Choice: Ultrasound is the primary imaging technique for PTC evaluation. Sonographic features suggestive of PTC include:
- Hypoechoic or isoechoic solid nodule.
- Irregular or poorly defined margins.
- Microcalcifications (highly specific for PTC).
- Taller-than-wide shape.
- Disorganized internal vascularity.
- Ultrasound is also essential for guiding FNA biopsies of suspicious nodules and lymph nodes.
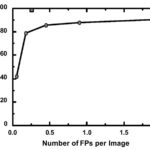
- Advanced Imaging (CT, MRI, FDG-PET/CT): These modalities may be used to:
- Assess extra-thyroidal extension.
- Evaluate substernal masses.
- Detect recurrent tumors.
- Improve diagnostic accuracy in complex cases.
Differential Diagnosis of PTC
Distinguishing PTC from other thyroid conditions is crucial for accurate diagnosis. The differential diagnosis includes:
- Reactive Changes Post-FNA: FNA procedures can induce nuclear changes (enlargement, chromatin clearing, micronucleoli) that mimic PTC. Careful interpretation in the context of clinical history is essential.
- Severe Chronic Lymphocytic Thyroiditis (Hashimoto’s Thyroiditis): Inflammation-related atypia in Hashimoto’s thyroiditis can exhibit nuclear features resembling PTC.
- Benign Nodular Conditions: Adenomatoid nodules, diffuse hyperplasia, dyshormonogenetic goiter, and follicular adenoma need to be considered.
- Other Thyroid Malignancies: Follicular thyroid carcinoma, medullary thyroid carcinoma.
- Metastatic Tumors: Metastasis to the thyroid from other primary cancers should be excluded.
Staging and Prognosis: Implications for PTC Diagnosis and Management
Staging systems are essential for risk stratification and management planning in PTC. The most commonly used staging systems vary based on patient age:
Staging for Patients Under 45 Years
- Stage I: Any T, any N, M0 (Localized to the thyroid, any nodal involvement, no distant metastasis).
- Stage II: Any T, any N, M1 (Any tumor size, any nodal involvement, distant metastasis present).
Staging for Patients Over 45 Years
- Stage I: T1, N0, M0 (Tumor ≤2 cm, no nodal or distant metastasis).
- Stage II: T2, N0, M0, and T3 (Tumor 2-4 cm or confined to thyroid, no nodal or distant metastasis).
- Stage III: T4, N0, M0, and any T, N1, M0 (Tumor >4 cm or extra-thyroidal extension, or nodal metastasis in the neck, no distant metastasis).
- Stage IV: Any T, any N, M1 (Any tumor size, any nodal involvement, distant metastasis present).
Prognostic Factors
While PTC generally has a favorable prognosis, certain factors can indicate a less favorable outcome:
- Older Age at Diagnosis
- Large Tumor Size
- Extra-thyroidal Extension
- Male Sex
- Aggressive Histological Variants: Tall cell variant, diffuse sclerosis variant, solid variant, follicular variant.
- Vascular Invasion and Aneuploidy
Conclusion: Enhancing PTC Diagnosis for Improved Outcomes
Accurate and timely PTC diagnosis is critical for effective management and favorable patient outcomes. A multifaceted approach encompassing clinical evaluation, advanced imaging, fine needle aspiration, and histopathological analysis is essential. Continued research into molecular markers and refined diagnostic techniques promises to further enhance our ability to detect and manage PTC, ultimately improving the lives of individuals affected by this prevalent thyroid malignancy.