Navigating the complexities of medical consent, especially for children under the care of Child Protective Services (CPS), can be challenging. In Texas, specific laws are in place to ensure that children in DFPS (Department of Family and Protective Services) conservatorship have a designated medical consenter. This guide aims to clarify the process of medical consent, informed consent, and the crucial role of backup child care providers and medical consenters in making health decisions. It’s important to understand these procedures to provide the best possible care and advocate effectively for the children involved, ensuring appropriate medical advice and diagnosis are considered in every decision.
Decoding Medical Consent
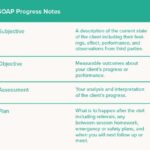
Medical consent, at its core, is the act of deciding whether to approve or reject a proposed medical intervention. This encompasses a wide range of healthcare actions, from agreeing to a simple medical test to authorizing a complex treatment, procedure, or even the prescription of medication. For children in DFPS conservatorship, this decision-making power is entrusted to a designated medical consenter, ensuring that someone is legally responsible for overseeing their healthcare needs and acting in their best interest.
The Cornerstone of Informed Consent
Simply granting consent isn’t enough; the process must be rooted in “informed consent.” This principle mandates that the medical consenter receives comprehensive information about the recommended medical care before making any decisions. The fundamental objective of informed consent is to empower the consenter to make the most appropriate and well-considered choices concerning the child’s health. This process is vital for anyone involved in backup child care or as a primary caregiver, as it ensures they are fully equipped to understand and respond to medical advice and diagnosis.
To ensure informed consent, a medical consenter must confirm their understanding of several key aspects before authorizing healthcare:
- The Child’s Condition: A clear understanding of the child’s symptoms and the specific medical diagnosis is paramount. Without grasping the nature of the health issue, it’s impossible to make an informed decision about treatment.
- Treatment Benefits: The consenter needs to know precisely how the proposed treatment is expected to alleviate the condition and improve the child’s health. This involves understanding the intended positive outcomes of the medical intervention.
- Consequences of No Treatment: It’s equally crucial to comprehend what might happen if the recommended treatment is not pursued. This knowledge helps weigh the risks and benefits of intervention versus non-intervention.
- Treatment Risks and Side Effects: Every medical treatment carries potential risks and side effects. The medical consenter must be fully informed about these possibilities to make a balanced judgment about whether the benefits of treatment outweigh the potential harms.
Informed Consent and Psychotropic Medications
The process of informed consent becomes even more critical when considering psychotropic medications, particularly for children in foster care who may have experienced trauma or have complex emotional and behavioral needs. Texas law sets specific requirements for consent related to these powerful medications to protect children and ensure responsible prescribing practices.
Consent for psychotropic medication is legally valid only if it meets stringent criteria:
- Voluntary and Free of Coercion: The consent must be given willingly, without any pressure or undue influence from healthcare providers, caseworkers, or other parties. The decision should be made freely by the medical consenter.
- Comprehensive Information Disclosure: The medical consenter must receive detailed information, either verbally or in writing, covering the following critical points:
- Specific Condition for Treatment: A precise diagnosis of the condition that the psychotropic medication is intended to treat.
- Expected Benefits: A clear explanation of the positive effects the medication is expected to have on the child’s diagnosed condition.
- Consequences of Not Consenting: Information about the potential health and mental health outcomes if the medication is not administered.
- Probable Side Effects and Risks: A thorough discussion of the clinically significant side effects and potential risks associated with the medication.
- Alternative Treatments: Information about generally accepted alternative medications and non-pharmacological interventions (like therapy or behavioral strategies), if such alternatives exist.
- Rationale for Proposed Treatment: A clear explanation of the reasons behind recommending psychotropic medication as the chosen course of treatment.
When a new psychotropic medication is being considered, Texas DFPS Form 4526, titled “Psychotropic Medication Treatment Consent,” must be completed and signed by both the medical consenter and the prescribing healthcare provider (or their designee). This form formalizes the informed consent process specifically for new psychotropic medications. During this process, the medical consenter should actively discuss non-pharmacological alternatives with the provider and ask any questions they have to fully understand the elements of informed consent. This detailed discussion is required at both the initial appointment and all follow-up appointments to ensure ongoing informed decision-making. Understanding these requirements is vital for anyone in a backup child care role, as they may be involved in these critical discussions and decisions.
The Selection of a Medical Consenter
The court overseeing a child’s case will designate who will serve as the medical consenter. This can be either an individual or DFPS itself.
-
Individual Medical Consenter: The court may appoint an individual, often a relative or someone else deeply involved in the child’s life, to be the medical consenter. When an individual is appointed, they bear the ultimate responsibility for making medical decisions for the child and are accountable directly to the court for those decisions.
-
DFPS as Medical Consenter: In many cases, the court grants DFPS the authority to consent to medical care. When this occurs, DFPS selects up to four medical consenters, including primary and backup medical consenters. Typically, the primary consenters are the child’s live-in caregivers (such as foster parents or relatives) or the child’s caseworker along with another CPS staff member. Backup medical consenters are crucial for ensuring continuity of care, especially in situations where primary consenters are unavailable. DFPS can choose the following as medical consenters or backup medical consenters:
- Foster parents.
- Relatives providing kinship care.
