Introduction
Ulnar-sided wrist pain presents a significant diagnostic challenge, not only in general medicine but also particularly for automotive technicians. The intricate anatomy of the ulnar wrist, often described as the “black box” of the wrist, encompasses numerous potential pain generators stemming from both acute injuries and chronic degenerative conditions. For professionals in automotive repair, the constant use of hand tools and repetitive wrist motions can exacerbate or initiate ulnar wrist pain. Therefore, a thorough understanding of the differential diagnosis of ulnar sided wrist pain is crucial for effective self-care, seeking appropriate medical advice, and understanding potential work-related injuries. This article aims to provide a comprehensive guide to Ulnar Sided Wrist Pain Differential Diagnosis, emphasizing the anatomical complexities and diagnostic approaches relevant to automotive technicians and beyond.
Anatomy of the Ulnar Wrist: Key Structures for Differential Diagnosis
To effectively navigate the differential diagnosis of ulnar sided wrist pain, a solid grasp of the relevant anatomy is essential. The ulnar aspect of the wrist is a complex region comprising bones, joints, ligaments, tendons, neurovascular structures, and the triangular fibrocartilage complex (TFCC).
Bones and Joints of the Ulnar Wrist
The distal ulna, a primary bony structure in this region, consists of the ulnar head and the ulnar styloid. The ulnar styloid, a projection from the distal ulna, serves as a critical attachment point for several key structures, including the extensor carpi ulnaris (ECU) subsheath and superficial fibers of the TFCC and ulnocarpal ligaments [1]. At the base of the styloid, the fovea, a vascularized, non-cartilaginous area, anchors the radioulnar and ulnocarpal ligaments [1]. The distal ulna articulates with the TFCC and the distal radius at the distal radioulnar joint (DRUJ). The sigmoid notch of the radius, exhibiting a greater curvature than the ulnar head, facilitates a wide range of motion at the DRUJ. This joint allows for rotation about the forearm axis, dorsal-palmar translation, and proximal-distal translation. Variations in DRUJ bony morphology, such as flat face, ski slope, “C” type, and “S” type shapes, significantly impact joint stability [1].
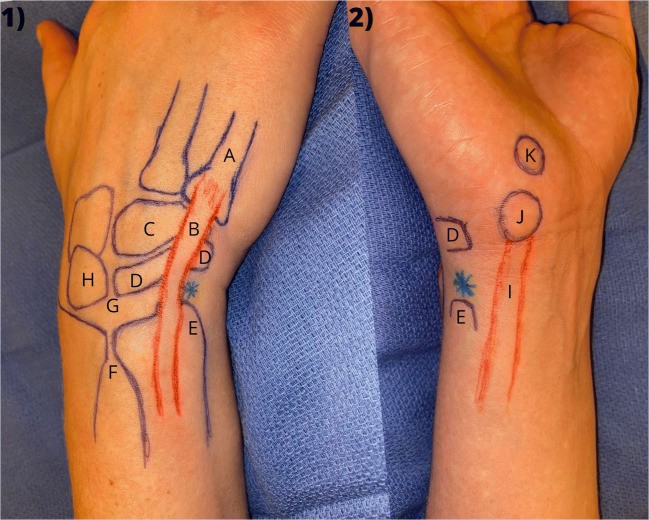 Surface anatomy of wrist demonstrating key landmarks for ulnar sided wrist pain differential diagnosis.
Surface anatomy of wrist demonstrating key landmarks for ulnar sided wrist pain differential diagnosis.
The carpus, interacting with the radius and ulna, enables balanced wrist motion. The lunate, articulating with the scaphoid and triquetrum, is the cornerstone of the carpal arch. A type 2 lunate, a normal anatomical variant with a narrow facet for hamate articulation, might offer some stability in cases of scapholunate tears [2]. This variation is important to consider during imaging interpretation. The triquetrum articulates with the hamate, pisiform, and TFCC. The helicoidal triquetrohamate joint is vital for midcarpal motion, allowing rotation and minimal translation [2]. The hamate, articulating with the lunate, triquetrum, and the fourth and fifth metacarpals, features a volar hook that acts as a pulley for finger flexors [1]. The pisiform, a sesamoid bone within the flexor carpi ulnaris (FCU) tendon, forms the pisotriquetral joint, a synovial joint [2]. The pisiform also serves as an attachment point for the abductor digiti quinti and transverse carpal ligament.
