Introduction
Patients with neurological impairments admitted to the Intensive Care Unit (ICU), often referred to as neurocritical patients (Delaney et al., 2018), require specialized and vigilant care from a multidisciplinary healthcare team. This heightened level of attention within the hospital setting is crucial to prevent further complications and secondary injuries. The nursing team plays a pivotal role in delivering this specialized care in the ICU, utilizing the systematization of nursing care as a vital framework (de Arruda et al., 2019; Unal et al., 2021). This review delves into the essential nursing diagnoses and management strategies for neurocritical patients, aiming to provide a comprehensive overview for practitioners in this demanding field.
Neurocritical patients encompass individuals experiencing a range of severe neurological conditions, including ischemic and hemorrhagic stroke (cerebrovascular accident), traumatic brain injury, hydrocephalus, brain tumors, aneurysms, and subarachnoid hemorrhage, either upon ICU admission or during their stay. These patients often present with or develop critical complications such as elevated intracranial pressure (ICP), intracranial hypertension, and intracranial hemorrhage (Wang et al., 2018). The complexity of these conditions necessitates intensive care and continuous monitoring, making the ICU the optimal environment for their management. The ICU setting allows for the application of advanced technological monitoring and facilitates rapid decision-making by healthcare professionals, ultimately contributing to improved patient prognosis (da Silva et al., 2020).
Within the neurocritical care paradigm, nursing assumes a central role due to the constant presence of nurses throughout the patient’s treatment and recovery journey. Nurses are instrumental in the early detection and prevention of potential complications. Their actions are guided by evidence-based practices focused on maintaining adequate cerebral perfusion, promptly recognizing signs of elevated or decompensated ICP, and conducting thorough neurological assessments using tools like the Glasgow Coma Scale (GCS; Barcelos et al., 2016; Delaney et al., 2018). Effective nursing care, grounded in a systematic approach, significantly influences patient outcomes and clinical improvement.
Essential nursing interventions encompass a wide spectrum of measures, including continuous hemodynamic and respiratory monitoring, meticulous patient positioning, vigilant vital sign assessment, and diligent oral hygiene and endotracheal suctioning. These practices are fundamental in ensuring patient safety and optimizing care delivery. Therefore, meticulously planned nursing care is indispensable for the effective management of neurocritical patients (Deldar et al., 2020). The nursing process itself serves as a structured framework, enabling nurses to provide targeted and patient-centered care that directly addresses individual needs (Barcelos et al., 2016). Furthermore, standardized protocols are crucial for streamlining care planning, implementation, and evaluation, promoting consistency and best practices in neurocritical care (Buterakos et al., 2022).
This review underscores the critical role of evidence-based practice and the existing literature in guiding nursing care for neurocritical patients. By examining current research, we aim to provide nurses with practical care plans tailored for this complex patient population. This study is motivated by the ongoing need for resources that effectively guide nurses in delivering optimal neurocritical care. Specifically, it identifies key nursing diagnoses (NDs) as defined by the North American Nursing Diagnosis Association International (NANDA-I; NANDA I 2021–2023, 2022) and associated nursing care strategies. Given the evolving landscape of healthcare, particularly in the post-pandemic era, an updated review of neurocritical care is essential. The COVID-19 pandemic has introduced new dimensions to patient care, making a contemporary analysis of nursing diagnoses and management in neurocritical patients particularly relevant. Thus, this study aims to identify prevalent nursing diagnoses and essential nursing care practices for neurocritical patients in the ICU, offering a valuable resource for nurses and contributing to enhanced patient outcomes.
Methodology
This review employed a scoping review methodology, adhering to the Joanna Briggs Institute (JBI) guidelines (JBI, 2020; Lockwood & Tricco, 2020), to synthesize existing knowledge and map key concepts related to the Systematization of Nursing Care for neurocritical patients within the ICU setting. The review followed a structured nine-step process: (1) defining the research question and objectives; (2) establishing eligibility criteria; (3) outlining the planned approach for study searching, selection, data extraction, and evidence presentation; (4) designating the evidence search strategy; (5) selecting evidence; (6) extracting evidence; (7) analyzing the evidence; (8) presenting results; and (9) summarizing evidence in relation to the review objective (Peters et al., 2015).
