I. Introduction
Abdominal pain is a frequently encountered complaint in primary care settings, presenting a considerable diagnostic challenge for healthcare practitioners. While numerous causes of abdominal pain are benign, a subset indicates severe, potentially life-threatening conditions necessitating prompt and accurate diagnosis. The right upper quadrant (RUQ) is a specific area of the abdomen where pain can originate from a variety of organs, including the liver, gallbladder, duodenum, pancreas, right kidney, and colon. Therefore, understanding the differential diagnosis of right upper quadrant pain is crucial for primary care physicians to ensure timely and effective patient management and prevent adverse outcomes. This article focuses specifically on providing a structured approach to the differential diagnosis of right upper quadrant pain in the primary care setting.
II. Pathophysiology of Right Upper Quadrant Pain
Pain in the right upper quadrant can arise from various mechanisms, mirroring general abdominal pain pathophysiology, but specifically relating to the organs located in this region. These mechanisms include inflammation, obstruction, distension, ischemia, and referred pain.
Inflammation: Inflammatory processes are common culprits of RUQ pain. Conditions like cholecystitis (inflammation of the gallbladder), hepatitis (liver inflammation), and pancreatitis (inflammation of the pancreas head, which can radiate to the RUQ) directly irritate pain receptors.
Obstruction: Blockages within the biliary tree, such as gallstones in the common bile duct, can cause significant RUQ pain. Obstruction leads to distension and increased pressure within the affected organ, stimulating pain receptors. Similarly, obstruction in the duodenum or right kidney can manifest as RUQ pain.
Distension: Hepatomegaly (liver enlargement) due to various causes including heart failure or hepatitis, or distension of the gallbladder or duodenum can stretch the organ capsules and trigger pain.
Ischemia: Reduced blood flow to organs in the RUQ, such as the liver or gallbladder (e.g., in ischemic hepatitis or gallbladder torsion), can cause severe pain due to tissue hypoxia and the release of pain-inducing chemicals.
Referred Pain: Pain originating from organs outside the RUQ, such as the right lower lobe pneumonia or myocardial ischemia (though less common), can sometimes be referred to the right upper quadrant due to shared nerve pathways.
Understanding these pathophysiological mechanisms is fundamental in approaching the differential diagnosis of right upper quadrant pain and guides the history taking and physical examination process.
III. Differential Diagnosis of Right Upper Quadrant Pain in Primary Care
The differential diagnosis for right upper quadrant pain is broad and encompasses a range of conditions from benign to life-threatening. In primary care, it is essential to systematically consider and rule out serious conditions while efficiently diagnosing and managing more common ailments. Here are key categories and examples to consider:
Biliary Tract Disease:
- Cholecystitis: Inflammation of the gallbladder, often due to gallstones. Presents with constant RUQ pain, often radiating to the back or right shoulder, associated with nausea, vomiting, and fever. Murphy’s sign is often positive.
- Biliary Colic: Transient obstruction of the cystic duct or common bile duct by gallstones. Characterized by episodic, severe RUQ pain that comes in waves, lasting from minutes to hours, often after fatty meals.
- Ascending Cholangitis: Infection of the bile ducts, usually due to obstruction. Presents with Charcot’s triad (RUQ pain, fever, jaundice) and can be life-threatening.
Liver Disease:
- Hepatitis (Viral, Alcoholic, Drug-induced): Liver inflammation causing RUQ discomfort, fatigue, jaundice, and elevated liver enzymes. Pain is typically mild to moderate and may be associated with hepatomegaly.
- Liver Abscess: A collection of pus in the liver, causing RUQ pain, fever, chills, and weight loss.
- Hepatomegaly: Liver enlargement due to various causes (heart failure, fatty liver disease, tumors) can cause a sensation of fullness or mild RUQ pain.
- Budd-Chiari Syndrome: Blockage of hepatic venous outflow, leading to liver congestion and RUQ pain, ascites, and hepatomegaly.
Pancreatic Disease:
- Pancreatitis (Head of Pancreas): Inflammation of the pancreas, where pain can radiate to the RUQ, epigastric area, or back. Characterized by severe, constant pain, often worsened by lying supine and relieved by sitting forward. Nausea, vomiting, and abdominal distension are common.
Gastrointestinal Conditions:
- Duodenal Ulcer: Ulcers in the duodenum can cause epigastric or RUQ pain, often related to meals (pain improves with food, then worsens 2-3 hours after).
