Diagnosing rheumatoid arthritis (RA) can be a complex process, particularly in the early stages of the disease. It’s important to understand that there isn’t a single, definitive test for RA. Blood tests, for instance, can yield varying results, being negative in individuals with RA and positive in others without the condition. Similarly, in early RA, X-rays might appear completely normal. Therefore, a skilled rheumatologist plays a crucial role in carefully evaluating all available information to determine if a patient has rheumatoid arthritis.
Beyond a thorough medical history and physical examination, several diagnostic tools and criteria are utilized in the Ra Criteria Diagnosis process. Let’s delve into these key aspects:
Blood Tests in RA Diagnosis
When rheumatoid arthritis is clinically suspected, specific laboratory tests are essential to support the diagnosis. These tests primarily look for particular antibodies and inflammatory markers in the blood.
Rheumatoid Factor (RF)
Rheumatoid factor (RF) is an antibody found in approximately 80% of individuals with rheumatoid arthritis. However, it’s crucial to note that around 20% of RA patients do not have this antibody, and their diagnosis is established based on other criteria. Furthermore, false positive RF results can occur in healthy individuals and in association with other conditions such as bacterial endocarditis, hepatitis C, chronic liver disease, sarcoidosis, or even aging.
Anti-Citrullinated Peptide Antibody (ACPA or anti-CCP)
Anti-citrullinated peptide antibody (ACPA), also known as anti-CCP, is another antibody present in about 70% of people with rheumatoid arthritis. ACPA is considered more specific for RA diagnosis compared to rheumatoid factor. The presence of ACPA strongly suggests RA.
It’s important to remember that some individuals can have rheumatoid arthritis even with negative RF and CCP tests. These cases are termed “seronegative” RA. Conversely, the presence of RF and/or CCP antibodies is often associated with a more aggressive disease course.
Inflammatory Markers and Other Lab Abnormalities
Beyond specific antibodies, other laboratory findings can be indicative of RA. Elevated inflammatory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are commonly observed in people with rheumatoid arthritis, reflecting the inflammation within the body. Anemia of chronic disease is also a frequent finding. Additionally, some individuals with RA may have a low positive anti-nuclear antibody (ANA).
Imaging Studies for Rheumatoid Arthritis
Imaging techniques play a vital role in visualizing joint damage and inflammation, aiding in the diagnosis and monitoring of rheumatoid arthritis.
X-rays
X-rays are routinely performed when rheumatoid arthritis is suspected. X-rays of the hands and feet are particularly common as these areas are frequently affected by RA. In early RA, X-rays may not show any abnormalities. However, as the disease progresses, characteristic RA-related changes may become visible on X-rays. These include:
- Thinning of the bone around a joint (periarticular osteopenia)
- Narrowing of the joint space
- Subluxation (partial dislocation) and joint deformity
- Erosions (bone damage) around the joint
X-rays are also used throughout RA treatment to assess the response to therapy and to monitor for disease progression.
Magnetic Resonance Imaging (MRI)
MRI is sometimes employed in diagnosing rheumatoid arthritis, especially when RA is strongly suspected despite negative antibody tests and normal X-rays. MRI is more sensitive than X-rays in detecting early signs of RA, such as synovitis (inflammation of the joint lining) and bony erosions, which are typical of RA. The visualization of these features on MRI can help confirm the diagnosis.
Ultrasound
Ultrasound is increasingly popular for both the diagnosis and ongoing management of RA. It is a relatively inexpensive, non-invasive, and readily available procedure that can be performed in a clinic setting. Studies have demonstrated that ultrasound can be as sensitive as MRI in detecting joint inflammation and erosions. However, the accuracy of ultrasound findings depends significantly on the expertise of the person performing the examination.
Joint Fluid Analysis
Examining the fluid from a swollen joint (joint aspiration or arthrocentesis) can be valuable in differentiating rheumatoid arthritis from other conditions like osteoarthritis, gout, or infection. In contrast to the fluid from an osteoarthritic joint, RA joint fluid will exhibit significant inflammation, characterized by a high white blood cell count. The presence of uric acid crystals in the joint fluid would suggest gout as the underlying diagnosis instead of RA.
