Introduction
The population aged 65 and older is rapidly growing, and with it, the prevalence of age-related diseases like cancer is also increasing. In fact, age is the most significant risk factor for cancer, making older adults disproportionately affected by this disease. In the United States alone, tens of millions of older adults are living with or have survived cancer, and this number is projected to double in the coming decades. Home health and hospice services are crucial components of healthcare for this population, offering vital support and treatment within the community setting. These services are designed to meet the complex needs of older adults facing various health challenges, including cancer. While hospice care is typically associated with end-of-life care for cancer patients, home health services play a broader role throughout the cancer care continuum. Understanding how these services are utilized and, importantly, The Primary Diagnosis In Home Care Is Most Related To for older cancer patients is essential for optimizing healthcare delivery and ensuring appropriate support for this vulnerable population. This article delves into the patterns of home health and hospice use among older adults with cancer, comparing them to their peers without cancer, and explores the factors that influence service utilization, shedding light on the critical role of primary diagnoses in shaping home care for this demographic.
Home Health and Hospice Utilization Patterns in Older Adults: Cancer vs. Non-Cancer
A significant disparity exists in the utilization of home health and hospice services between older adults with and without cancer. Research indicates that older cancer patients are considerably more likely to access home health services compared to those without cancer. Specifically, approximately 29% of older adults with cancer utilize home health services, whereas only about 7.8% of their non-cancer counterparts do so. Hospice service utilization also shows a marked difference, with around 10.7% of cancer patients using hospice, compared to less than 1% of non-cancer patients.
Interestingly, a substantial portion of home health utilization among cancer patients is not directly attributed to cancer as the primary admitting diagnosis. In fact, over half (51.4%) of cancer patients receiving home health services do not have cancer listed as the primary reason for admission. This suggests that while cancer undoubtedly increases the need for home-based care, the primary diagnosis in home care is most related to secondary conditions or complications arising from cancer or its treatment, rather than the cancer itself in many cases. This pattern holds true across various cancer types, indicating a broader trend beyond specific cancer sites. When examining utilization within specific timeframes, around 22.9% of newly diagnosed cancer patients use home health, and 24.4% of cancer patients in their last six months of life utilize home health services. These figures are still higher than those for non-cancer patients, underscoring the heightened need for home care in the cancer population, even when the primary diagnosis in home care is most related to factors other than the malignancy itself.
The Role of Primary Diagnosis in Home Care Admissions: Beyond Cancer
To further understand what primary diagnosis in home care is most related to for older adults, it’s crucial to examine the leading diagnoses for home health admissions in both cancer and non-cancer populations. For older adults without cancer, common primary diagnoses for home health include chronic conditions like diabetes mellitus, pressure ulcers, heart failure, hypertension, stroke, osteoarthritis, and chronic obstructive pulmonary disease (COPD). In contrast, while cancer patients also experience these conditions, the top diagnoses for their home health admissions (excluding cancer itself) are strikingly similar: diabetes mellitus, pressure ulcers, heart failure, stroke, osteoarthritis, COPD, and hypertension, along with conditions like open wounds and pneumonia.
This overlap in primary diagnoses suggests that the primary diagnosis in home care is most related to the management of common age-related chronic conditions, regardless of a cancer diagnosis. However, the higher utilization rates among cancer patients, even when the primary diagnosis is not cancer, point to the exacerbating effect of cancer and its treatment on these pre-existing conditions. Cancer or its therapy can worsen conditions like diabetes, heart failure, or COPD, leading to a greater need for home health services to manage these complexities. Therefore, while cancer may not always be the primary admitting diagnosis, it significantly contributes to the overall need for home care by increasing the burden of comorbid conditions and functional limitations in older adults. Understanding this interplay is crucial for healthcare providers to effectively address the primary diagnosis in home care is most related to the comprehensive care needs of older adults with cancer.
