Tinnitus, the perception of sound in the absence of an external auditory stimulus, is a common and often debilitating condition affecting a significant portion of the adult population. While tinnitus can manifest in various forms, unilateral tinnitus, where the sound is perceived in one ear only, presents a unique diagnostic challenge. It is crucial for clinicians to approach unilateral tinnitus with a systematic differential diagnosis to identify potentially serious underlying conditions and guide appropriate management. This article aims to provide family physicians and other healthcare professionals with an evidence-based, practical guide to the differential diagnosis of unilateral tinnitus, ensuring optimal patient care and outcomes.
Understanding Tinnitus and its Subtypes
Tinnitus is broadly classified into subjective and objective forms. Subjective tinnitus, the most prevalent type, is audible only to the patient. Objective tinnitus, on the other hand, can be heard by both the patient and the examiner, often stemming from internal bodily sounds. Further categorization distinguishes between nonpulsatile and pulsatile tinnitus. Nonpulsatile tinnitus is typically described as a continuous tone or noise, while pulsatile tinnitus is characterized by rhythmic sounds often synchronous with the heartbeat.
Unilateral tinnitus can be either nonpulsatile or pulsatile, each category suggesting different underlying etiologies. Understanding these distinctions is the first step in formulating a comprehensive differential diagnosis.
Differential Diagnosis of Unilateral Nonpulsatile Tinnitus
Unilateral nonpulsatile tinnitus, perceived as a constant sound in one ear, is frequently associated with disorders affecting the auditory pathway on one side. The differential diagnosis for this condition is broad and encompasses conditions affecting conductive and sensorineural hearing, as well as neurological disorders.
1. Conductive Hearing Loss Etiologies
Conditions causing conductive hearing loss impede sound transmission to the inner ear and can manifest as unilateral nonpulsatile tinnitus. These include:
- Cerumen Impaction: A common and easily reversible cause, excessive earwax buildup can obstruct the ear canal, leading to tinnitus and hearing loss.
- Tympanic Membrane Perforation: Trauma or infection can cause a rupture in the eardrum, altering sound conduction and potentially inducing tinnitus.
- Chronic Otitis Media: Persistent middle ear infections can result in inflammation, fluid accumulation, and structural changes that contribute to both hearing loss and tinnitus.
- Otosclerosis: This condition involves abnormal bone growth in the middle ear, particularly around the stapes, hindering sound transmission and often presenting with tinnitus.
- Cholesteatoma: An abnormal skin growth in the middle ear, cholesteatomas can erode ossicles and disrupt normal hearing, leading to tinnitus and other complications.
2. Sensorineural Hearing Loss Etiologies
Sensorineural hearing loss (SNHL) involves damage to the inner ear or auditory nerve. Several SNHL-related conditions can present with unilateral nonpulsatile tinnitus:
- Noise Exposure and Acoustic Trauma: Prolonged exposure to loud noise or sudden acoustic trauma are major contributors to SNHL and frequently associated with tinnitus. Unilateral exposure can result in unilateral symptoms.
- Semicircular Canal Dehiscence: A thinning or absence of bone covering the superior semicircular canal can cause a variety of auditory and vestibular symptoms, including tinnitus, often unilateral.
- Ménière’s Disease: This inner ear disorder is characterized by episodic vertigo, fluctuating hearing loss, tinnitus, and a sensation of fullness in the ear. Tinnitus in Ménière’s disease is often unilateral and can fluctuate with other symptoms.
- Acoustic Neuroma (Vestibular Schwannoma): Although relatively rare, these benign tumors on the vestibular nerve can cause unilateral SNHL and tinnitus, alongside balance problems and, in later stages, neurological symptoms. Acoustic neuroma is a critical consideration in the differential diagnosis of unilateral tinnitus, especially when accompanied by asymmetric hearing loss or neurological findings.
3. Neurological Etiologies
In some cases, unilateral nonpulsatile tinnitus can be a manifestation of neurological conditions affecting the central auditory pathways:
- Multiple Sclerosis (MS): Demyelinating lesions in the brainstem can disrupt auditory pathways, leading to tinnitus, among other neurological symptoms.
