Vulvar intraepithelial neoplasia, commonly known as VIN, is a condition characterized by the development of abnormal cells on the surface of the vulva. It’s crucial to understand that VIN is not vulval cancer, but rather a precancerous condition. This means that while it’s not cancer, it has the potential to develop into cancer over time if left unaddressed. The progression to cancer, however, typically occurs over many years, offering a window for diagnosis and intervention.
While some medical professionals might refer to VIN as a pre-cancerous condition, it’s important to note that many women diagnosed with VIN will not ultimately develop vulval cancer. The medical terminology for VIN is vulvar intraepithelial neoplasia.
Understanding the Causes of VIN
The exact causes of VIN are not definitively known by medical experts. However, several risk factors have been identified that can increase a woman’s likelihood of developing this condition. It’s important to remember that having one or more of these risk factors doesn’t guarantee the development of VIN, but it does elevate the risk.
Key risk factors associated with VIN include:
- Human Papilloma Virus (HPV) Infection: HPV is a very common sexually transmitted infection, and certain types are strongly linked to VIN.
- Smoking: Smoking is associated with a range of health issues, including an increased risk of VIN.
- Compromised Immune System: Conditions that weaken the immune system, such as HIV, can increase susceptibility to VIN.
- Chronic Skin Conditions: Long-term vulval skin problems like lichen sclerosus are also considered risk factors for VIN.
Types of VIN: Classical and Differentiated
VIN is broadly classified into two primary types, each with distinct characteristics and implications for VIN diagnosis and management:
- Usual or Classical VIN: This is the more prevalent type of VIN. It encompasses subtypes previously known as VIN 1, VIN 2, and VIN 3, which are now categorized as low-grade squamous intraepithelial lesions (LSIL) and high-grade squamous intraepithelial lesions (HSIL).
- Differentiated VIN (dVIN): Differentiated VIN is less common and presents with different risk factors and a potentially higher risk of progression to cancer compared to classical VIN.
Usual or Classical VIN: LSIL and HSIL Explained
Usual VIN, the most frequently diagnosed type, is further categorized into:
- Low-grade Squamous Intraepithelial Lesion (LSIL): Formerly known as VIN 1, LSIL indicates less significant changes in the vulval skin cells.
- High-grade Squamous Intraepithelial Lesion (HSIL): Previously referred to as VIN 2 and VIN 3, HSIL signifies more pronounced abnormal changes with a higher risk of progression.
The terms LSIL and HSIL are crucial in VIN diagnosis as they describe the extent of abnormal cell involvement within the skin’s surface layer. If these abnormal cells penetrate the basement membrane and invade deeper tissues, the condition is then classified as vulval cancer, highlighting the importance of early VIN diagnosis and management.
Usual or classical VIN is strongly associated with infections caused by the human papilloma virus (HPV).
Low Grade Squamous Intraepithelial Lesion (LSIL) in Detail
LSIL, or VIN 1 as it was formerly known, is typically linked to low-risk types of HPV. These HPV types are also responsible for causing genital warts. LSIL lesions are generally not cancerous and often resolve spontaneously without requiring treatment. However, regular follow-up appointments are recommended to monitor LSIL and ensure it is improving.
High Grade Squamous Intraepithelial Lesion (HSIL) – Understanding the Risks
HSIL, encompassing VIN 2 and VIN 3 in previous classifications, is primarily caused by high-risk types of HPV. Due to a higher risk of progressing to cancer over time, HSIL typically requires treatment. Common treatment approaches include surgical removal of the affected tissue or topical creams. Early VIN diagnosis and treatment of HSIL are essential to prevent potential progression.
Differentiated VIN (dVIN): A Less Common Type
Differentiated VIN (dVIN) is a less common variant of VIN, often diagnosed in older women compared to LSIL and HSIL. The average age at diagnosis for dVIN is around 68 years. Unlike usual VIN, dVIN is not associated with HPV infection. It is frequently observed in women with lichen sclerosus, a chronic inflammatory skin condition affecting the vulva, characterized by itchy, white patches.
Differentiated VIN carries a higher risk of developing into vulval cancer compared to HSIL. Consequently, surgical intervention is generally recommended for dVIN to prevent cancer development, underscoring the importance of accurate VIN diagnosis and proactive management.
Recognizing Symptoms of VIN
Symptoms associated with VIN can vary significantly among individuals. Some women with VIN may experience no noticeable symptoms at all. However, others may develop symptoms such as:
- Persistent Itching (Pruritus): Itching in the vulval area is a common symptom.