The research question was formulated using the PCC framework: Population “P” (Neurocritical Patient), Concept “C” (Nursing Care), and Context “C” (ICU; Peters et al., 2015). This framework guided the formulation of the central question: “What are the diagnoses and nursing care strategies for neurocritical patients in the ICU?”
Data collection was conducted in February 2022, utilizing a paired approach across several key databases: Excerpta Medica DataBASE (EMBASE), MEDLINE (via Online System of Search and Analysis of Medical Literature), PubMed (Medline US National Library of Medicine National Institutes of Health), and SCOPUS. The search strategy employed controlled descriptors combined with Boolean operators (AND, OR) to ensure comprehensive retrieval of relevant studies. The specific search string used was: “Neurology” AND “Nursing Care” OR “Nursing Diagnosis” AND “Critical Care.”
Study selection criteria included original research articles available in full text, online, and without charge. The review focused on articles published in English, Spanish, or Portuguese, within a timeframe of 2017 to 2022. This period was chosen to capture recent advancements in neurocritical patient care protocols and the emergence of new care techniques influenced by the COVID-19 pandemic. Exclusion criteria encompassed duplicate articles, review articles, and abstracts.
Retrieved studies were imported into the Reyyan Intelligent Systematic Review system (rayyan.ai) for efficient screening (Ouzzani et al., 2016). Study selection was performed independently by two reviewers (M.L.P.B. and L.F.R.M) in a blinded manner (JBI, 2020) across two stages. The initial stage involved screening titles and abstracts, followed by a full-text review of potentially eligible studies based on the pre-defined inclusion criteria.
Following the double-blind screening process, a significant proportion of articles (91%) were excluded, 6% showed interreviewer disagreement, and 3% were included by both reviewers. Disagreements were resolved through consensus discussion, eliminating the need for a third reviewer. The rayyan.ai tool also recorded screening session durations for each reviewer, enhancing process transparency.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Tricco et al., 2018) flowchart was used to visually represent the study identification, screening, eligibility assessment, and inclusion process, as depicted in Figure 1.
Figure 1.
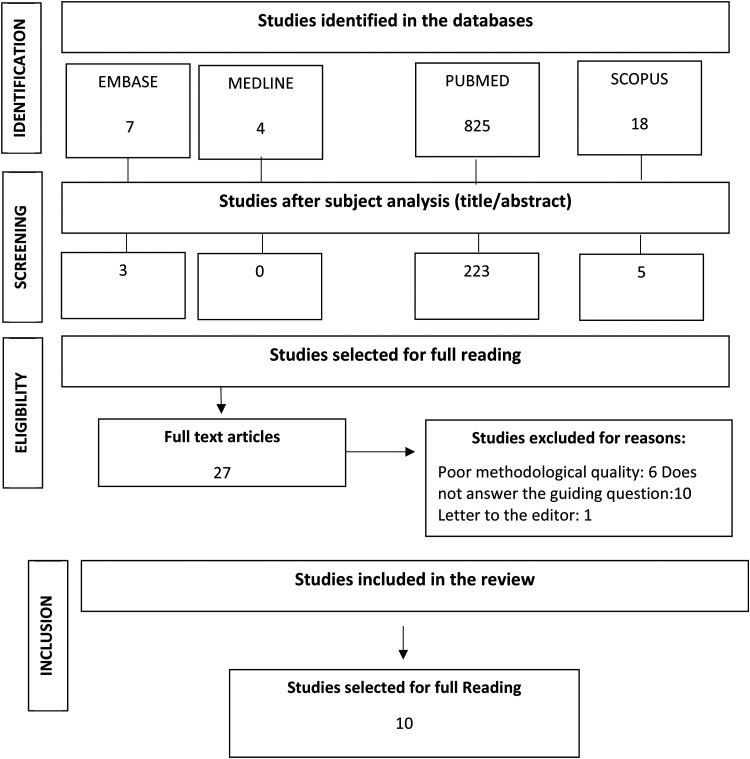 PRISMA Flowchart illustrating the study selection process for this review.