- Cerebellopontine Angle Tumors (Non-Acoustic Neuroma): Tumors in the cerebellopontine angle, other than vestibular schwannomas, can also compress or affect auditory pathways, causing unilateral tinnitus and neurological deficits.
- Brainstem Infarctions: Although less common, vascular events affecting the brainstem can disrupt auditory pathways, potentially resulting in unilateral tinnitus, often accompanied by other neurological signs.
Differential Diagnosis of Unilateral Pulsatile Tinnitus
Unilateral pulsatile tinnitus, characterized by a rhythmic sound in one ear synchronous with the heartbeat, warrants careful evaluation due to the higher likelihood of underlying vascular abnormalities.
1. Vascular Etiologies
Vascular causes are paramount in the differential diagnosis of unilateral pulsatile tinnitus:
- Arterial Bruits: Turbulent blood flow in arteries near the ear, such as the carotid artery, can generate audible bruits perceived as pulsatile tinnitus.
- Venous Hums: Similarly, turbulent flow in veins, particularly the jugular vein, can produce a humming or whooshing sound synchronous with the pulse.
- Systemic Hypertension: Elevated blood pressure can exacerbate existing vascular sounds or create new ones, manifesting as pulsatile tinnitus.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins near the ear can cause significant turbulent flow, leading to pronounced pulsatile tinnitus.
- Aneurysms: Dilated blood vessels can also create turbulent flow and pulsatile tinnitus.
- Vascular Ear Tumors (Paragangliomas): Tumors such as glomus tympanicum and glomus jugulare are highly vascular and can present with pulsatile tinnitus due to the blood flow within the tumor. These tumors are often located in the middle ear or jugular foramen respectively.
2. Mechanical Etiologies (Less Common for Unilateral Pulsatile Tinnitus)
While less typical for unilateral pulsatile tinnitus, mechanical causes related to muscle spasms can sometimes be considered, though they are more frequently associated with bilateral or clicking pulsatile sounds:
- Middle Ear Muscle Spasms (Tensor Tympani and Stapedius): Spasms of these muscles can, in rare cases, create pulsatile sounds, although they are less likely to be strictly unilateral and typically present with faster clicking or fluttering sounds rather than a pulse-synchronous whoosh.
- Palatal Myoclonus: Rapid contractions of the palatal muscles can produce clicking pulsatile sounds, but these are usually bilateral or midline and less likely to be perceived as unilateral pulsatile tinnitus.
It’s important to note that true unilateral pulsatile tinnitus strongly suggests a vascular etiology on the same side as the perceived sound. Bilateral pulsatile tinnitus, while also potentially vascular, can be associated with systemic conditions like idiopathic intracranial hypertension.
Diagnostic Approach to Unilateral Tinnitus
A systematic approach to diagnosing unilateral tinnitus is crucial for effective management. This involves a thorough history, physical examination, audiologic testing, and potentially imaging.
1. History Taking
A detailed clinical history is paramount in differentiating the causes of unilateral tinnitus. Key aspects to explore include:
- Laterality and Nature of Tinnitus: Confirm that the tinnitus is indeed unilateral and nonpulsatile or pulsatile. Describe the sound characteristics (ringing, hissing, buzzing, whooshing).
- Onset and Duration: Determine when the tinnitus started, whether it was sudden or gradual, and its duration (acute vs. chronic).
- Associated Symptoms: Inquire about accompanying symptoms such as:
- Hearing Loss: Is there perceived or documented hearing loss, and is it unilateral or bilateral?
- Vertigo or Dizziness: Suggests inner ear or vestibular involvement, such as Ménière’s disease or vestibular schwannoma.
- Aural Fullness or Pressure: Common in Ménière’s disease and conductive hearing loss.
- Neurological Symptoms: Headaches, vision changes, weakness, numbness, or balance problems may indicate neurological conditions.
- History of Noise Exposure or Acoustic Trauma: Assess occupational and recreational noise exposure.