Predictors of Home Health and Hospice Service Use: Demographic Factors
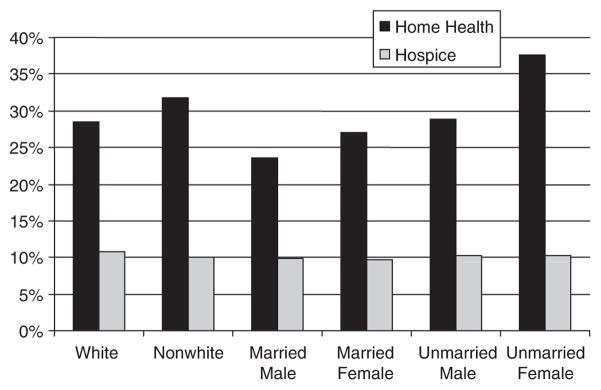
Beyond diagnosis, demographic factors also play a role in predicting home health and hospice utilization among older adults with cancer. Research indicates that race, sex, and marital status can influence the likelihood of accessing these services. For instance, white individuals tend to have lower expected rates of home health use but slightly higher hospice utilization compared to non-white individuals.
Unmarried women exhibit the highest expected rates of home health utilization, while unmarried men show the highest hospice utilization rates. Conversely, married men have the lowest home health utilization rates, and married women have the lowest hospice utilization rates. These disparities suggest that social support systems and caregiving availability, often linked to marital status and gender roles, influence the reliance on formal home health and hospice services.
For newly diagnosed cancer patients, hospice utilization is generally low across all demographic groups. However, non-white individuals and women, particularly unmarried women, tend to have higher expected utilization rates of home health care in the period following a new cancer diagnosis. In the context of end-of-life care, hospice utilization becomes more prominent, with white individuals showing higher hospice use and lower home health use compared to non-white individuals. Interestingly, married women demonstrate the highest utilization rates for both home health and hospice care in the terminal phase, while unmarried men exhibit the lowest home health utilization but also lower hospice utilization rates in this phase. These complex patterns highlight the interplay of demographic factors, disease stage, and care needs in shaping service utilization and underscore the importance of culturally sensitive and individualized care planning.
Implications and Future Directions: Optimizing Home Care for Older Adults with Cancer
The findings emphasize that older adults with cancer have a significantly higher need for home health and hospice services compared to their non-cancer counterparts. Crucially, a substantial portion of home health utilization in cancer patients is driven by conditions other than cancer itself, indicating that the primary diagnosis in home care is most related to the broader spectrum of age-related health issues exacerbated by cancer and its treatment. This “excess morbidity” experienced by cancer patients highlights the complex interplay between cancer, comorbid conditions, and functional decline in older adults.
Moving forward, several key questions and research directions emerge. Firstly, determining “appropriate utilization” of community-based services for older adults with cancer is paramount. Future studies should investigate the optimal role of home health and hospice in cancer care, exploring when and how these services should be utilized to maximize patient outcomes and quality of life. Comparing the effectiveness of home health versus hospice in managing symptoms, addressing emotional and spiritual needs, and reducing overall healthcare utilization and costs is essential. Furthermore, exploring the experiences of cancer survivors and their long-term healthcare needs, including community-based care, is a critical area for future research. Investigating geographical variations and differences between fee-for-service and managed care models in home health and hospice utilization can also inform policy and practice improvements. Ultimately, a deeper understanding of what primary diagnosis in home care is most related to for older adults with cancer, coupled with insights into service utilization patterns and predictors, will pave the way for more effective and patient-centered home-based care delivery for this growing population.
Conclusion
In conclusion, this analysis reveals that older adults with cancer exhibit significantly higher utilization of home health and hospice services compared to those without cancer. While hospice utilization aligns with end-of-life care needs, a considerable portion of home health use among cancer patients is not primarily due to cancer itself. Instead, the primary diagnosis in home care is most related to the management of comorbid conditions and treatment-related sequelae. Demographic factors like race, sex, and marital status further influence service utilization patterns, highlighting the need for tailored and equitable care approaches. Future research should focus on defining optimal utilization models and addressing the complex care needs of older adults with cancer in the community setting, ensuring that they receive the right care, at the right time, and in the most appropriate setting.