PRISMA Flowchart illustrating the study selection process for this review.
To characterize the selected studies, a custom-designed checklist was utilized, capturing variables such as author(s), publication year, article title, indexing database/journal, study type, study participants, and key findings. Data analysis involved data reduction techniques, including thorough reading and logical structuring of data, systematic comparison of primary study results, and interpretive analysis (Lockwood & Tricco, 2020; Tricco et al., 2018). The findings are presented in Tables 1 and 2 and further discussed in relation to current relevant literature.
Table 1.
Characteristics of Included Scoping Review Studies
| Reference | Journal | Type of study/sample | Objective | Risk of Bias* |
|---|---|---|---|---|
| Ben-Tovim and Theilla (2021) | Intensive and Critical Care Nursing | Descriptive, exploratory study, intentional sampling (n = 45). | Assess ICU nurses’ perceived and real role in nutritional care and knowledge of hypophosphatemia and refeeding syndrome. | 100% |
| Buterakos et al. (2022) | American Journal of Infection Control | Retrospective medical record review (2017-2020). | Evaluate impact of sample collection on diagnosis and VAP bundle implementation on VAP rates. | 100% |
| Deldar et al. (2020) | BMC Medical Education | Quasi-experimental study (n = 70) nurses. | Evaluate effects of two methods on pain diagnosis and management in mechanically ventilated patients. | 100% |
| da Silva et al. (2020) | The Latin American Journal of Nursing | Cohort study (n = 93) patients. | Clinically validate nursing diagnosis “Dysfunctional Response to Ventilatory Weaning” in adult ICU patients. | 100% |
| Biyabanaki et al. (2020) | Indian Journal of Critical Care: Official publication of the Indian Society of Intensive Care Medicine | Cross-sectional study | Explore ICU nurses’ perceptions and practices in delirium assessment and barriers. | 100% |
| Olsen et al. (2020) | Acta Neurochirugica | Consecutive sample of neuro-ICU patients | Compare FOUR score and automated pupillometry to GCS and visual pupil inspection. | 100% |
| Souza et al. (2017) | Revista Gaúcha de Enfermagem | Experience report | Describe nurse training experience implementing a systematic delirium screening tool (CAM-ICU). | 100% |
| Wuni et al. (2020) | Pain Research and Management | Descriptive, cross-sectional study, institutions (n = 180) nurses. | Assess nurses’ knowledge, practices, and barriers in pediatric pain management at Tamale University Hospital, Ghana. | 100% |
| Li et al. (2017) | Medicine | Longitudinal study | Assess FMEA implementation impact on CRBSI incidence in the ICU. | 100% |
| Delaney et al. (2018) | BMJ Open | Prospective observational study (n = 80) adults. | Assess feasibility and accuracy of sleep assessment techniques for widespread ICU sleep monitoring. | 100% |
*Risk of bias assessed using JBI Appraisal Tools. ICU = intensive care unit; GCS = Glasgow Coma Scale; CRBSI = catheter-related bloodstream infection; FMEA = failure mode and effect analysis; VAP = ventilator-associated pneumonia; CAM-ICU = Confusion Assessment Method for the ICU.
Table 2.
NANDA-I Nursing Diagnoses Identified in Reviewed Articles
Methodological quality and risk of bias in the selected studies were assessed by two independent researchers (M.L.P.B. and L.F.R.M) using JBI Appraisal Tools (JBI, 2020). Discrepancies were resolved using tool elements to enhance accuracy and minimize bias. Descriptive analysis was employed, with a summary of each included study.
Results
The initial search identified 854 studies. Following title and abstract screening, 27 articles met eligibility criteria, and after full-text review, 10 studies were included in this review. The primary focus of this review is the presentation of nursing diagnoses and care strategies identified within these ten articles.