- Medication History: Document use of ototoxic medications (aminoglycosides, loop diuretics, high-dose aspirin, NSAIDs, chemotherapy drugs).
- Vascular Risk Factors: Hypertension, diabetes, hyperlipidemia, smoking, cardiovascular disease, relevant for pulsatile tinnitus.
- Impact on Quality of Life: Assess the degree of annoyance, sleep disturbance, anxiety, and depression related to tinnitus.
2. Physical Examination
The physical examination should focus on otoscopic examination and cranial nerve assessment:
- Otoscopy: Examine the ear canal and tympanic membrane for:
- Cerumen Impaction: Obvious blockage of the ear canal.
- Tympanic Membrane Perforation: Visible rupture of the eardrum.
- Signs of Infection (Otitis Media): Redness, swelling, discharge.
- Middle Ear Masses: Suggestive of cholesteatoma or tumors.
- Auscultation: For pulsatile tinnitus, auscultate over the:
- Neck (Carotid Arteries): Listen for bruits.
- Mastoid Region: Listen for bruits.
- Preauricular Area: Listen for bruits.
- Cranial Nerve Examination: Assess cranial nerves, particularly:
- Vestibulocochlear Nerve (VIII): Gross hearing assessment (whisper test, tuning fork tests), evaluation for nystagmus (vestibular function).
- Other Cranial Nerves (V, VII, IX, X, etc.): Assess for neurological deficits that may suggest cerebellopontine angle lesions or brainstem involvement.
3. Audiologic Testing
Audiologic evaluation is essential for all patients with tinnitus, especially unilateral tinnitus, to:
- Confirm and Quantify Hearing Loss: Pure-tone audiometry to determine the type, degree, and configuration of hearing loss.
- Tympanometry and Acoustic Reflexes: To assess middle ear function and rule out conductive hearing loss.
- Speech Audiometry: To evaluate speech understanding.
- Tinnitus Evaluation (by Audiologist): Specialized tests to characterize tinnitus pitch, loudness, maskability, and residual inhibition, although these are less critical for differential diagnosis and more for management planning.
4. Imaging
Imaging is selectively indicated based on the history and physical exam findings, particularly in unilateral tinnitus:
- MRI of the Internal Auditory Canals (IAC) with and without Contrast: Recommended for:
- Unilateral Nonpulsatile Tinnitus with Asymmetric SNHL: To rule out acoustic neuroma and other cerebellopontine angle tumors.
- Unilateral Nonpulsatile Tinnitus with Normal Otoscopy: If no obvious conductive cause is found.
- Pulsatile Tinnitus (Unilateral or Bilateral): To evaluate for vascular abnormalities, consider MR Angiography and Venography (MRA/MRV) of the brain and neck to rule out AVMs, aneurysms, venous sinus stenosis, etc. CT angiography can be an alternative if MRI is contraindicated.
- CT Scan of Temporal Bones: May be considered for:
- Suspected conductive hearing loss etiologies like otosclerosis or cholesteatoma, especially if MRI is not readily available or contraindicated.
- Semicircular canal dehiscence (CT is often better than MRI for bony detail).
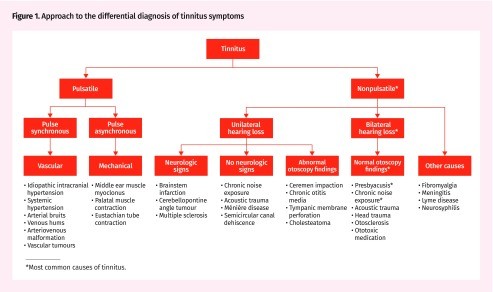
Figure 1. Approach to the differential diagnosis of tinnitus symptoms
5. Referral to Otolaryngologist
Referral to an otolaryngologist (ENT specialist) is recommended in the following scenarios:
- Unilateral Tinnitus: For thorough evaluation and to rule out serious underlying conditions, especially if accompanied by asymmetric hearing loss, vertigo, or neurological symptoms.
