Tuberous sclerosis complex (TSC) is a rare genetic disorder that leads to the growth of non-cancerous tumors in various organs, including the brain, skin, kidneys, heart, eyes, and lungs. Early and accurate diagnosis of tuberous sclerosis is crucial for effective management and improving patient outcomes. This article delves into the diagnosis of tuberous sclerosis, outlining the methods, challenges, and the importance of timely detection.
What is Tuberous Sclerosis Complex?
Tuberous sclerosis complex is a genetic condition characterized by the development of benign tumors throughout the body. These tumors, or lesions, can affect multiple organ systems, leading to a wide range of symptoms. In the brain, TSC manifests as cortical tubers, subependymal nodules (SENs), and subependymal giant cell astrocytomas (SEGAs). Understanding the nature of these lesions is fundamental to diagnosing TSC and managing its neurological impact.
Alt text: Brain MRI showing cortical tubers and subependymal nodules, characteristic brain lesions in tuberous sclerosis complex diagnosis.
Recognizing the Signs: Symptoms as Diagnostic Clues
The symptoms of TSC are highly variable, differing significantly from person to person depending on the organs affected and the severity of the condition. Symptoms can emerge in infancy or childhood, but in some cases, they may not become apparent until later in life. Recognizing these symptoms is the first step in considering a diagnosis of tuberous sclerosis. Common symptoms that prompt diagnostic investigation include:
- Seizures: Epilepsy is a frequent neurological manifestation of TSC. This can include infantile spasms, focal seizures, and tonic-clonic seizures. The presence of different seizure types, especially in children, is a significant indicator.
- Kidney Issues: Kidney problems such as cysts and angiomyolipomas are common. While often asymptomatic, large angiomyolipomas can cause pain, internal bleeding, or kidney dysfunction. Detection of these kidney lesions during imaging studies is a key diagnostic finding.
- Developmental Delays and TAND: TSC-associated neuropsychiatric disorders (TAND) encompass a spectrum of cognitive, behavioral, and psychiatric conditions. Developmental delays, learning disabilities, ADHD, autism spectrum disorder (ASD), anxiety, and aggression are all within the TAND spectrum and can point towards a TSC diagnosis.
- Skin Manifestations: Distinctive skin features are strong visual clues for TSC diagnosis. These include:
- Ash leaf spots: White or lighter patches of skin, often best seen under a Wood’s lamp.
- Facial angiofibromas: Raised red or darker bumps on the face, typically appearing in a butterfly distribution.
- Shagreen patches: Areas of thick, pebbled skin usually on the lower back or nape of the neck.
- Ungual or subungual fibromas: Small growths around or under the fingernails and toenails.
- Lung Lesions: Lymphangioleiomyomatosis (LAM) is a lung disorder associated with TSC, primarily affecting women. Symptoms range from breathlessness to being asymptomatic, and detection often occurs during imaging for other reasons.
Alt text: Close-up of a child’s face showing facial angiofibromas, a characteristic skin finding aiding in tuberous sclerosis diagnosis.
Diagnostic Process: Confirming Tuberous Sclerosis
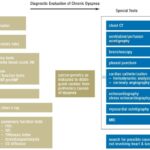
Diagnosing TSC involves a comprehensive approach, integrating clinical evaluation, family history, and various diagnostic tests. The diagnostic process aims to identify the characteristic features of TSC across different organ systems.
Clinical Examination and Symptom Review
A thorough clinical examination is the initial step in diagnosing TSC. This includes a detailed review of the patient’s symptoms, developmental history, and a careful physical examination looking for the hallmark skin findings and other signs of TSC. Family history is also important to assess for potential inherited cases.
Imaging Techniques: Visualizing Internal Lesions
Imaging plays a critical role in confirming TSC diagnosis and assessing the extent of organ involvement.
- MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) Scans: These are crucial for visualizing brain lesions like cortical tubers, SENs, and SEGAs. MRI is generally preferred for brain imaging due to its superior soft tissue resolution. CT scans may be used in certain situations. These scans help identify the characteristic brain abnormalities associated with TSC.