- Pain or Soreness: Vulval pain or discomfort can occur.
- Changes in Vulval Skin Appearance: This can include color changes, thickening, or the presence of lumps or lesions.
- Discomfort or Pain During Sexual Intercourse (Dyspareunia): Pain during sex may be experienced.
It’s crucial to recognize that these symptoms are not exclusive to VIN and can be indicative of other conditions. Therefore, if you experience any of these symptoms, it’s essential to consult your General Practitioner (GP) for proper evaluation and VIN diagnosis if necessary.
VIN Diagnosis: Tests and Procedures
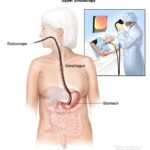
If you present with symptoms suggestive of VIN, your GP may refer you to a specialist, typically a gynecologist or a dermatologist specializing in skin conditions, for further evaluation. The specialist will conduct an examination in a private setting, usually within an outpatient clinic.
The definitive method for VIN diagnosis is a biopsy. This involves taking a small tissue sample from the affected vulval area for microscopic examination. The biopsy procedure may be performed during the initial consultation or scheduled for a later date. Prior to the biopsy, a local anesthetic is administered to numb the vulval area, minimizing discomfort.
The results of the biopsy are typically available within approximately two weeks, requiring a follow-up appointment at the clinic to discuss the findings and determine the appropriate course of action based on the VIN diagnosis.
VIN Treatment Options: Tailoring the Approach
The treatment strategy for VIN is individualized and depends on several factors, including:
- Location of VIN: The specific area of the vulva affected.
- Severity of Symptoms: The intensity and impact of symptoms experienced.
- Risk of Cancer Development: The assessed likelihood of VIN progressing to vulval cancer.
For low-grade squamous intraepithelial lesion (LSIL) or VIN 1, a strategy of monitoring may be recommended initially, rather than immediate treatment.
However, treatment is typically advised for high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN due to their higher risk profiles. Treatment modalities include:
- Surgical Excision: Surgical removal of the VIN-affected skin.
- Imiquimod Cream: Topical application of imiquimod cream to stimulate the immune system to target abnormal cells.
- Laser Treatment: Laser ablation to destroy abnormal cells, although less commonly used.
Monitoring and Follow-up for LSIL
For LSIL, given the low risk of cancer development, close monitoring and regular follow-up may be preferred over immediate treatment, particularly if symptoms are minimal. Regular check-ups allow for timely intervention if there are any signs of changes or progression of the VIN.
Surgical Treatment for VIN: Wide Local Excision and Skinning Vulvectomy
Surgical treatment for VIN typically involves removing the affected skin. Wide local excision is a common procedure where the VIN lesion and a margin of surrounding healthy skin are surgically removed. In cases of widespread VIN, a more extensive procedure called skinning vulvectomy may be necessary.
Imiquimod Cream: Immune System Stimulation
Imiquimod cream is a topical treatment that works by activating the body’s immune system to target and eliminate HPV and VIN-affected cells. The cream is usually applied to the affected area once a week initially, gradually increasing to three times per week, and treatment duration can range from 3 to 4 months. Common side effects of imiquimod cream include inflammation of the vulval skin, potentially causing redness, soreness, itching, weeping, peeling, or cracking.
Laser Treatment for VIN: Laser Ablation
Laser treatment, or laser ablation, is a less frequently used option that involves using a laser to destroy abnormal VIN cells. Typically, only a single treatment session is required. Potential side effects of laser treatment can include hair loss in the vulval area and changes in skin color.
Vulval Care and Follow-up After VIN Diagnosis
Following VIN treatment, symptoms usually improve. Your healthcare provider will provide guidance on proper vulval skin care to manage sensitivity and promote healing.
Regular follow-up appointments at the hospital are crucial after VIN diagnosis and treatment. Initially, these appointments are scheduled every few months, gradually becoming less frequent if the condition remains stable. During follow-up, the vulva is examined to monitor for any signs of VIN recurrence. Long-term follow-up, often spanning several years, is recommended due to the potential for VIN to recur even after successful treatment. Self-examination of the vulva may also be advised as part of ongoing monitoring. It’s important to promptly report any new symptoms or concerns to your healthcare provider between scheduled appointments.
Coping with a VIN Diagnosis
Receiving a VIN diagnosis can be emotionally challenging. The diagnostic tests and treatments can be physically and emotionally uncomfortable. Your GP and specialist will strive to ensure your comfort throughout the process. You have the option to request a chaperone to be present during examinations or procedures, providing additional support. A chaperone can be a friend, family member, or a trained healthcare professional.