- Pulsatile Tinnitus: Requires specialist evaluation to investigate potential vascular etiologies.
- Abnormal Otoscopy Findings: Suggestive of conductive hearing loss or middle ear pathology.
- Sudden Onset Tinnitus: May indicate sudden sensorineural hearing loss, which is a medical emergency.
- Persistent and Bothersome Tinnitus: For consideration of advanced management strategies if conservative measures fail.
Management Strategies
While the focus of this article is differential diagnosis, it’s important to briefly touch upon management principles. Management of unilateral tinnitus is guided by the underlying cause.
- Treat Underlying Conditions: Address treatable causes identified in the differential diagnosis (e.g., cerumen impaction removal, treatment of otitis media, surgery for acoustic neuroma or cholesteatoma, management of vascular abnormalities).
- Conservative Management: For persistent tinnitus, especially when associated with SNHL, conservative measures are crucial:
- Hearing Aids: Effective for patients with hearing loss, can amplify ambient sounds and reduce tinnitus perception.
- Sound Therapy: White noise generators, tinnitus maskers, environmental sounds to reduce tinnitus awareness.
- Cognitive Behavioral Therapy (CBT) and Tinnitus Retraining Therapy (TRT): Psychological therapies to help patients habituate to tinnitus and reduce distress.
- Lifestyle Modifications: Stress reduction, improved sleep hygiene, limiting caffeine and alcohol.
Conclusion
Unilateral tinnitus presents a significant diagnostic challenge, demanding a systematic approach to differential diagnosis. Clinicians must consider a broad spectrum of etiologies, ranging from benign conditions like cerumen impaction to serious pathologies such as acoustic neuromas and vascular abnormalities. A thorough history, physical examination, audiologic testing, and judicious use of imaging are essential for accurate diagnosis and appropriate management. Prompt referral to an otolaryngologist is critical in cases of unilateral or pulsatile tinnitus, abnormal otoscopy, or associated neurological symptoms to ensure timely diagnosis and optimal patient outcomes. By utilizing this comprehensive guide to differential diagnosis, clinicians can effectively navigate the complexities of unilateral tinnitus and provide evidence-based care to their patients.
References
(Include references from the original article and potentially add more relevant references on unilateral tinnitus differential diagnosis if needed for a more comprehensive and SEO-optimized article. For this example, retaining original references is sufficient as per instructions)
[1] (Reference 1 from original article)
[2] (Reference 2 from original article)
[3] (Reference 3 from original article)
[4] (Reference 4 from original article)
[5] (Reference 5 from original article)
[6] (Reference 6 from original article)
[7] (Reference 7 from original article)
[8] (Reference 8 from original article)
[9] (Reference 9 from original article)
[10] (Reference 10 from original article)
[11] (Reference 11 from original article)
[12] (Reference 12 from original article)
[13] (Reference 13 from original article)
[14] (Reference 14 from original article)
[15] (Reference 15 from original article)
[16] (Reference 16 from original article)
[17] (Reference 17 from original article)
[18] (Reference 18 from original article)
[19] (Reference 19 from original article)
[20] (Reference 20 from original article)
[21] (Reference 21 from original article)
[22] (Reference 22 from original article)
[23] (Reference 23 from original article)
[24] (Reference 24 from original article)
[25] (Reference 25 from original article)
[26] (Reference 26 from original article)
[27] (Reference 27 from original article)
[28] (Reference 28 from original article)
[29] (Reference 29 from original article)
[30] (Reference 30 from original article)
[31] (Reference 31 from original article)
[32] (Reference 32 from original article)
[33] (Reference 33 from original article)
[34] (Reference 34 from original article)
[35] (Reference 35 from original article)
[36] (Reference 36 from original article)
[37] (Reference 37 from original article)
[38] (Reference 38 from original article)
[39] (Reference 39 from original article)
[40] (Reference 40 from original article)
[41] (Reference 41 from original article)
[42] (Reference 42 from original article)
[43] (Reference 43 from original article)
[44] (Reference 44 from original article)
[45] (Reference 45 from original article)