Ligaments, Tendons, and the TFCC in Ulnar Wrist Pain
A dense network of intrinsic and extrinsic ligaments supports the ulnar wrist. Intrinsic ligaments, located within the carpus, include the capitohamate, lunotriquetral (LT), and triquetrohamate ligaments. The LT ligament, crucial for wrist stability, has dorsal, volar, and proximal components, with the volar portion being the strongest [2, 3]. Extrinsic ligaments, connecting the carpus to the forearm, include the ulnotriquetral and ulnolunate ligaments, which stabilize the distal ulna and carpus and merge with the TFCC volar margin [2, 3]. The volar and dorsal radioulnar ligaments stabilize the DRUJ, forming a triangle around the articular disk at the distal ulna. DRUJ stability is further enhanced by the deep foveal TFCC, interosseous membrane, extensor retinaculum, ECU subsheath, sigmoid notch bony morphology, and dynamic stabilization from the ECU tendon [1].
The FCU and ECU tendons are the primary tendons on the ulnar wrist. The ECU tendon, running in the sixth dorsal compartment, is critical for wrist extension and ulnar deviation [4]. Its dorsal displacement during supination and wrist extension is clinically relevant [2]. The FCU tendon, located ulnar to the ulnar nerve and artery, inserts on the pisiform and blends with the palmar carpal ligament.
Neurovascular Structures of the Ulnar Wrist
The ulnar nerve and artery traverse Guyon’s canal, a critical anatomical tunnel in the ulnar wrist. The canal’s borders are defined by structures like the volar carpal ligament, transverse carpal ligament, pisiform, pisohamate ligament, abductor digiti minimi, and hook of hamate [2]. The ulnar nerve bifurcates within Guyon’s canal into deep and superficial branches. Nerve compression at different zones within the canal results in varying clinical presentations, affecting motor and sensory functions differently [2]. The superficial ulnar artery’s proximity to the hook of the hamate makes it vulnerable in hamate hook fractures [2].
Differential Diagnosis of Ulnar Sided Wrist Pain: A Categorized Approach
Diagnosing ulnar sided wrist pain requires a systematic approach due to the wide range of potential pathologies. A comprehensive differential diagnosis should consider osseous, ligamentous, tendinous, vascular, neurologic, and miscellaneous causes, as outlined in Table 1, adapted from Shin et al. [3] and other resources [2, 5, 6].
Table 1: Differential Diagnosis of Ulnar-Sided Wrist Pain
This table offers a detailed list of potential diagnoses for patients experiencing ulnar-sided wrist pain, categorized to facilitate a systematic diagnostic process. Each category and specific diagnosis should be carefully considered during patient evaluation.
| Osseous | Ligamentous | Tendinous | Vascular | Neurologic | Miscellaneous |
|---|---|---|---|---|---|
| Fractures: hamate (hook, body), pisiform, triquetrum (dorsal avulsion), lunate, 4th/5th metacarpal base, ulnar styloid, distal ulna, distal radius | TFCC tear (peripheral vs foveal) | ECU tendon subluxation, dislocation, tendinopathy, rupture | Hypothenar hammer syndrome | C8–T1 cervical radiculopathy | Benign or malignant neoplasms |
| Fracture sequelae: nonunions, malunions | Carpal, midcarpal, DRUJ instability | FCU tendinitis | Ulnar artery thrombosis | Brachial plexopathy | Psychological conditions |
| Degenerative conditions: PT joint, midcarpal (triquetrohamate), 4th/5th CMC, DRUJ | Ligament tears: LT, CH, UL, TC, TH, UT split | EDM tendinitis | Hemangioma | Thoracic outlet syndrome | |
| Kienböck disease | LT dissociation | Raynaud syndrome | Cubital tunnel syndrome | ||
| Incomplete coalition of LT joint | Thoracic outlet syndrome | Guyon’s canal syndrome | |||
| Ulnar impingement vs impaction | Peripheral vascular disease | Dorsal sensory ulnar nerve neuritis | |||
| Hamatolunate impingement syndrome | Cardiac emboli | CRPS | |||
| Ulnar styloid impaction syndrome | Neuroma | ||||
| Hamate Arthrosis Lunotriquetral ligament Tear (HALT) lesion | |||||
| Madelung’s deformity |
Clinical History in Ulnar Wrist Pain Diagnosis
A thorough clinical history is paramount in narrowing the differential diagnosis for ulnar wrist pain. Details of any recent or past traumatic injuries, including the mechanism of injury, are crucial. Exacerbating factors that reproduce the pain can be highly informative. For instance, pain aggravated by ulnar deviation, wrist extension, or weight-bearing through the ulnocarpal joint (like pushing up from a chair) can point towards specific diagnoses. Cohen-Tanugi has previously detailed additional historical and injury patterns that aid in diagnosis [6••]. For automotive technicians, understanding the specific tools and tasks that provoke pain is especially relevant.