Discussion
This scoping review highlights the crucial contributions of nurses in providing specialized care for neurocritical patients. The analysis of current literature provides valuable insights into prevalent nursing diagnoses and essential care practices. However, the limited number of studies specifically addressing this intersection underscores the need for further research in this critical area of healthcare. To enhance clarity and facilitate understanding, the discussion is structured around key themes: primary Nursing Diagnoses (NDs) based on NANDA-I taxonomy (NANDA I 2021–2023, 2022) and associated nursing care management strategies.
Nursing Diagnoses in Neurocritical Care
Nursing diagnoses for neurocritical patients are inherently complex and require a systematic, evidence-based approach, particularly aligning with the NANDA-I taxonomy (NANDA I 2021–2023, 2022). A study by Soares et al. (2019), which examined 184 medical records of neurocritical patients, identified 19 distinct nursing diagnoses. The most frequently observed diagnoses included risk for electrolyte imbalance, decreased intracranial adaptive capacity, risk for ineffective cerebral tissue perfusion, acute confusion, risk for infection, and acute pain. These findings are further corroborated by Souza et al. (2017), whose research also highlighted the prevalence of these specific nursing diagnoses in neurocritical patients.
A cross-sectional study by Franco et al. (2018) involving 219 patients with urgent and emergent clinical needs, identified a slightly different distribution of nursing diagnoses. Ineffective breathing pattern was the most prevalent diagnosis (28.3%), followed by acute pain (22.3%). Other significant diagnoses identified included chronic pain, impaired spontaneous ventilation, impaired gas exchange, ineffective airway clearance, and decreased cardiac output. The presence of these diagnoses in emergency settings underscores their relevance to the neurocritical patient population, particularly in the acute phase of their illness.
Analyzing medical records, Soares et al. (2019) also reported a high prevalence of acute confusion (28%) and risk for acute confusion (100%). This suggests that altered cognitive function is a significant concern in neurocritical patients, potentially linked to underlying infectious conditions, as noted in their study. These findings emphasize the critical role of nurses in the systematic assessment and management of cognitive changes in this patient group.
The research of da Silva et al. (2020) supports the findings of this review, identifying key nursing diagnoses such as risk for decreased cardiac output, anxiety related to perceived threat of death, stress factors, and fear associated with separation from support systems. Disturbances in sleep patterns and sleep deprivation are also prevalent nursing diagnoses in critically ill patients, including those with neurological compromise. These sleep-related issues are associated with increased risks of both physical and psychological complications, necessitating comprehensive care and targeted interventions (Olsen et al., 2020).
Key Nursing Care Management Strategies
Nursing care in the ICU for neurocritical patients demands a patient-centered approach, characterized by comprehensive monitoring and proactive intervention. It is recognized as complex care that necessitates continuous vigilance and plays a vital role in early identification of clinical changes and timely diagnosis (Biyabanaki et al., 2020). Barcelos et al. (2016) affirm the fundamental role of nursing in neurocritical patient management, encompassing treatment and complication prevention. This includes diligent monitoring of vital signs such as respiratory rate, heart rate, blood pressure, and oxygen saturation.
Preventing Ventilator-Associated Pneumonia (VAP), providing meticulous assistance with mechanical ventilation (MV), and managing the ventilator weaning process are crucial aspects of nursing care for neurocritical patients. Regina et al. (2020) highlight the increased risk of complications such as VAP, ventilation-induced diaphragmatic dysfunction, ventilation-induced lung injury, polyneuropathy, tracheostomies, and increased mortality in neurological patients undergoing prolonged MV. Therefore, proactive VAP prevention strategies and expert MV management are paramount in this population.
Assessing sedation levels and consciousness is another critical nursing responsibility. Souza et al. (2017) advocate for the use of the Richmond Agitation and Sedation Scale (RASS) for this purpose. Their study indicated that patients assessed using a standardized tool like RASS had a higher incidence of neurological sequelae (55.9%). This underscores the importance of utilizing validated assessment tools to correlate sedation levels with patient outcomes, potentially contributing to reduced complications and ICU length of stay. The Glasgow Coma Scale (GCS) is also highlighted as an essential tool for promoting evidence-based care. Routine GCS assessment aids in evaluating patient severity and is associated with reductions in MV duration and ICU stay (Ben-Tovim & Theilla, 2021).