Classification Criteria for Rheumatoid Arthritis
Classification criteria for RA were initially developed for research purposes but are widely used by clinicians to aid in confirming a diagnosis of rheumatoid arthritis. These criteria provide a standardized framework for diagnosis.
1987 ACR/EULAR Criteria
The initial classification criteria were established in 1987 through a joint effort by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR). These criteria required the presence of symptoms for at least 3 months and the fulfillment of at least 4 out of 7 criteria to classify a patient as having RA.
The 1987 ACR/EULAR classification criteria for rheumatoid arthritis:
| Criteria | Description |
|---|---|
| 1. Morning stiffness | Morning stiffness in and around the joints, lasting at least 1 hour |
| 2. Arthritis of ≥3 joints | The qualified joints include proximal interphalangeal (PIP), metacarpophalangeal (MCP), wrist, elbow, knee, ankle, and metatarsophalangeal (MTP) joints |
| 3. Arthritis of hand joints | At least one joint area swollen in a wrist, MCP, or PIP joint |
| 4. Symmetric arthritis | Simultaneous involvement of the same joint areas on both sides of the body |
| 5. Rheumatoid nodules | Subcutaneous nodules, which are lumps under the skin, over bony prominences, extensor surfaces (like the back of the forearm), or around joints |
| 6. Rheumatoid factor | Positive rheumatoid factor blood test |
| 7. Radiographic changes | X-ray findings including erosions (bone damage) or periarticular demineralization (thinning of bone around the joints) |
However, the 1987 criteria were recognized as being less effective for diagnosing early RA. Patients with early rheumatoid arthritis might not yet exhibit rheumatoid nodules or radiographic changes, leading to diagnostic delays.
2010 ACR/EULAR Criteria
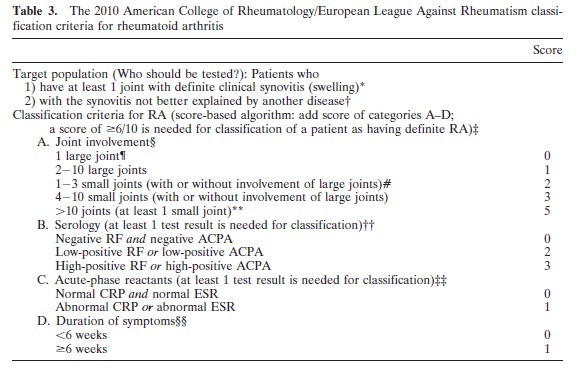
Recognizing the need for earlier diagnosis, the ACR/EULAR introduced revised rheumatoid arthritis classification criteria in 2010. These newer criteria are more sensitive for early RA diagnosis. A total score of 6 points or more (out of a possible 10) is required to meet the 2010 criteria for RA.
This criteria is particularly useful for establishing an early diagnosis of RA. It is acknowledged that some individuals with long-standing RA might meet the 1987 criteria but not the 2010 criteria. In the 2010 criteria, “large joints” refer to shoulders, elbows, hips, knees, and ankles, while “small joints” encompass metacarpophalangeal (MCP) joints, proximal interphalangeal (PIP) joints, 2nd-5th metatarsophalangeal joints, thumb interphalangeal joints, and wrists.
 Understanding the 2010 ACR/EULAR Rheumatoid Arthritis Classification Criteria
Understanding the 2010 ACR/EULAR Rheumatoid Arthritis Classification Criteria
Image: A visual representation of the 2010 ACR/EULAR rheumatoid arthritis classification criteria, highlighting the point system and categories.
From: Arthritis & Rheumatism; vol 62, No 6, September 2010, pp 2569-2581
The Importance of Early RA Diagnosis
Early diagnosis of rheumatoid arthritis is critical because the primary goal in managing RA is to control symptoms and prevent irreversible joint damage. Extensive research over the past years has clearly demonstrated that the earlier rheumatoid arthritis diagnosis is made and treatment is initiated, the better the long-term outcomes for patients. Prompt diagnosis and treatment significantly improve the chances of effectively managing the disease and minimizing its impact on quality of life. Therefore, seeking timely medical evaluation and pursuing ra criteria diagnosis when symptoms arise is of utmost importance.
See also:
Treatment of rheumatoid arthritis
Reference: (Original article source – comprehensiverheumatology.com)