Physical Examination of the Ulnar Wrist: A Step-by-Step Guide
A systematic approach to the physical examination of the ulnar wrist is essential for consistent and accurate assessments. The recommended position involves the examiner sitting opposite the patient, with the patient’s elbow flexed and resting on a table in an “arm wrestling” posture [3, 5, 6].
Observation
Initial observation involves comparing the affected wrist to the contralateral side, noting any wounds, scars, ecchymosis, swelling, erythema, skin or nail changes, and differences in digital perfusion. Visible abnormalities can suggest specific diagnoses [6••]. Palmar carpal sag may indicate LT tears, though it’s more commonly seen with DRUJ disruptions. A prominent ulnar head can result from chronic foveal TFCC injuries and DRUJ instability. Swelling along the ulnar wrist might indicate tenosynovitis, infection, or gout. Intrinsic hand muscle atrophy or finger clawing can suggest ulnar nerve pathology.
Palpation
Palpation begins with identifying the pisiform, distal to the ulnar wrist flexion crease, which may be painful in pisotriquetral (PT) arthritis or pisiform fractures. The FCU tendon is palpated proximally from the pisiform and becomes prominent with finger abduction and extension. To palpate the hook of hamate, place your thumb over the pisiform and direct the tip towards the ring finger; deep palpation will reveal the hook. This is crucial for assessing hook of hamate fractures. The ulnar styloid, a dorsal ulnar prominence, is more palpable in neutral or pronated positions. Moving volarly from the styloid, the fovea is found in the groove between the ECU and FCU. Foveal pain suggests peripheral TFCC or ulnotriquetral ligament split tears. Distal to the fovea lies the triquetrum. The dorsal triquetrum, radial to the ECU tendon, is an important palpation point for dorsal triquetral avulsion fractures. The ECU tendon is best visualized in forearm supination with finger abduction, which also facilitates instability assessment. In pronation, the ECU aligns straight with the arm. Palpate distally along the fifth metacarpal shaft from the ECU insertion. The lunotriquetral (LT) interval is palpated distal to the DRUJ between the 4th and 5th dorsal compartments with the wrist flexed 30 degrees [3, 6].
Range of Motion (ROM) and Grip Strength
Assess active and passive wrist ROM, comparing to the contralateral side. Normal ROM includes 80 degrees flexion, 70 degrees extension, 90 degrees supination, and 90 degrees pronation [8]. Isolate wrist pronation/supination by having the patient adduct shoulders and keep elbows tucked. Note any motion limitations, pain, clicking, locking, or snapping. Grip strength testing assesses patient effort and strength. The ratio of injured to uninjured side grip strength correlates with DASH scores, providing objective evaluation [9]. While bilateral grip testing is used, no single test reliably predicts effort sincerity [10].
Provocative Maneuvers and Special Tests for Ulnar Wrist Pain
Numerous provocative maneuvers and special tests aid in differentiating ulnar wrist pathologies. Table 2 lists these maneuvers and their corresponding pathologies.