- Ultrasound: Renal ultrasound is used to detect kidney cysts and angiomyolipomas. It is a non-invasive and effective method for screening the kidneys in individuals suspected of having TSC.
- Echocardiogram (EKG): An echocardiogram can detect cardiac rhabdomyomas, a type of heart tumor associated with TSC, especially in infants.
Alt text: Abdominal CT scan revealing kidney angiomyolipomas, benign tumors in the kidneys, a key diagnostic indicator for tuberous sclerosis.
Genetic Testing: Identifying the Genetic Basis
Genetic testing can confirm the diagnosis of TSC by identifying mutations in the TSC1 or TSC2 genes. While clinical criteria are often sufficient for diagnosis, genetic testing can be particularly useful in:
- Atypical presentations: When clinical findings are suggestive but not definitive.
- Prenatal diagnosis: In families with a known history of TSC.
- Confirming sporadic cases: To differentiate from phenocopies or other conditions.
- Genetic counseling: To assess recurrence risk and inform family planning.
It’s important to note that a negative genetic test does not entirely rule out TSC, as some mutations may be missed by current testing methods or TSC can occur due to mosaicism.
Diagnostic Criteria for Tuberous Sclerosis Complex
The diagnosis of TSC is often based on established diagnostic criteria, which are categorized into major and minor features. Meeting a certain number of major and minor criteria, or having a positive genetic test, can confirm a TSC diagnosis. These criteria are regularly updated as medical understanding evolves.
Differential Diagnosis: Ruling Out Other Conditions
When considering a diagnosis of tuberous sclerosis, it’s important to differentiate it from other conditions that may present with similar symptoms. These include:
- Neurofibromatosis type 1 (NF1): NF1 shares some skin findings with TSC but has distinct features and genetic causes.
- Hypomelanosis of Ito: This condition also presents with hypopigmented skin lesions, but lacks other systemic features of TSC.
- Isolated epilepsy or autism: While seizures and autism are common in TSC, they can also occur independently. A comprehensive evaluation is needed to determine if they are part of a broader TSC presentation.
Importance of Early and Accurate Diagnosis
Early diagnosis of tuberous sclerosis complex is paramount for several reasons:
- Early Intervention: Prompt diagnosis allows for timely initiation of treatments to manage symptoms like seizures and developmental delays, potentially improving long-term outcomes.
- Surveillance and Monitoring: Once diagnosed, individuals with TSC require regular monitoring for the development and progression of tumors in various organs. Early diagnosis sets the stage for proactive surveillance.
- Genetic Counseling and Family Planning: Accurate diagnosis enables genetic counseling for families, providing information about inheritance patterns and recurrence risks, aiding in family planning decisions.
- Access to Support and Resources: A confirmed diagnosis connects patients and families with support networks, advocacy organizations like the TSC Alliance, and valuable resources for managing the condition.
Advances in TSC Diagnosis and Research
Ongoing research continues to refine diagnostic methods and deepen our understanding of TSC. Advances include:
- Improved genetic testing: More comprehensive genetic testing panels are enhancing the detection rate of TSC1 and TSC2 mutations.
- Biomarker discovery: Research into biomarkers aims to develop more sensitive and specific diagnostic tools for TSC, potentially even before symptoms are fully manifest.
- Longitudinal studies: Natural history studies are providing valuable insights into the progression of TSC across the lifespan, informing diagnostic and management strategies.
Conclusion: Empowering Lives Through Diagnosis
Diagnosing tuberous sclerosis complex is a multifaceted process requiring careful clinical evaluation, advanced imaging, and often genetic testing. Early and accurate diagnosis is not just about naming a condition; it’s about unlocking access to appropriate medical care, support systems, and ongoing research advancements. By understanding the diagnostic pathways for tubular sclerosis, we empower individuals and families to navigate this complex condition with greater knowledge and hope for improved quality of life.
For further information and support, resources like the TSC Alliance and the NIH GARD Information Center are invaluable. Continued research and awareness are essential to improving the lives of those affected by tuberous sclerosis complex.