- CPS caseworkers, supervisors, or other CPS personnel.
However, DFPS is legally restricted from appointing certain individuals as medical consenters or backup medical consenters:
- Employees of staffed facilities, such as residential treatment centers or intermediate care facilities for individuals with developmental disabilities. Similarly, HCS (Home and Community-based Services) caregivers cannot serve as medical consenters. In these situations, CPS caseworkers are typically designated.
DFPS formally appoints medical consenters and backup medical consenters by issuing Form 2085-B (Designation of Medical Consenter). This form is provided to the designated consenter and other caregivers when the child is placed in their care. Form 2085-B contains essential information regarding medical care and the STAR Health program (Texas’ managed care program for children in foster care, Medicaid, and CHIP). Medical consenters and backup consenters are required to provide copies of Form 2085-B to each child’s doctors and other healthcare providers to demonstrate their legal authority to consent. Form 2085-B also includes contact information for CPS supervisors and the court, facilitating communication if healthcare providers encounter any issues or concerns regarding a medical consenter’s decisions.
DFPS retains the authority to change a child’s medical consenter or backup medical consenter for various reasons. This is done by issuing a new Form 2085-B and notifying the court of the change.
In specific circumstances, a court may empower a youth aged 16 or 17 to act as their own medical consenter, provided they meet certain legal requirements.
- Attorneys ad litem (lawyers appointed to represent the child’s best interests) and DFPS staff are legally obligated to inform 16 and 17-year-olds in foster care about their right to petition the court for the authority to consent to their own medical care.
- This request can be made at any court hearing after the youth’s 16th birthday. The court then decides whether the youth can consent to all, some, or none of their medical care.
- When a court grants a youth the authority to make their own medical decisions, DFPS staff, the youth, and the youth’s caregivers will receive a copy of the official court order documenting this decision.
Essential Training for Medical Consenters
To ensure they are adequately prepared for their responsibilities, all medical consenters and backup medical consenters, regardless of whether they are appointed by the court or DFPS, must complete DFPS Medical Consent Training for Caregivers. This mandatory training is accessible on the DFPS Intranet for DFPS staff and on the DFPS Public Website for all other medical consenters and backups. Initial completion of this training is a prerequisite for being named a medical consenter, and annual refresher training is also required to maintain this designation. The training resources are available in both English and Spanish to ensure accessibility for all.
Specialized Training for Psychotropic Medication Consent
Medical consenters and caregivers responsible for children who may be prescribed psychotropic medications must complete a more specialized training program: “Psychotropic Medication for Children in Foster Care.” Upon successful completion of this training, which includes passing a post-test, consenters must provide documentation of completion to the child’s caseworker. This specialized training is also required annually to ensure consenters remain up-to-date on best practices and relevant guidelines. This training, like the general medical consent training, is available in both English and Spanish.
Medical Consent Training for Youth
Recognizing the increasing autonomy of older youth, DFPS provides specific medical consent training tailored for youth.
Youth who are authorized by the court to be their own medical consenters must complete DFPS Medical Consent Training for Caregivers within seven days of the court order granting them this authority. If the youth has a scheduled medical or behavioral health appointment before this seven-day deadline, the training must be completed at least 48 hours prior to the appointment. This expedited timeline ensures youth are prepared to make informed decisions about their healthcare promptly. Training is not required before emergency medical appointments.
Furthermore, if a youth authorized to consent for themselves is taking or considering psychotropic medication, they must also complete the “Psychotropic Medication for Children in Texas Foster Care” training within seven days of the court order. Similar to the general medical consent training for youth, if there is a scheduled medical or behavioral health appointment before the seven-day training deadline, the psychotropic medication training must be completed at least 48 hours before the appointment, except in emergency situations. Documentation of youth training completion must be sent to the caseworker within 5 days.
Support and Guidance for Youth Acting as Their Own Medical Consenter
Even when youth are empowered to make their own medical decisions, they are not alone. The youth’s caseworker and caregivers are legally obligated to assist them in obtaining comprehensive information about any medical conditions, tests, treatments, and medications. They must also provide ongoing support to help youth make well-informed healthcare decisions. This collaborative approach ensures that youth have the resources and guidance they need to navigate complex medical choices responsibly.
However, there are safeguards in place. If a youth’s healthcare decision poses a significant risk of harm, the court retains the authority to overrule the youth’s decision, even after authorizing them to make medical decisions. To do so, the court must find clear and convincing evidence that the medical care is in the youth’s best interest and that one of the following conditions is met:
- The youth lacks the capacity to make an informed decision.
- Failure to receive medical care will result in observable and substantial impairment of the youth’s growth, development, or overall functioning.
- The youth is at risk of causing substantial bodily harm to themselves or others.
In these situations, DFPS may file a motion requesting the court to mandate specific medical treatment or to authorize DFPS to consent to medical care on the youth’s behalf. Any such motion must include a detailed explanation of the youth’s reasons for refusing medical care and a statement from a physician explaining why the medical care is deemed necessary.
Understanding the intricacies of medical consent, particularly within the foster care system, is essential for everyone involved in providing care and support to these vulnerable children. From backup child care providers to caseworkers and medical professionals, a clear grasp of these procedures ensures that children receive the necessary medical attention while their rights and best interests are protected.