Table 2: Provocative Maneuvers for Ulnar-Sided Wrist Pain Differential Diagnosis
This table outlines various provocative tests employed in the assessment of ulnar-sided wrist pain. For each test, the table specifies what constitutes a positive result and the associated pathology indicated by a positive test.
| Test | Positive Result | Indicative Pathology |
|---|---|---|
| Ulnocarpal stress test | Pain | Ulnocarpal impaction, central TFCC tear |
| Press test | Pain | Ulnar-sided wrist pain, possible TFCC pathology |
| Hook of hamate pull test | Pain | Hook of hamate fracture |
| Pisiform tracking test/PT grind test | Pain | PT joint pathology |
| LT ballottement test | Pain or laxity | LT tear |
| Regan shuck test | Pain or laxity | LT tear |
| Kleinman shear test | Pain | LT tear |
| DRUJ compression test | Pain | DRUJ arthritis |
| Piano key/DRUJ ballottement test | Pain or laxity | DRUJ instability |
| Synergy test | Sharp pain, Subluxation/dislocation | ECU tendonitis, ECU tendon instability |
| Ulnar fovea sign | Tenderness | TFCC pathology |
| Midcarpal shift test | Painful clunk | Midcarpal instability |
The ulnocarpal stress test involves axial pressure on the ulnarly deviated wrist during pronation and supination. Pain indicates a positive test, sensitive but not specific for ulnar wrist pathology, including ulnar impaction [11]. The hook of hamate pull test, by Wright, involves resisted flexion of the ring and small fingers in ulnar deviation. Pain suggests a hook of hamate fracture [12]. The pisiform triquetral grind test assesses PT arthritis by gripping and shucking the pisiform while stabilizing the dorsal wrist [6••].
Three tests assess the lunotriquetral (LT) joint. The LT ballottement test applies radial pressure to the pisiform while stabilizing the wrist; pain or laxity suggests LT tears [13], though it lacks specificity. The Regan shuck test grasps and shucks the triquetrum and pisiform unit dorsally to palmarly. The Kleinman shear test applies pressure between thumbs on the pisiform and dorsal lunate, after ruling out PT arthritis [13, 6••].
DRUJ pain may indicate instability, arthritis, or both. The DRUJ compression test involves compressing the distal radius and ulna, eliciting pain in DRUJ arthritis. The piano key or DRUJ ballottement test assesses instability by shucking the distal ulna volarly and dorsally while stabilizing the radius, performed in supination, neutral, and pronation [14].
ECU instability is assessed via the synergy test. Patients fully supinate and abduct the thumb and long finger against resistance, synergistically firing the ECU. Sharp pain indicates ECU tendonitis, while subluxation or dislocation suggests instability [15]. The ECU tendon can also be assessed with an “ice cream scoop” motion simulation [6••].
TFCC evaluation includes the ulnar fovea sign, where foveal tenderness is 95.2% sensitive and 86.5% specific for TFCC pathology [16]. The ulnocarpal stress test, moving an ulnarly deviated wrist volarly to dorsally with axial compression, may elicit pain in ulnar carpal impaction or central TFCC tears [3].
The midcarpal shift test, performed in pronation and ulnar deviation with volar pressure on the capitate and axial load on metacarpals, is positive for midcarpal instability if a painful clunk occurs [6••].
Diagnostic injections, into tendon sheaths like the ECU sheath or specific joints, can help identify or exclude pathologies [3].
Radiographic Evaluation in Diagnosing Ulnar Sided Wrist Pain
Radiographic evaluation is crucial in diagnosing ulnar sided wrist pain, starting with standard radiographs and progressing to advanced imaging as needed.
Radiography: Initial Imaging Modality
Standard posteroanterior (PA) and lateral radiographs are the initial step for all patients with ulnar-sided wrist pain. PA views should be examined for Gilula’s lines and ulnar variance. Gilula’s lines disruption typically indicates carpal subluxation or dislocation [17]. Ulnar variance refers to the relative lengths of the distal ulna and radius. Positive ulnar variance occurs when the distal ulna extends beyond the radial articular surface. Negative ulnar variance, sometimes linked to Kienbock’s disease, is when the distal ulna is proximal to the radial articular surface [2].