- Gastritis/Duodenitis: Inflammation of the stomach or duodenum can cause upper abdominal discomfort, including the RUQ.
- Irritable Bowel Syndrome (IBS): While primarily causing lower abdominal pain, IBS can sometimes manifest with upper abdominal discomfort, including RUQ pain, associated with altered bowel habits.
- Right-sided Colitis (Inflammatory Bowel Disease): Inflammation of the right side of the colon (ascending colon) can present with RUQ pain and diarrhea, potentially bloody.
Renal Conditions:
- Pyelonephritis (Right Kidney): Kidney infection can cause flank pain radiating to the RUQ, along with fever, chills, dysuria, and urinary frequency.
- Nephrolithiasis (Right Kidney Stones): Kidney stones passing through the right ureter can cause severe, colicky flank pain that may radiate to the RUQ, groin, and back.
Musculoskeletal and Abdominal Wall Pain:
- Abdominal Wall Strain: Muscle strain in the abdominal wall can cause localized RUQ pain, often worsened by movement or palpation. Carnett’s test may be positive.
- Costochondritis: Inflammation of the cartilage connecting ribs to the sternum can cause chest or upper abdominal pain that can mimic RUQ pain.
- Herpes Zoster (Shingles): Reactivation of varicella-zoster virus can cause a painful vesicular rash along a dermatomal distribution, which if involving the T9-T12 dermatomes, can present as RUQ pain.
Other Conditions:
- Right Lower Lobe Pneumonia: Inflammation of the right lower lung lobe can sometimes cause referred pain to the RUQ, especially in elderly patients.
- Right Pleural Effusion/Pleurisy: Inflammation or fluid buildup in the pleura surrounding the right lung can cause sharp RUQ pain that worsens with breathing.
This extensive differential highlights the importance of a systematic approach to history taking and physical examination to narrow down the possibilities and reach an accurate diagnosis.
IV. History Taking for Right Upper Quadrant Pain
A thorough history is paramount in evaluating RUQ pain. Using mnemonics like PQRST and PHRASED, as mentioned in the original article, can be helpful. Specifically tailored to RUQ pain, important historical features include:
- Pain Characteristics (PQRST):
- P (Provoking/Palliating factors): What makes the pain worse or better? (e.g., fatty foods worsen biliary colic/cholecystitis, antacids may relieve duodenal ulcer pain).
- Q (Quality): What does the pain feel like? (e.g., colicky pain in biliary colic, constant and sharp in cholecystitis, burning in duodenal ulcer).
- R (Region/Radiation): Where is the pain located? Does it radiate? (RUQ, radiation to back/shoulder in biliary disease).
- S (Severity): How severe is the pain on a scale of 1-10?
- T (Timing): When did the pain start? Is it constant or intermittent? How long does it last? (e.g., biliary colic episodes are typically time-limited).
- Associated Symptoms:
- Nausea and Vomiting: Common in biliary and pancreatic disease.
- Fever and Chills: Suggestive of infection (cholecystitis, cholangitis, pyelonephritis, liver abscess).
- Jaundice: Indicates biliary obstruction or liver disease.
- Changes in Urine and Stool: Dark urine and pale stools in biliary obstruction, hematuria in renal stones/infection.
- Appetite and Weight Loss: May suggest chronic conditions like malignancy or chronic liver disease.
- Bowel Habits: Diarrhea (colitis, infection), constipation (less specific but relevant in general abdominal assessment).
- Past Medical History:
- Gallstones or Biliary Disease: Previous episodes increase the likelihood of recurrence.
- Liver Disease (Hepatitis, Cirrhosis): Predisposes to liver-related RUQ pain.
- Pancreatitis: Risk factor for recurrent pancreatitis.
- Diabetes: Increased risk of gallbladder disease and infections.
- Medications: Hepatotoxic drugs, NSAIDs (gastritis/duodenal ulcer).
- Alcohol History: Alcoholic hepatitis or pancreatitis.
- Social and Family History:
- Family history of gallstones, liver disease, or inflammatory bowel disease.
- Travel history: Exposure to hepatitis viruses or parasitic infections.
By meticulously gathering historical information focused on these key aspects, primary care physicians can significantly refine the differential diagnosis of RUQ pain.
V. Physical Examination for Right Upper Quadrant Pain
A focused physical examination is crucial to complement the history and guide further investigations. Key components in examining a patient with RUQ pain include:
- General Appearance and Vital Signs: Assess for signs of systemic illness (fever, tachycardia, hypotension – suggesting sepsis or severe infection).
- Abdominal Examination:
- Inspection: Look for distension, scars, jaundice.
- Auscultation: Bowel sounds (hyperactive in early obstruction, hypoactive or absent in peritonitis).
- Percussion: Liver span (hepatomegaly), tympany vs. dullness.
- Palpation:
- Light and Deep Palpation: Assess for tenderness, guarding, rigidity in the RUQ.
- Murphy’s Sign: Specific for cholecystitis. Performed by palpating deeply in the RUQ at the right costal margin while the patient takes a deep breath. A positive Murphy’s sign is indicated by inspiratory arrest due to pain as the inflamed gallbladder hits the examiner’s hand.
- Liver Palpation: Assess for hepatomegaly, tenderness, consistency.
- Palpation for Masses: Although less common, masses in the RUQ need to be considered.
- Carnett’s Test: To differentiate abdominal wall pain from visceral pain.
- Flank Tenderness: Assess for kidney tenderness, suggesting pyelonephritis or nephrolithiasis.
- Chest Examination: Auscultate lungs to rule out right lower lobe pneumonia or pleural effusion as a cause of referred RUQ pain.
- Rectal and Pelvic Examination: May be indicated based on clinical suspicion to rule out other pelvic or rectal pathologies, although less directly relevant to isolated RUQ pain.
Combining the findings from the physical examination with the patient’s history allows for a more targeted differential diagnosis and guides the selection of appropriate investigations.
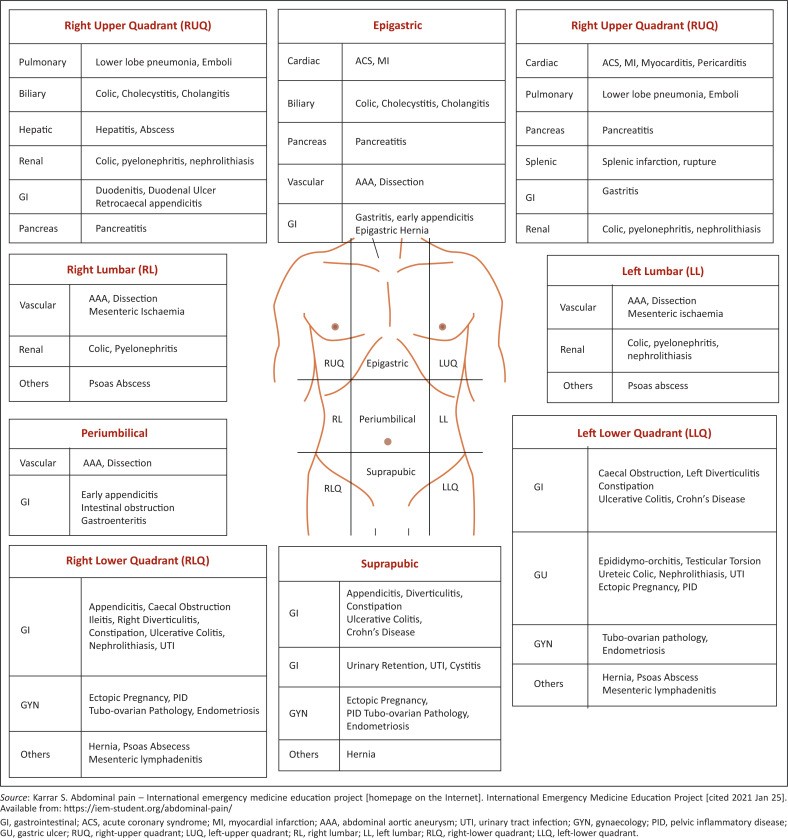
Figure 1: Anatomical localization of abdominal pain regions. Understanding the nine abdominal quadrants is helpful in pinpointing potential organ involvement in right upper quadrant pain.
VI. Investigations for Right Upper Quadrant Pain
Investigations are crucial to confirm the diagnosis and exclude serious pathology in RUQ pain. The choice of investigations is guided by the clinical suspicion based on history and physical examination.
Laboratory Investigations:
- Complete Blood Count (CBC): Elevated white blood cell count suggests infection (cholecystitis, cholangitis, pyelonephritis, liver abscess).
- Liver Function Tests (LFTs): Elevated AST, ALT, alkaline phosphatase, bilirubin indicate liver or biliary disease (hepatitis, cholecystitis, cholangitis, liver abscess, cholestasis).
- Amylase and Lipase: Elevated in pancreatitis.
- Renal Function Tests (Creatinine, BUN): Assess kidney function, especially if pyelonephritis or nephrolithiasis is suspected.
- Urinalysis: To detect urinary tract infection (pyelonephritis), hematuria (nephrolithiasis, pyelonephritis).
- Pregnancy Test (for females of childbearing age): To rule out ectopic pregnancy, although less likely to present as isolated RUQ pain.
Imaging Studies:
- Ultrasound: First-line imaging for RUQ pain. Highly sensitive for gallstones, cholecystitis, biliary obstruction, liver abscess, and can assess for hepatomegaly and pancreatic abnormalities. Rapid, non-invasive, and no radiation.
- CT Scan of the Abdomen: More comprehensive imaging, useful when ultrasound is inconclusive or to evaluate for pancreatitis, liver masses, abscesses, appendicitis (though less common in RUQ pain primarily), and other intra-abdominal pathologies. Involves radiation.
- HIDA Scan (Hepatobiliary Iminodiacetic Acid Scan): Used to assess gallbladder function and diagnose acute cholecystitis when ultrasound is equivocal.
- Abdominal X-ray: Limited role in RUQ pain, mainly to rule out bowel obstruction or perforation if suspected, or to identify calcified gallstones (not radiolucent stones).
Endoscopy:
- Upper Endoscopy (Esophagogastroduodenoscopy – EGD): May be considered if upper GI pathology (duodenal ulcer, gastritis/duodenitis) is suspected and not clarified by initial investigations.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): Therapeutic and diagnostic for biliary obstruction, cholangitis, and gallstone removal from the common bile duct, typically after initial diagnosis by less invasive methods.
The selection of investigations should be tailored to the individual patient based on the history, physical examination, and pre-test probability of different diagnoses. Ultrasound is often the initial imaging modality of choice for RUQ pain in primary care.
VII. Management of Right Upper Quadrant Pain in Primary Care
Initial management in primary care focuses on pain relief, symptomatic treatment, and determining the need for urgent referral.
Symptomatic Treatment:
- Analgesia: Pain relief is crucial. Paracetamol (acetaminophen) and NSAIDs (if not contraindicated) can be used for mild to moderate pain. Opioids may be necessary for severe pain while awaiting diagnosis and further management.
- Antiemetics: For nausea and vomiting associated with biliary or pancreatic disease.
- Antacids or Proton Pump Inhibitors (PPIs): For suspected gastritis or duodenal ulcer.
Further Management and Referral:
- Urgent Referral to Emergency Department: For patients with:
- Severe, unrelenting RUQ pain.
- Signs of sepsis (fever, tachycardia, hypotension).
- Jaundice.
- Vomiting and inability to tolerate oral intake.
- Suspected ascending cholangitis, acute cholecystitis, pancreatitis, liver abscess.
- Outpatient Referral to Specialist (Gastroenterologist, Surgeon): For patients with:
- Persistent RUQ pain despite initial management.
- Diagnostic uncertainty after initial investigations.
- Confirmed gallbladder disease requiring elective cholecystectomy.
- Chronic liver disease requiring specialist management.
- Conservative Management in Primary Care: For patients with:
- Mild, self-limiting RUQ pain, likely due to abdominal wall strain or mild gastritis.
- Known IBS with RUQ pain as part of their symptom complex.
- After exclusion of serious pathology and with appropriate follow-up.
Management strategies need to be individualized based on the underlying cause of RUQ pain and the patient’s overall clinical condition. Primary care physicians play a critical role in the initial assessment, symptomatic relief, and appropriate triage of patients with right upper quadrant pain.
VIII. Conclusion
Right upper quadrant pain is a common and diagnostically challenging presentation in primary care. A systematic approach incorporating a detailed history, focused physical examination, and judicious use of investigations is essential for accurate differential diagnosis. Primary care practitioners must be adept at recognizing serious conditions requiring urgent referral while effectively managing common causes of RUQ pain in the outpatient setting. Understanding the differential diagnosis of right upper quadrant pain and employing a structured diagnostic and management approach are crucial skills for providing optimal care to patients presenting with this complaint.