The findings of this review align with Souza et al. (2017), emphasizing the importance of GCS assessment in evaluating consciousness levels. Their study reported an average GCS score of four in neurocritical patients, indicating a profile associated with severe physical and neurological consequences during hospitalization. Nursing plays a pivotal role in managing these patients, providing clinical management, hemodynamic stabilization, early detection of neurological changes, and implementing comprehensive care plans (Rodriguez et al., 2016).
Pupillary assessment is another crucial aspect of neurological monitoring performed by nurses. Souza et al. (2017) emphasize pupillometry as a standard procedure in neurocritical care. Routine pupillometric assessments serve as a valuable adjunct to ICP monitoring and can be an early indicator of increasing ICP (Santos et al., 2020). Specific nursing interventions aimed at reducing ICP, such as maintaining the head of the bed elevated to 30 degrees, are essential. The effectiveness of such interventions is supported by Buterakos et al. (2022), whose research indicated a 100% success rate in implementing appropriate nursing interventions for ICP management in critically ill patients.
Comprehensive monitoring and accurate documentation by nursing professionals are crucial for developing well-founded nursing care plans and ensuring continuity of care for neurocritical patients. Detailed and timely records facilitate effective communication among the healthcare team and contribute to optimal patient management.
Implications for Practice
This review provides a valuable resource for nurses involved in the care of critically ill patients, offering essential insights for developing individualized care plans. The findings underscore the need for specialized training and knowledge in neurocritical care for nursing staff. Healthcare institutions should prioritize ongoing education and resource allocation to equip nurses with the necessary competencies to effectively manage this complex patient population.
By utilizing this review as a foundation for practice, nurses can gain enhanced guidance in delivering technical care and deepen their understanding of prevalent nursing diagnoses in neurocritical ICUs. This knowledge empowers nurses to provide more targeted and effective interventions, ultimately contributing to improved patient outcomes and quality of care.
Conclusion
This scoping review successfully identified key nursing care strategies for neurocritical patients, despite the relative scarcity of dedicated literature in this specific area. Descriptive and cross-sectional studies constituted the majority of the reviewed sample, providing essential information for developing a comprehensive understanding of nursing diagnoses and care practices in neurocritical care.
The review highlighted the prevalence of specific nursing diagnoses and their corresponding interventions that are critical for nurses in the ICU setting. It underscores the importance of continuous professional development for nurses, emphasizing the need to stay updated on the nursing process and deliver individualized care tailored to each patient’s unique needs. The review reinforces the existing literature advocating for the essential role of systematized nursing care in achieving satisfactory patient prognoses.
The nursing care strategies identified in this review can be effectively integrated into neurocritical patient care plans, facilitating improved patient outcomes, enhanced quality of life, and overall health promotion. Finally, this work serves as a valuable foundation for future research focused on optimizing quality nursing care for neurocritical patients and further refining best practices in this specialized field.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Luis Fernando Reis Macedo https://orcid.org/0000-0002-3262-9503
References
Asim et al., 2021
Barcelos et al., 2016
Ben-Tovim & Theilla, 2021
Biyabanaki et al., 2020
Buterakos et al., 2022
da Silva et al., 2020
de Arruda et al., 2019
Delaney et al., 2018
Deldar et al., 2020
Franco et al., 2018
JBI, 2020
Li et al., 2017
Lockwood & Tricco, 2020
NANDA I 2021–2023, 2022
Olsen et al., 2020
Ouzzani et al., 2016
Peters et al., 2015
Regina et al., 2020
Rodriguez et al., 2016
Santos et al., 2020
Soares et al., 2019
Souza et al., 2017
Tricco et al., 2018
Unal et al., 2021
Wang et al., 2018
Wuni et al., 2020