Lateral views assess carpal instability using scapholunate, capitolunate, and lunotriquetral angles [3]. Oblique 30-degree pronation and supination views evaluate the dorsal and volar ulnar wrist, respectively [3]. Ulnar deviation views can reveal LT instability, while pronated grip views show ulnocarpal abutment. The carpal tunnel view, a tangential X-ray with 35-degree wrist extension, is useful for examining the hook of hamate and PT joint.
Fluoroscopy or live X-ray imaging can detect abnormal carpal motion and dynamic instability, such as the midcarpal instability “catch up” clunk [3].
Advanced Imaging: CT, MRI, and Ultrasound
Computed tomography (CT) provides detailed carpal bone evaluation, superior for identifying occult fractures of the pisiform, hamate, and ulnar styloid. CT is also useful for assessing DRUJ instability via bilateral wrist CTs in neutral, pronation, and supination [18]. “Dynamic” or “4D” CT visualizes 3D bony wrist interactions [19]. CT arthrography aids in locating TFCC tears [20].
MRI is now standard for soft tissue and occult fracture evaluation. Wrist MRI requires high resolution and signal-to-noise ratios [5]. 3-Tesla (T) MRI offers better image quality and sensitivity for ulnar wrist pathologies than 1.5-T MRI [21, 22], though sensitivity varies with radiologist experience [3]. MRI also assesses lunate vascularity and cystic/signal changes in ulnocarpal impaction [23].
MRI arthrography, using intravenous (indirect) or intra-articular (direct) contrast, enhances ulnar wrist anatomy visualization. Contrast in the DRUJ after TFCC contrast injection indicates a TFCC tear [24], representing abnormal communication rather than synovitis [5].
Radionuclide imaging or triple bone scans can identify wrist inflammation, occult fractures, osteonecrosis, and osteomyelitis [3], but are not specific and less frequently used.
Ultrasound is increasingly used for ulnar wrist pain, offering portability, no radiation, and low cost. It is user-dependent and limited for bony pathologies, but valuable for tendinous pathologies like ECU subsheath tears and preoperative tendon rupture planning [5, 25, 26].
Recent Developments in Ulnar Wrist Pain Diagnosis
Recent advancements in ulnar wrist pain diagnosis focus on diagnostic imaging and arthroscopy. Dry wrist arthroscopy (DWA) is gaining popularity for evaluating and treating ulnar-sided pathologies, avoiding soft tissue distension that can mask ligamentous tears and cause post-operative pain [27]. DWA limitations include inability to use thermal probes and challenges in aggressive debridement [27]. Smaller arthroscopes are being developed for in-office wrist examinations without anesthesia [28•]. 7-T MRIs are improving wrist MRI quality, offering superior imaging of tendons, ligaments, and nerves compared to 3T MRI [29].
Conclusion: A Systematic Approach to Ulnar Sided Wrist Pain Differential Diagnosis
Ulnar-sided wrist pain is a common and persistent issue. Accurate diagnosis requires detailed history, anatomical knowledge, and systematic physical examination. Narrowing the broad differential diagnosis of ulnar sided wrist pain and utilizing cost-effective diagnostic imaging are essential for minimizing treatment delays and optimizing patient outcomes, particularly for automotive technicians and others at risk due to repetitive wrist use.
Compliance with Ethical Standards
Conflict of Interest
Genoveffa Morway declares that she has no conflicts of interest.
Andrew Miller declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Ulnar-Sided Wrist Pain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
[1] Viegas SF. Distal radioulnar joint anatomy, biomechanics, and instability. J Hand Surg Am. 2017 Jan;42(1):35-45.
[2] Kulshrestha V, Chung KC. Ulnar wrist pain. Hand Clin. 2015 Aug;31(3):427-38.
[3] Shin AY, Weinstein LP. Ulnar-sided wrist pain: evaluation and treatment. J Am Acad Orthop Surg. 2011 Oct;19(10):597-606.
[4] • ᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭᅭ
